What Foods Should I Avoid
Certain foods can exacerbate UC flares, but everyone has different trigger foods. For some, it might be a juicy burger and for others, it could be their morning latte.
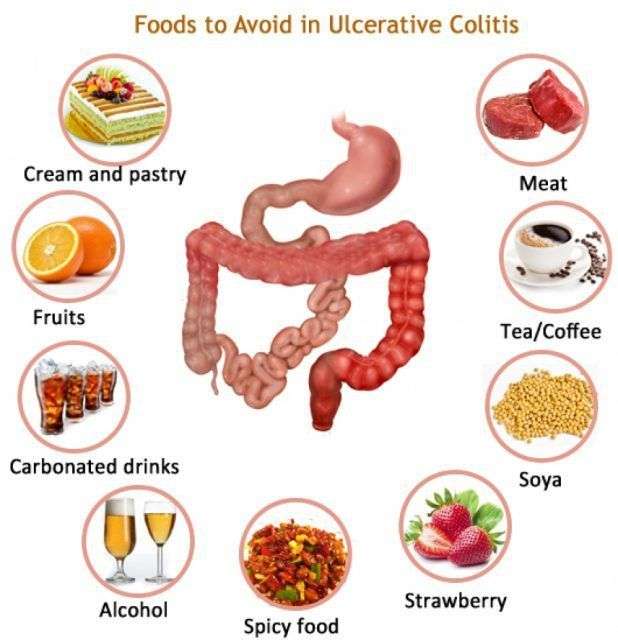
In general, inflammatory foods, like fast food, processed food, alcohol, and sugary drinks contribute to the development of flares, says Dr. Singh. Freuman adds that saturated fat, specifically, can be an issue for certain people. Foods that contain significant amounts of saturated fat include:
- Coconut oil
- Whole-milk dairy, such as cheese, cream, butter, and full-fat yogurt
- Fried foods
- Red meat
Lactose is the sugar present in milk and dairy products, and lactase is the enzyme people need to break down those sugars during digestion. If someone is lactose-intolerant, it means they dont produce enough lactase to break down the sugars, which can cause cramps, bloating, diarrhea, and gas.
To complicate matters, UC is sometimes coupled with lactose intolerance. But lactose intolerant dairy lovers, take heart: Its often possible to still consume dairy with lower lactose content, like cottage cheese and yogurt. Because these products contain live cultures that produce their own lactase, your body doesnt have to do all the work to break down lactose5.
Thats a win-win, since dairy foods provide important nutrients, like calcium and vitamin D, to your diet. In fact, avoiding them completely is not recommended unless 100% necessary.
Food Preparation And Meal Planning
While there is no one-size-fits-all for meal planning, these tips can help guide you toward better daily nutrition:
-
Eat four to six small meals daily.
-
Stay hydrated drink enough to keep your urine light yellow to clear with water, broth, tomato juice, or a rehydration solution.
-
Drink slowly and avoid using a straw, which can cause you to ingest air, which may cause gas.
-
Prepare meals in advance, and keep your kitchen stocked with foods that you tolerate well .
-
Use simple cooking techniques boil, grill, steam, poach.
-
Use a food journal to keep track of what you eat and any symptoms you may experience.
What Can I Do For Periods Of Poor Appetite And Weight Loss To Prevent Malnutrition
At times, there are very few foods that are tolerated well. During these times it is important to eat high calorie foods in tolerable amounts as frequently as possible. During times when solid foods cause irritation or you have a poor appetite, liquid oral supplementation may help provide nutrition. The following list includes liquid supplements for Crohn’s Disease and ulcerative colitis.
Liquid Supplements for Crohn’s Disease
Liquid Supplements for Ulcerative Colitis
Because people with ulcerative colitis do not have malabsorption concerns, a supplement that contains partially broken down protein is not usually needed. Standard supplements are fine but are more easily tolerated if they are isotonic or low concentration, which helps prevent diarrhea. Some formulas that may be helpful include Modulen IBD or Enlive .
