Whats The Difference Between Inflammatory Bowel Disease And Irritable Bowel Syndrome
IBD is a disease IBS is a syndrome, or group of symptoms. The causes and treatments are different.
IBS is a type of functional gastrointestinal disease. It affects how the bowels function, causing them to contract more often than usual. IBS is also known as spastic colon or nervous stomach.
IBS doesnt inflame or damage the intestines like IBD, so imaging scans cant detect it and it doesnt increase the risk of colon cancer. People with IBS rarely need hospitalization or surgery.
Crohns Disease And Ulcerative Colitis And Digesting Food
Your mouth and stomach break down food by mechanical and chemical means. When the food has reached a pulp-like consistency, it is slowly released into the first part of the small intestine . The food is then massaged along the length of the small intestine. Organs like the pancreas and the gall bladder make digestive enzymes to further break down the food into its simpler components.
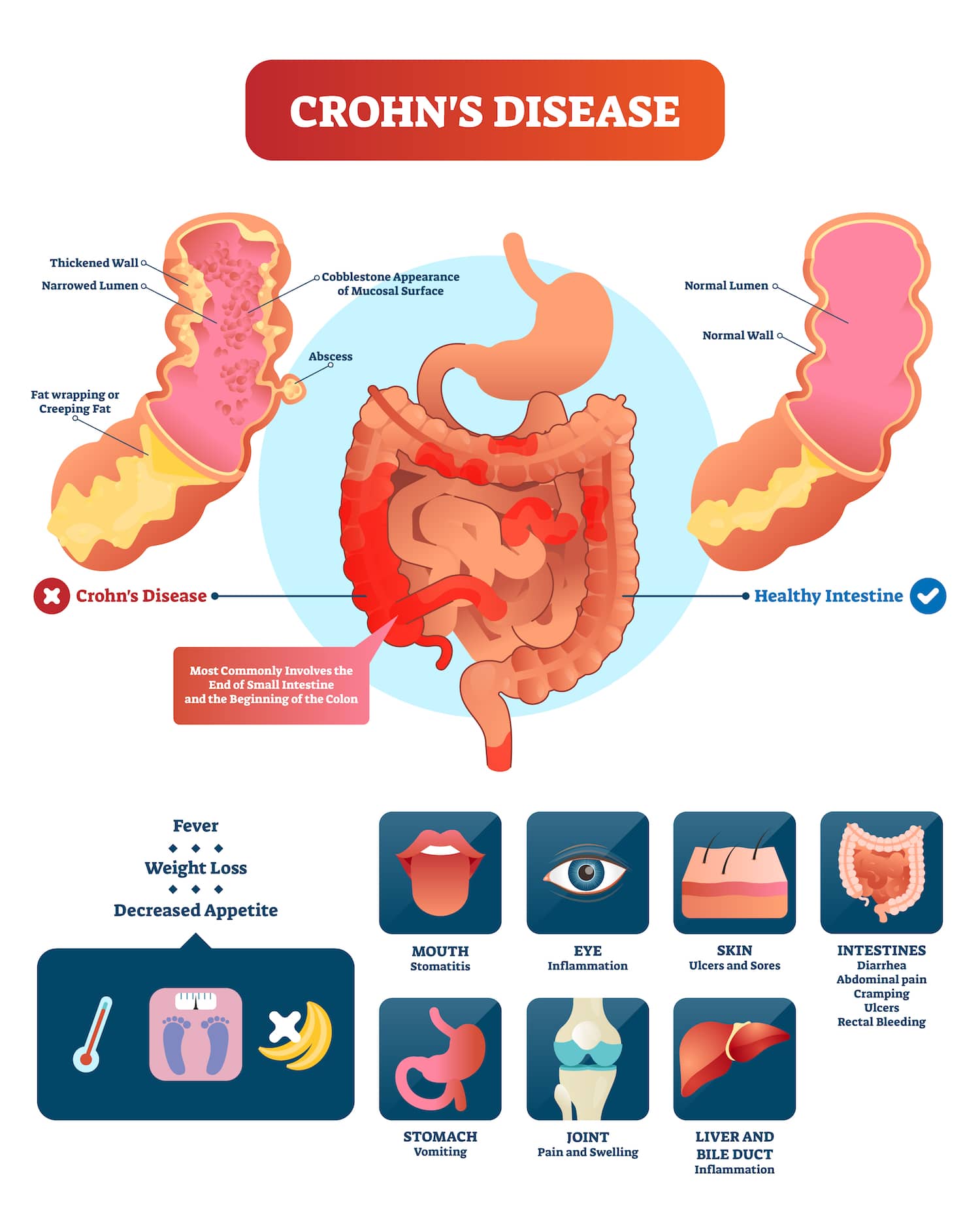
- Crohns disease an inflamed ileum impairs absorption of vitamin B12 and bile salts. Inflammation along the length of the small intestine impairs absorption of all food nutrients. Inflammation of the large bowel impairs water absorption, causing diarrhoea.
