Colorectal Cancer Risk In Ibd
Colorectal cancer risk and IBD
Patients with IBD appear to be at notably increased risk of colorectal cancer compared to the general population , with one recent study demonstrating a 7% colorectal cancer risk after 30 years of disease . Patients with at least 8 years disease duration and colonic involvement are at increased risk of colorectal cancer . Patients at risk of colorectal cancer should be enrolled in a dysplasia surveillance plan as this appears to reduce the risk of colorectal cancer. Surveillance typically includes colonoscopy every 1-3 years, depending on individual patient risk .
Risk factors and surveillance intervals
In patients at high risk, consider ~1 year surveillance intervals. High risk features include: primary sclerosing cholangitis , prior history of dysplasia or colonic strictures, or strong family hx of colorectal cancer . Patients with low to moderate risk may be surveyed every 2-3 years. Moderate risk features include: extensive colitis with moderate inflammatory burden, family hx of CRC in first degree relative > age 50 and possibly extensive inflammatory polyps or pseudopolyps
Surveillance Protocols
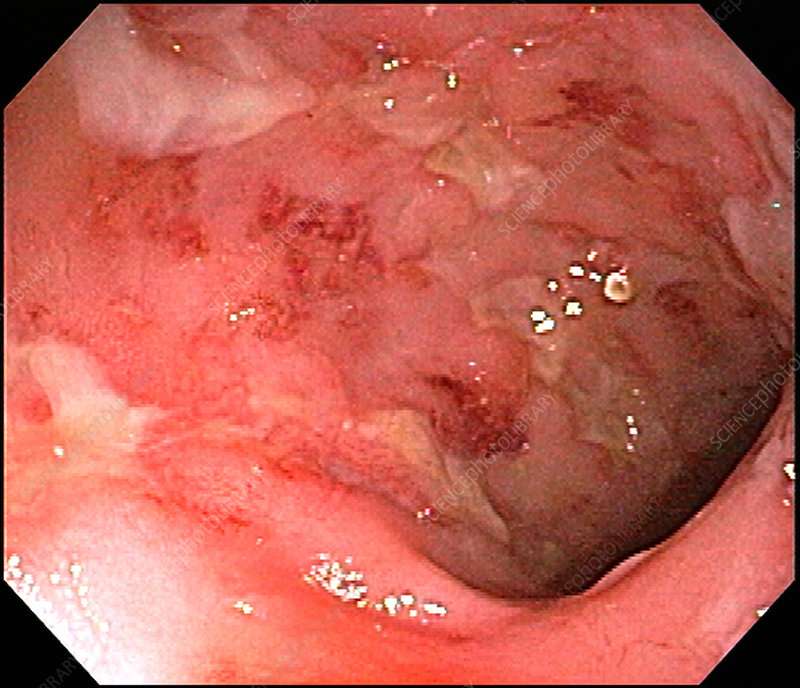
Management of Endoscopic lesions
Any visible polyps or lesions should be endoscopically resected if feasible and the specimen should be sent in a separately labeled jar. If a lesion has indistinct borders or is not amenable to resection, biopsy sample should be taken and sent in a separate jar.
Management of Dysplasia
Crohns & Colitis Uk Local Networks
Our Local Networks of volunteers across the UK organise events and provide opportunities to get to know other people in an informal setting, as well as to get involved with educational, awareness-raising and fundraising activities. You may find just being with other people and realising that you are not alone can be reassuring. Families and relatives may also find it useful to meet other people with Crohn’s or Colitis. All events are open to members of Crohns & Colitis UK.
Previous Treatment For Certain Cancers
Some studies have found that men who survive testicular cancer seem to have a higher rate of colorectal cancer and some other cancers. This might be because of the treatments they have received, such as radiation therapy.
Several studies have suggested that men who had radiation therapy to treat prostate cancer might have a higher risk of rectal cancer because the rectum receives some radiation during treatment. Most of these studies are based on men treated in the 1980s and 1990s, when radiation treatments were less precise than they are today. The effect of more modern radiation methods on rectal cancer risk is not clear, but research continues to be done in this area.