Read Also: Can Food Allergies Cause Ulcerative Colitis
Ulcerative Colitis In Children
Without proper care, pediatric ulcerative colitis will result in slower than normal growth and/or stunted growth.Intestinal inflammation lowers a childs appetite, which mean less food is eaten resulting in fewer nutrients to support healthy growth. Supplements are often a good idea as is making sure that enough calories are consumed, which sometimes requires a high-calorie diet for some kids. Additionally, a therapy or counseling may be sought to help a child develop the tools to cope with their disease.
Toasted Potato Bread With Scrambled Eggs And Spinach
Whole-grain foods are a good source of fiber, which normally helps reduce constipation and supports overall health. The high levels of fiber in whole grains may be hard to digest during an ulcerative colitis flare.
Potato or sourdough bread is usually easier to tolerate for people with ulcerative colitis. Top with scrambled eggs for a good source of protein.
Add sautéed spinach for a healthy dose of iron.
Recommended Reading: Best Probiotic Brand For Ulcerative Colitis
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
Diet Recommendations For Crohn’s Disease Flare
- Follow a low residue diet to relieve abdominal pain and diarrhea.
- If you have strictures, it is especially important to avoid nuts, seeds, beans and kernels.
- Avoid foods that may increase stool output such as fresh fruits and vegetables, prunes and caffeinated beverages. Cold foods may help reduce diarrhea.
- If you have lactose intolerance, follow a lactose-free diet. Lactose intolerance causes gas, bloating, cramping and diarrhea 30 to 90 minutes after eating milk, ice cream or large amounts of dairy. A breath hydrogen test may confirm suspicions of lactose intolerance.
- If you have oily and foul-smelling stools, you may have fat malabsorption. Treat fat malabsorption by following a low-fat diet. Discuss these symptoms with your doctor or nutritionist.
- Smaller, more frequent meals are better tolerated and can maximize nutritional intake.
- If your appetite is decreased and solid foods not tolerated well, consider taking nutritional supplements .
Recommended Reading: Ulcerative Colitis And Lung Disease
What Side Effects Of Ibd Can Cause Malnutrition
There are several reasons why people with IBD may be at risk for malnutrition. The following list includes some side effects that contribute to malnutrition.
- Inadequate food/fluid intake may by caused by nausea, abdominal pain, loss of appetite or altered taste sensation
- Increased losses â intestinal inflammation during acute flares results in increased protein losses, losses from fistula fluids, diarrhea and bleeding
- Increased nutritional needs â inflammation or infection increases metabolic requirements
- Malabsorption with Crohns disease may be caused by severe intestinal inflammation, resection of small intestine and medications, such as prednisone and sulfasalazine
Expert Treatments For Ulcerative Colitis
Our inflammatory bowel disease experts deliver advanced care for ulcerative colitis. At the Stanford Inflammatory Bowel Disease Program, you have access to the most advanced care:
- Clinical trials: We offer the latest clinical trials including a trial for the Specific Carbohydrate Diet as Maintenance Therapy in Crohn’s Disease.
- Innovative medical treatment: Our experts have unique expertise in creating medical treatment plans for individual patients.
Recommended Reading: What Are The Signs Of A Bleeding Stomach Ulcer
Foods Rich In Sulfur And Sulfites
Foods like beer, wine, shellfish, some dried fruits, white bread, and cured meats containsulfur, producing excess gas in the colon. Even without these foods, UC patients produce more hydrogen sulfide than usual, and they have difficulty breaking the gas down due to inflammation of the colonic wall. Hence, ingesting more foods with sulfur causes more damage to the colon.
Donât Miss: What Does Asacol Do For Ulcerative Colitis
How To Cure Ulcerative Colitis Naturally
This article is about how to cure ulcerative colitis naturally. In 2010 I was diagnosed with ulcerative colitis and after 1 year of being housebound and shitting blood 30-40 times a day, I thankfully discovered a natural way to cure it.
I have been mostly symptom free for the last 7 years, however sometimes I have had a very slight flare up if I went through a period of intense emotional stress or if I stopped following my protocol and go back to my old bad ways . So according to this Oxford English dictionary definition I can safely say I am cured.
If you are someone who is suffering from ulcerative colitis right now and want to learn how to cure ulcerative colitis naturally without being dependent on medications long term, then you are in the right place.