- Ulcerative colitis digestion and absorption are generally not affected. Inflammation of the large bowel impairs water absorption, causing diarrhoea.
Other factors that may affect your nutritional status include:
Do Inflammatory Foods Play A Role In Ulcerative Colitis
If youre searching for an ulcerative colitis treatment that starts with your diet, you are far from alone. David Schwimmer, M.D., a board-certified gastroenterologist at Florida Digestive Health Specialists in Sarasota, Florida, sees ulcerative colitis patients on a daily basis and has even lived with the condition himself since he was 18 years old. I think every patient that has a GI illness certainly thinks that what they are consuming and what theyre eating has an impact on their disease, he says.
Exclusion diets like the specific-carbohydrate diet, the semi-vegetarian diet, and the IBD-inflammatory diet continue to grow in popularity within the IBD community. But research to prove that these diets are helpful for ulcerative colitis lags behind the trend. As recently as 2019, a study published in the journal Nutrients concluded that the mechanism by which dietary interventions impact inflammation in IBD remains unknown1. Basically, theres a lot more scientists need to learn before one type of diet reigns supreme for people with IBD.
You May Like: How You Get Stomach Ulcers
What If I Have Symptoms Of Both
If you exhibit symptoms of both ulcerative colitis and Crohns disease, you might have a condition known as indeterminate colitis. This means that you are exhibiting features of both issues, and while treatment may resemble a similar course of action, you do not have either one or the other issue.
Symptoms from both ulcerative colitis and Crohns disease overlap in similarity, and both should be treated with similar levels of care and attention. If you think you may have indeterminate colitis, prioritize hydration and rest. Your body is working overtime to manage inflammation.
A gastroenterologist will assess your risk factors for these and other conditions and may perform tests that include a colonoscopy, blood tests, an endoscopic retrograde cholangiopancreatography , or a CT scan. These tests can help your doctor figure out which forms of inflammatory bowel disease may have affected you while ruling out other conditions. Your doctor will help determine ways to improve your quality of life based on the results.
Crohns Disease Vs Ulcerative Colitis
Danielle Gaffen, MS, RDN, LD
Home | Blog | Inflammatory Bowel Disease | Crohns Disease vs. Ulcerative Colitis
Co-written by Luis Tejeda
Have you ever wondered the difference between Crohns disease vs. ulcerative colitis? Many of my clients ask me what the difference is between the two conditions. While both share similar symptoms and are both types of inflammatory bowel disease , they are not the same illness and affect different areas of the GI tract. This blog will compare the key differences between Crohns disease and ulcerative colitis .
Recommended Reading: Best Diet For Gerd And Ulcers
What Procedures And Tests Diagnose Crohn’s Disease And Ulcerative Colitis
Doctors diagnose ulcerative colitis by endoscopy . During this procedure, the doctor can see and take pictures of the patient’s abnormal gut mucosa , and the presence of continuous disease . Other blood tests and imaging tests like CT scans or MRI are used, but these tests are not definitive.
Doctors use the same procedures and tests to diagnose Crohn’s disease. However, they also use small bowel studies, colonoscopy, and upper GI endoscopy to identify the abnormal gut mucosa that usually occurs in multiple areas anywhere in the intestinal tract. These areas are not continuous but are separated by normal areas of the intestinal mucosa that distinguish them from ulcerative colitis lesions.
As with Crohn’s disease, nutrition is important if you have ulcerative colitis because symptoms of diarrhea and bleeding can lead to dehydration, electrolyte imbalance, and loss of nutrients. It may be necessary to take nutritional supplements if your symptoms do not allow you to eat a nutritionally balanced diet. Talk to your healthcare professional about what supplements to take.
Crohns And Ulcerative Colitis Pose Special Concerns For Women
Karen Nitkin Spring/Summer 2020
About 1.5 million Americans slightly more women than men live with Crohns disease and ulcerative colitis, the chronic gastrointestinal disorders collectively known as inflammatory bowel disease .