Don’t Miss: Folic Acid And Ulcerative Colitis
How To Reduce Your Risk
Here are a few other things you can do to lower your chances of developing colorectal cancer and improve your odds of finding it early if you develop it:
- Ask your doctor about taking medications such as sulfasalazine , vedolizumab , or mesalamine . These drugs help manage UC, and they may help lower your risk for colorectal cancer.
- Take your medications as your doctor prescribed to keep your UC inflammation well managed.
- See your gastroenterologist for check-ups at least once a year.
- Let your doctor know if any of your family members had colorectal cancer or have recently been diagnosed.
- Eat more fruits, vegetables, and whole grains such as brown rice or wheat bread.
- Limit red meat, such as burgers, steaks, and pork. Also limit processed meats, such as hot dogs, bacon, and sausage. Theyve been linked to colorectal cancer risk.
- Avoid alcohol or limit yourself to no more than one drink a day.
- Try to walk, ride a bike, or do other exercises on most days of the week.
Along with getting regular screenings, look for these symptoms of colorectal cancer and report them to your doctor right away:
- a change in your bowel movements
- blood in your stool
What You Need To Know About Ulcerative Colitis And Colorectal Cancer
Posted by Minnesota Oncology Physicians on October 4, 2021
There is a significant link between ulcerative colitis and colorectal cancer. If you have UC, your risk of developing colorectal cancer is six times greater. And the longer you have had ulcerative colitis, the higher your risk for colon or rectal cancer becomes. Why are these two conditions of the intestines connected?
Recommended Reading: What’s The Difference Between Colitis And Ulcerative Colitis
People With Iron Deficiency Anemia
- Iron deficiency anemia may be a presentation of colorectal cancer. People who present with unexplained iron deficiency anemia should be referred to have a colonoscopy on a prompt basis.
- Stool-based testing should not be used to guide the decision to refer or investigate people with symptoms or other conditions suggestive of colorectal cancer because it may lead to a delay in diagnosis.Reference 6Close referenceNarula N, Ulic D, Al-Dabbagh R, Ibrahim A, Mansour M, Balion C, et al. Fecal occult blood testing as a diagnostic test in symptomatic patients is not useful: A retrospective chart review. Can J Gastroenterol Hepatol. 2014 28: 42126.OpenCloseReference 7Close referencevan Rijn AF, Stroobants AK, Deutekom M, Lauppe C, Sturk A, Bossuyt PMM, et al. Inappropriate use of the faecal occult blood test in a university hospital in the Netherlands. Euro J of Gastroenterol and Hepatol. 2012 24:1266-69.OpenCloseReference 8Close referenceIp S, Sokoro AA, Kaita L, Ruiz C, McIntyre E, Singh H. Use of fecal occult blood testing in hospitalized patients: results of an audit. Can J Gastroenterol Hepatol. 2014 28: 489-94.OpenClose
You May Like: Ulcerative Colitis Worse At Night
Can Ulcerative Colitis Increase Your Risk Of Colon Cancer Find Out
Ulcerative colitis is a condition that causes inflammation in the large intestine, including the colon. Two of the most common effects of this disease are symptoms like abdominal pain and diarrhea. You can also be at an increased risk of colorectal cancer if you have UC.
Duration of Ulcerative Colitis
According to the Crohns & Colitis Foundation, once youve lived with UC for about 8-10 years, your risk for colon cancer typically starts to increase. Your cancer risk is higher if youve had UC for long.
Colorectal cancer rates increase dramatically for people in North America after a person has lived with UC for 30 years, according to a 2019 literature review. In Asia, colorectal cancer rates dramatically increase after a UC duration of about 10-20 years.
Inflammation
Your risk for getting colorectal cancer also depends on how much your colon has inflamed. The highest risk for colorectal cancer has been seen in people with a lot of inflammation in their entire colon.
Primary Sclerosing Cholangitis
If you have this rare complication of UC, you need to be prepared. PSC affects the bile ducts that carry the digestive fluid to the intestine from the liver and causes scarring and inflammation, which narrows the ducts. Youre at higher risk of colorectal cancer, and this disease might start sooner than 8-10 years after youve been diagnosed with UC.