In this article you will learn:
You May Like: Can You Eat Pizza With Ulcerative Colitis
Also Check: Ulcerative Colitis Diet During Flare
How Is Ulcerative Colitis Diagnosed
To diagnose ulcerative colitis in children, teenagers and adults, your healthcare provider has to rule out other illnesses. After a physical exam, your provider may order:
- Blood tests: Your blood can show signs of infection or anemia. Anemia is a low level of iron in your blood. It can mean you have bleeding in the colon or rectum.
- Stool samples: Signs of infection, parasites , and inflammation can show up in your poop.
- Imaging tests: Your healthcare provider may need a picture of your colon and rectum. You may have tests including a magnetic resonance imaging scan or computed tomography scan.
- Endoscopic tests: An endoscope is a thin, flexible tube with a tiny camera. Specialized doctors can slide the endoscope in through the anus to check the health of the rectum and colon. Common endoscopic tests include colonoscopy and sigmoidoscopy.
Aip Diet Functional Medicine & Treatments

Our History
Our History
Our amazing core team and volunteers are committed to helping others. We take our convictions and turn them into action. Think you would be a good fit? Get in touch for more information!
Our History
Our History
Our History
Founding members fighting autoimmune diseases saw a dire need for passionate, nonprofit work in this area and formed a foundation to provide solutions, education and support.
Our Goal
Also Check: Yea Sacc For Horses With Ulcers
How Is It Diagnosed
Ulcerative colitis is diagnosed by clinical, colonoscopic, and histologic examinations. A colonoscope/sigmoidoscope is inserted into the large bowel and then a sample biopsy confirms the diagnosis. Clinical symptoms and blood tests can help to assess the blood losses and nutritional deficiencies in patients.
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
Read Also: What Are Ulcers In Horses
What To Eat During An Ulcerative Colitis Flare
Research shows that nutrition cant cause or cure ulcerative colitis. There are no foods that can cause someone to develop ulcerative colitis, and there is no miracle diet that will cure people of the condition. However, good nutrition does play an important role in the management of ulcerative colitis symptoms, especially during a flare.
Ulcerative colitis flare-ups are uncomfortable and frustrating. Pain, bloating, cramping, fatigue, rectal bleeding, and diarrhea are common symptoms during flare-ups. If youre in the midst of the flare, changes in your diet can help control your symptoms and allow your intestine time to heal. If you have a flare
While carefully watching what you eat can help ease symptoms of ulcerative colitis, there are very few treatments for ulcerative colitis currently available. Participating in research is one of the best ways to actively search for a cure. Research helps increase the understanding of ulcerative colitis and trial new treatment options. If you or a loved one has ulcerative colitis, fill out the form below to learn more about a clinical trial that you may qualify for.
What Are The Best Vegetables For Ulcerative Colitis
While every gut is different, many people with ulcerative colitis find that they can tolerate a wide range of vegetables when their symptoms are in remission , says Arielle Leben, RD, a member of the Inflammatory Bowel Disease Center Clinical Care Team at NYU Langone Health in New York. These may include:
- Peeled, shredded carrots
- Green beans
- Asparagus tips
What makes these vegetables a particularly good bet? Many are high in soluble fiber, which pulls water into the GI tract to turn the fiber into a thick, gel-like substance during digestion. This type of fiber may be beneficial to patients in a flare experiencing diarrhea, because it slows digestion and can improve the consistency of bowel movements, Leben says.
At the same time, theyre lower in insoluble fiber, which can be irritating to the gut, particularly during a flare. When experiencing active symptoms, a diet low in insoluble fiber can be part of the management process to reduce irritation in the GI tract, Warren explains. Avoiding insoluble fiber might help prevent or reduce bloating, diarrhea, or abdominal pain.
Not all of these vegetables may be right for everyone, and you might find that you can tolerate certain vegetables when youre symptom free but not during a flare. Ulcerative colitis diets arent one size fits all, varying from person to person, Warren says.
Also Check: Can You Develop Ulcerative Colitis Later In Life
Who Gets Ulcerative Colitis
Anyone at any age, including young children, can get ulcerative colitis. Your chance of getting it is slightly higher if you:
- Have a close relative with inflammatory bowel disease .