Both men and women with IBD experience painful and potentially damaging inflammation of the digestive tract. IBD has no cure treatments focus on controlling and preventing future flare-ups with medications and treating symptoms such as abdominal pain, fever or diarrhea.
Yet IBD affects women in unique ways, says Aline Charabaty, clinical director of gastroenterology and director of the Inflammatory Bowel Disease Center at Sibley Memorial Hospital. It can interfere with menstruation and childbirth and intensify anemia and osteoporosis, she notes.
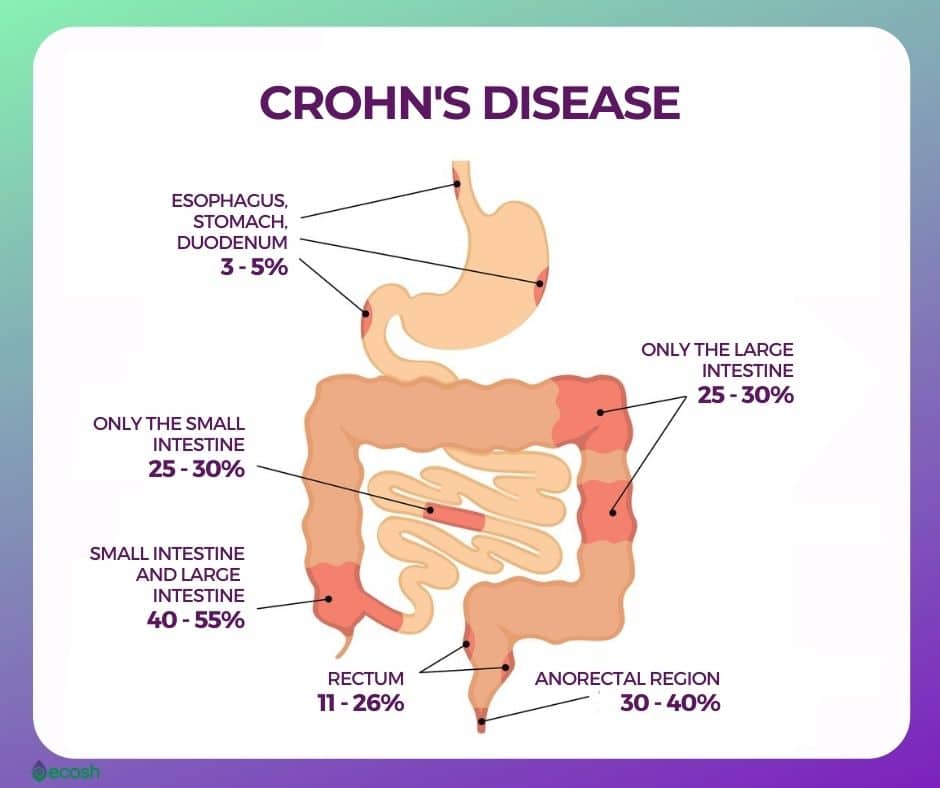
Crohns disease and ulcerative colitis are not exactly the same. Crohns disease is characterized by inflammation in any part of the gastrointestinal tract, with symptoms that can include abdominal cramps, diarrhea, delayed growth, weight loss, fever and anemia. Ulcerative colitis affects the inner lining of the large intestine and rectum, with symptoms that often include bloody diarrhea, frequent bowel movements, abdominal and rectal pain, fever, weight loss, joint pain and rashes.
Here are four ways IBD poses particular concerns for women:
Recommended Reading: Why Do I Get Mouth Ulcers
Are There Geographic Links To Ulcerative Colitis Incidence
All types of IBD happen more often in industrialized nations. North America and Northern Europe have the highest rates of UC in particular.
But experts say IBD is increasingly becoming a global disease. Some believe that a Westernized diet or lifestyle may be at least partly responsible for triggering IBD symptoms.
UC is also thought to be more common in cities than in rural areas.
The condition seems to be more common in countries with advanced sanitation systems, which could mean that less exposure to bacteria increases your risk.
Foods To Avoid During Flares
Diet doesnt cause flares, but your food choices can make symptoms worse if your IBD becomes active.
How foods affect people who are flaring varies from person to person. But here are some of the foods that may worsen symptoms of a flare and cause complications:
- Beverages containing alcohol or caffeine.