Here are some things you can do to lower your chances of developing colorectal cancer and diagnose it earlier:
You May Like: Ulcerative Colitis Treatment In India
Does Ibd Increase Your Risk For Colon Cancer
Regardless of the type of colitis, this type of sustained inflammation can cause lasting damage to sensitive tissues, causing pain, bloating, bowel issues and bleeding. If left untreated, IBD can create complications like dysplasia, which results in the growth of abnormal cells in the colon or rectum. Over time, these abnormal cells can mutate into cancer.
Your risk of developing colon cancer depends on a few factors, such as the type of inflammatory disease you have, how long youve had it and how much of your large intestine is affected, said Dr. Senatore. Research shows that your cancer risk doesnt increase until youve had IBD for at least eight years.
Does The Occurrence Of Dysplasia Require Confirmation
Our recommendation: The occurrence of dysplasia must be confirmed by a second pathologist.
Histopathological analysis is qualitative and consequently has a high inter-observer variability, especially in low grade dysplasia and in inflamed mucosa. Therefore, there is a general consensus that the occurrence of dysplasia should be confirmed by an independent expert gastrointestinal pathologist.
Read Also: Over The Counter Drugs For Ulcers
When To See A Doctor
People with UC should regularly check in with their doctor to discuss any changes in their condition, as well as any new changes in available treatments.
It is also important to have regular scans, as they may help detect early signs of damage that could be precancerous. Catching colorectal cancer early is crucial to effectively treating it.
Also, people who feel that their current treatment plan is not helping with their UC symptoms should see a doctor.
Unchecked damage from UC is a risk factor for colorectal cancer, so having an effective treatment plan is vital.
A Personal History Of Inflammatory Bowel Disease
If you have inflammatory bowel disease , including either ulcerative colitis or Crohns disease, your risk of colorectal cancer is increased.
IBD is a condition in which the colon is inflamed over a long period of time. People who have had IBD for many years, especially if untreated, often develop dysplasia. Dysplasia is a term used to describe cells in the lining of the colon or rectum that look abnormal, but are not cancer cells. They can change into cancer over time.
If you have IBD, you may need to start getting screened for colorectal cancer when you are younger and be screened more often.
Inflammatory bowel disease is different from irritable bowel syndrome , which does not appear to increase your risk for colorectal cancer.
Also Check: How To Get Remission In Ulcerative Colitis
Recommended Reading: What Foods Should I Avoid With A Stomach Ulcer
Why The Higher Risks
There are several reasons why Crohns Disease and ulcerative colitis increase your risk of cancer.
According to Medical News Today, Inflammation is one of the ways these conditions are linked. Crohns Disease causes high levels of inflammation in the intestines. That inflammation can make it more likely that abnormal cells could become cancerous, especially in the GI tract.
The risks increase under the following conditions:
- The longer you have Crohns disease, the higher the risk of cancer. After eight years, increased screenings should occur every one to two years.
- Getting a diagnosis of ulcerative colitis or a type of Crohns that only affects the colon. This is known as Crohns colitis.
- Suffering from a severe colon inflammation
- Having a family history of colon cancer
- If there are changes in the cells known as dysplasia.
- Having Primary Sclerosing Cholangitis, or PSC, which is an inflammation of the bile ducts.
- Being over the age of 50
What Do Colorectal Cancer Screening Guidelines Say About Who Should Have Colorectal Cancer Screening
Expert medical groups, including the US Preventive Services Task Force , strongly recommend screening for colorectal cancer. Although some details of the recommendations vary, most groups now generally recommend that people at average risk of colorectal cancer get screened at regular intervals beginning at age 45 or 50 .
The expert medical groups generally recommend that screening continue to age 75 for those aged 76 to 85 years, the decision to screen is based on the individuals life expectancy, health conditions, and prior screening results.
People who are at increased risk of colorectal cancer because of a family history of colorectal cancer or documented advanced polyps or because they have inflammatory bowel disease or certain inherited conditions may be advised to start screening earlier and/or have more frequent screening.