- Are between 15 and 30 years old, or older than 60.
- Are Jewish.
- Use frequent nonsteroidal anti-inflammatory drugs like ibuprofen .
What Should I Eat
It really depends on how active the inflammation is or if you are in a flare, Marvin Singh, M.D., author of Rescue Your Health, founder of Precisione Clinic, and director of Integrative Gastroenterology at the Susan Samueli Integrative Health Institute at UC Irvine, tells SELF.
Freuman explains that most of the science points to eating anti-inflammatory foods and the Mediterranean diet is a good eating pattern to follow3. This includes fiber-rich foods, like fruits, veggies, legumes, and whole grains. While fiber is generally a good thing for digestion, its important to note that sometimes people with ulcerative colitis cant tolerate too much.
She also recommends eating foods with omega-3 fatty acids , such as fish, nuts or nut butters, avocado, and olive oil, as this type of fat has been shown to decrease inflammation4. I encourage my patients to eat the greatest variety of plant-based foods they can comfortably tolerate, which may look different whether you are in a flare versus remission, says Freuman.
In other words, trial and error is key to figuring out what works best for you.
Recommended Reading: Can A Heating Pad Help Ulcerative Colitis
Other Weight Loss Tips
Other strategies that may help someone lose weight include:
- Cutting down on alcohol: Drinking alcohol can cause a person to experience symptoms of UC and gain weight. People who drink alcohol may find that reducing their intake is an easy way to cut down the number of calories they consume.
- Reducing plate size: People can reduce their portion sizes by replacing their dinner plate with a side plate. A small plate gives the illusion of a full plate while decreasing the portion size.
- Taking steps to improve sleep hygiene: Getting enough sleep can help a person lose weight.
I Have Heard That Fiber Is Good For Ulcerative Colitis What Does Onpoint Say

-
We encourage you to eat a medium/high fiber diet when you are not experiencing a flare up. A high fiber diet is almost always encouraged in all adults, part of maintaining a healthy gut as well
-
If you decide to increase your fiber intake, increase it gradually, even if you are not having GI or IBD issues presently
-
You may find a “Low Residue” approach helpful. We have seen it work well for some people
-
Increase or be aware of hydration and fluid intake. Try to drink at least 64 oz of water per day
-
Some studies show that a higher fiber diet can improve IBD conditions
You May Like: How To Check A Horse For Ulcers
What Are The Diet Recommendations For Ulcerative Colitis
Faq: Dietary Management Of Ibd
Information regarding dietary treatments for IBD is often confusing. Many people receive information telling them to avoid entire food groups or specific foods. However, there is no need to avoid foods unless they worsen your symptoms. It is best to restrict as few foods as possible to increase the chances that you are getting a balanced, nutritious diet. This is important for maintaining the function of your digestive tract and your overall health.
Also Check: What Is A Duodenal Ulcer And How Is It Caused
Scd And Low Fodmap Diet For Ulcerative Colitis
There is a lot of interest but limited clinical evidence for the use of the specific carbohydrate diet and low FODMAP diet for ulcerative colitis.
In one trial, a low FODMAP diet did appear to improve quality of life and symptoms of ulcerative colitis, without improving fecal calprotectin or C-reactive protein, two markers of inflammation. If you are experiencing a lot of IBS-like symptoms, it may be a temporary option to help get symptoms under control.
I have also used low FODMAP foods as a lower fermentation framework for increasing fruit and vegetable intake for those who are currently eating a low fiber diet. I worry about the adoption of a long-term low FODMAP diet in ulcerative colitis as I believe that it might be simply tamping down symptoms by further altering the gut microbiomewhich could be detrimental for long term gut health.
The specific carbohydrate diet is based on a decades-old book called Breaking the Vicious Cycle. To my mind, it is similar to a low FODMAP approach in that it alters the types of carbohydrates available for fermentation in the gut.
It is not uncommon for those who have UC to feel that an SCD diet is helping if that is the case, we will support our client on that chosen path however, I dont believe it is a solution for long term gut health and wont advocate for it in practice. It is a complex diet to follow and isnt supported by the evidence.