- Sugar alcohols used to sweeten in sugar-free foods
- Raw fruits and vegetables
Read Also: What Medications Are Used For Ulcerative Colitis
Also Check: Herbal Ulcer Blend For Horses
Effects Of Crohns Disease And Ulcerative Colitis
Every person responds differently to IBD. The severity of symptoms will vary from time to time and from person to person. IBD is not a progressive disease . Rather, flare-ups can range from mild to severe and back to mild again. Some people will experience periods of relief from symptoms in between flare-ups.We cannot predict how long a person will stay free from symptoms, or when their next flare-up will occur. Some flare-ups settle down quite quickly with treatment. Other times, it may take months for a persons symptoms to respond to treatment.IBD interferes with a persons normal body functions. Signs and symptoms can include:
- pain in the abdomen
Dont Miss: What Is Good For Mouth Ulcers
Special Diets May Help
A variety of organizations and individuals recommend many different diets to help UC. Research generally warns against restrictive diets for UC because no one diet works for everyone. Also, very little research supports the idea that one diet by itself helps all people with UC.
However, these special diets may give you some ideas to work into your nutritional program. They all have slightly different takes on which vegetables are best. Look into them and see what works for you:
- Mediterranean diet
Also Check: How To Prevent Ulcers In Horses
What Types Of Surgery Can Treat Ulcerative Colitis
There are different procedures. All are major surgery on your digestive system. Talk with your doctor about which one they recommend for you.
Hemicolectomy. This is an operation that removes part of your colon. There are two types, depending on where your problem area is:
- Right hemicolectomy: Removes the right, or ascending, part of your colon. The surgeon may also take out some other areas, like your appendix and part or all of your middle large intestine. Theyâll connect whatâs left of your colon to your small intestine.
- Left hemicolectomy: Removes the left, or descending, part of your colon. The surgeon will attach the right and middle parts to your rectum. This is the last place your bowel movements pass through on their way out.
Colectomy. This is surgery to remove the entire colon.
Proctocolectomy. This procedure removes both the colon and rectum.
Proctocolectomy is considered the standard treatment when surgery for ulcerative colitis is needed.
If the entire colon is removed, the surgeon may create an opening, or stoma, in the abdominal wall. The tip of the lower small intestine is brought through the stoma. An external bag, or pouch, is attached to the stoma. This is called a permanent ileostomy. Stools pass through this opening and collect in the pouch. The pouch must be worn at all times.
How We Can Help
Though Crohns disease and ulcerative colitis are typically not fatal or life-threatening issues, they are generally uncomfortable. Additionally, these disorders can cause life-threatening or fatal complications if left untreated. If you are looking for relief from some of the more mild symptoms resulting from either of these disorders, then you might consider intravenous fluid treatment.
Offered discreetly in the comfort of your home or office, The I.V. Doc offers on-call intravenous fluid therapy that can assist with everything from vitamin and nutrient replacement to rehydration. If you are dealing with digestive tract issues, you may be at a higher risk of dehydration or deficiencies.
Intravenous, or IV therapy, offers plenty of electrolytes, vitamins, and nutrients so that you can stay healthy and on the track toward healing.
Don’t Miss: What Happens In Ulcerative Colitis
What Causes Ulcerative Colitis
However, there are cases where the diagnosis of one form of IBD over the other is very difficult. At times, a final diagnosis is possible only after an event during the course of the disease or its treatment makes the form of IBD readily apparent.
Patients with IBD may be very confused as to the differences between these diseases. As with any chronic condition, education is an important tool to become an active participant in one’s own treatment plan.
If your diagnosis isn’t firm, don’t panic. In some people, it can take time to determine if the IBD is more like Crohn’s disease or more like ulcerative colitis. In about 5-20% of cases, people are diagnosed as having indeterminate colitis .
IBD is becoming increasingly treatable and there are now many medications in the arsenal that are helping people with all forms get greater control over their disease. The main differences between ulcerative colitis and Crohn’s disease are described below.
-
Smoking can worsen condition
Does Your Race Or Ethnicity Increase The Risk
Caucasian people are more often diagnosed with UC than those with African or Asian ancestry. And the condition is three to six times more common in people of Jewish heritage than in other groups.
But IBD is being diagnosed more often in Black, Asian, and Hispanic people than in previous years. Its not clear whether this means IBD is becoming more common in these populations, or if it reflects differences in how often doctors are diagnosing it.