Read Also: Can Ulcerative Colitis Affect Your Kidneys
Availability Of Data And Materials
The data that support the findings of this study are available from the DCCSD and The Danish Health Data Authority . Restrictions apply to the availability of these data, which were used under license for this study. Data may be available upon reasonable request to the DCCSD and The Danish Health Data Authority.
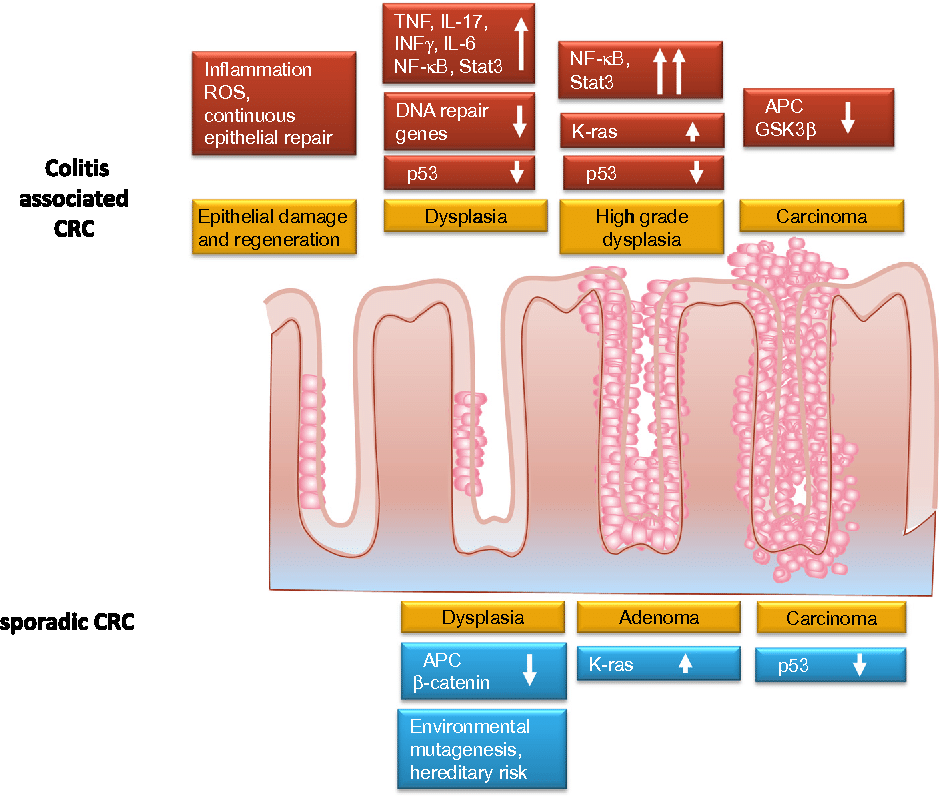
Inflammation And Tumorigenesis In Ibd
The innate and adaptive immune system cells play an important role in the onset of IBD-CRC. Crosstalk between these cell types occurs mainly through a network of cytokines that drive and maintain inflammation and contribute to tumorigenesis via oxidative stress, epithelial cell proliferation, and angiogenesis . In Table 1 is reported a brief summary of the effects of different inflammation-related molecules in IBD-CRC.
TABLE 1. cytokines and/or pro-inflammatory molecules in IBD-CRC.
Among these molecules, the macrophage migration inhibitory factor , a pleiotropic cytokine that drives cellular proliferation and regulates the migration and activation state of immune cells, seems to be relevant. The pathophysiological role of MIF in a wide range of inflammatory diseases, among which IBD, was already demonstrated . Increased MIF in macrophages in a CRC mouse model was demonstrated, and loss of MIF expression protects mice during tumor initiation . In cancer cells from CRC patients and in an acute colitis-CRC mouse model, a tumor-specific elevation of MIF expression was demonstrated . The heat shock protein 90 chaperone machinery stabilizes and protects MIF from degradation and supports tumor progression via macrophage recruitment and angiogenesis.
In the context of inflammation and CRC, the most investigated pathways are the nuclear factor light-chain enhancer and IL-6/signal transducer and activator of transcription 3 and STAT6 signaling pathways .