You May Like: Does Stomach Ulcer Cause Pain
How Are Ulcerative Colitis And Crohns Disease Diagnosed
If youre looking for one easy test that will definitively tell you whether you have ulcerative colitis or Crohns, you might be disappointed. Getting an ulcerative colitis diagnosis or a Crohns disease diagnosis is a process that involves multiple tests and factoring in your unique symptoms. Theres not that one signature test, says Dr. Balzora. So when we meet somebody and theres a suspicion for the disease, its really just a matter of the story they tell us, their age, and their family history because it does run in families. There are other things that might be ruled out right like an infection or cancer with a colonoscopy , she explains.
Other ulcerative colitis and Crohns disease tests can include an upper endoscopy, where a doctor will use a scope to look inside your stomach and the first part of the small intestine. They may also take a biopsy from one of these tests that they will then study in the lab for signs of inflammation or cancer. Imaging tests, like MRIs and CT scans, can also help give your doctor information about whats going on in your digestive tract.
Sometimes we do something called a video capsule which is basically a pill that you swallow that has a camera inside and allows us to look at the small intestine, says Dr. Balzora. Finally, blood tests may be able to show whether certain inflammatory markers that are consistent with IBD are present in your blood.
How Are Crohns Disease And Ulcerative Colitis Diagnosed
No single test result is enough for a medical doctor to diagnose IBD. Here are the several types of tests commonly used in the diagnostic process for Crohns disease and ulcerative colitis:
- CT scans and/or MRI scans
Once your doctor has reviewed all the tests performed, a diagnosis of Crohns disease or UC can be made.
Recommended Reading: Diet Plan For Someone With Ulcerative Colitis
Telling The Difference Between Conditions
Obviously, theres considerable overlap between the symptoms of celiac disease, non-celiac gluten sensitivity, and inflammatory bowel disease, and that can make getting an accurate diagnosis somewhat challenging.
Healthcare providers use blood tests to screen for celiac disease , and confirm the diagnosis with an endoscopy and biopsy to look directly at the lining of your small intestine to see if its damaged.
To diagnose Crohns disease or ulcerative colitis, your healthcare provider likely will perform a colonoscopy and/or an endoscopy to look for specific signs, which are different from those of celiac disease. Theres no one blood test for inflammatory bowel disease, although more general blood testssuch as one to screen for anemiamay provide some information.
Finally, theres no accepted medical test for non-celiac gluten sensitivity . The only way to know if you have it is to follow the gluten-free diet strictly and see if you feel better. But even thats not definitive: you may feel better because youve reduced or eliminated junk food from your diet along with the gluten, for example, or just the idea that youre doing something positive for your health may help lessen your symptoms. Still, research shows that some people do, indeed, seem to react to gluten grains with symptoms that are similar to those of celiac disease, even though those people definitely dont have celiac disease.
Key Differences In Symptoms Of Ulcerative Colitis Vs Crohns Disease
Although abdominal pain is a common symptom of both Crohns disease and ulcerative colitis, one of the key factors that differentiates the two conditions is the location of the pain .
Crohns: Abdominal pain is more often in the right lower quadrant of the abdomen and in the upper abdomen .
Colitis: People more often experience general lower abdominal pain.
Since the location of the pain is important, noting the location of your abdominal pain can be helpful when you are tracking your symptoms.
There are also a few non-digestive symptoms that are seen more often in Crohns disease and not ulcerative colitis such as gallstones and issues with the bile ducts as well as kidneys.
This table of symptoms might help you see the similarities and differences. Symptoms that are common in both diseases are in bold.
| Ulcerative Colitis |
| Hemorrhoids |
You May Like: Diet For Stomach Ulcers Mayo Clinic
Can Medications Raise Your Risk For Developing Ulcerative Colitis
Taking several courses of antibiotics, especially broad-spectrum ones that act on different types of bacteria, may raise your risk for both UC and Crohns. This might be because antibiotics can affect the delicate balance of bacteria in your gut, known as the microbiome.
Some research has suggested that taking birth control pills could raise your risk for UC by 30% if youre genetically prone to the condition. But we need more studies on this.
If you have UC, your doctor might warn you that taking aspirin or nonsteroidal anti-inflammatory drugs like ibuprofen and naproxen could make your symptoms worse. But these medications arent thought to raise your risk for UC.
One thing that might lower your risk of developing UC? Having your appendix removed before age 20 because of an inflammation . Its not clear why this happens. But scientists theorize that your appendix may have an impact on your immune system.