Read Also: What Is The Difference Between Ulcerative Colitis And Crohn’s Disease
Can Uc Medications Cause Eye Problems
Yes. Some eye complications can be caused by drugs youâre taking for UC.
If your UC doctor or your eye doctor thinks this is happening, they can work together to fine-tune your treatment if needed, Ali says. For instance, they might decide to change the dose of your drug or switch you to a different one.
Some eye problems linked to UC drugs are:
Cataracts and glaucoma. Steroids can cause either of these common conditions, Ali says.
A cataract makes your eyeâs natural lens cloudy. It can make things look blurry, hazy, or less colorful. If it bothers you a lot, you can get it removed with surgery.
Glaucoma is a disease that, without treatment, can damage your optic nerve, which allows you to see. There are different types of it, but any of them could bring on symptoms like eye pain or pressure, headaches, and worse vision, including blind spots. Some treatments that can slow the permanent vision loss it causes are medication, laser procedures, and surgery.
Retinopathies. These are diseases that damage the part of your eye that senses light . Theyâre rarely linked to IBD. But they can happen due to certain biologic drugs that treat IBD, Ali says.
If youâre diagnosed with retinopathy, your eye doctor has treatments that can lower your chances for losing your sight.
Why Regular Colorectal Cancer Screenings Are So Important
Colorectal cancer is curable, especially in the early stages. The best chance of complete remission comes with finding polyps early that need to be removed before they turn into cancer. This makes the entire process easier on you, less invasive, reduces the chance of it spreading to other organs, and is less expensive than late-stage cancer treatment.
To find colorectal cancer early, you need to stick with a regular cancer screening schedule. If you have ulcerative colitis or other medical conditions that put you at risk for colorectal cancer, your primary care doctor may recommend starting cancer screenings younger than the average age of 45. Screening for colon and rectal cancer can be done with an at-home stool test using a test such as a colonoscopy or a sigmoidoscopy. The right test for you, based on the severity of the UC, will be determined by your physician.
Read Also: Foods To Avoid If You Think You Have An Ulcer
How Can I Get Screened
FIT kits are currently available in every NWT community. Book an appointment with your primary care provider to get screened FIT kit. If you are aged 50-74 and of average risk, you will complete a Fecal Immunochemical Test every 1 to 2 year to be screened. This test is a simple one-and-done, at-home poop test that only requires one sample.
NEW TESTING METHOD: This test used to be a three-sample smear poop test. In June 2018 this was changed to a simple, 1-sample poke test.
In communities with hospital laboratories your primary care provider will give you a laboratory requisition to take to the lab to pick up a FIT to take home to complete. Once youve done the FIT at home you need to bring it back to the lab within 7 days.
In the communities without laboratories the FIT will be provided from the Health Centre or Health Cabin. Once youve done the FIT at home you need to bring it back to the Health Centre or Health Cabin within 7 days.
If youre considered to have an increased or special risk or developing colorectal cancer, talk to your primary care provider for them to complete a referral to the specialist.
Recommended Reading: Over The Counter Remedies For Ulcers
How A Colonoscopy Works
In a colonoscopy, a doctor uses a long, flexible tube with a camera at the end to see inside your colon. The test helps them detect polyps in your colon lining. The doctor can remove these growths to prevent them from turning into cancer.
Your doctor might also remove tissue samples during your colonoscopy and have them tested for cancer. This procedure is called a biopsy.
Recommended Reading: Is Ulcerative Colitis A Chronic Disease
What To Expect During A Colonoscopy
About 24 hours before a colonoscopy, you will be asked to clear your bowels with laxatives, enemas, or an all-liquid diet. Be sure to follow the fasting instructions given to you by your healthcare provider.
On the day of the procedure, you will be asked to change into a hospital gown and given a sedative and pain medication, either orally by pill or intravenously . In most cases, you will be awake during the procedure.
Once sedated, your doctor will ask you to lie on your left side, insert the colonoscope through the rectum and use the tool to take pictures. They will also remove any polyps and tissue samples.
The procedure usually takes about 30 minutes, and then you will moved to a recovery room to allow the sedative to wear off. Typically, you will be able to go home the same day.