What Are The Complications Of Bedsores
Once a bedsore develops, it can take days, months, or even years to heal. It can also become infected, causing fever and chills. An infected bedsore can take a long time to clear up. As the infection spreads through your body, it can also cause mental confusion, a fast heartbeat, and generalized weakness.
Use Specialty Bedding Or Materials To Reduce Pressure
Depending on the needs of each senior, specialty beds, such as water or air mattress toppers, or special, cushioned padding, such as heel protectors, may be needed to reduce the amount of pressure placed on sensitive areas of the body. These additional materials should not be limited to mattresses or modifications to footwear. Instead, keep the options open for what may and may not be the most comfortable and beneficial to the needs of seniors.
For example, a memory-foam pillow is great, but it does little good if it is always placed in the same position. Furthermore, soft, pillow-like wedges may be used to help seniors remain on their sides while lying in bed between repositioning times.
Some newer beds may suggest automatic turning is available for use. However, these systems do not completely reposition a person. As a result, it is best to use these systems in conjunction with manually reposition of a person.
Factors That Influence Sacral Ulcer Management
While wound management is a key part of sacral ulcer management, treating patients holistically is the key to success. Apart from ischemia, other factors that impede normal healing include poor nutrition, infection, edema, persistent moisture, fecal and urinary soiling, and shearing forces. One can look for, prevent, or minimize each of these risk factors. Of course, the patient should be frequently repositioned to avoid further tissue damage and to promote healing.
When selecting a dressing, the wound should be kept moist but not contain excessive amounts of exudate. Wound care professionals should consider the type of ulcer and any comorbid conditions that could complicate treatment . Arterial wounds generally require a moisture-retaining dressing, while wounds that arise from venous insufficiency usually require a dressing that absorbs excess moisture. All surfaces of the wound, including any tunnels, should be packed with the appropriate dressing.
Also Check: What Is The Medication For Ulcerative Colitis
Read Also: How To Heal Ulcerative Colitis With Food
What Complications Might Come With Pressure Ulcers
Pressure ulcers can be painful and become infected, and infection may spread from the skin , to blood , muscle or bone. Treatment may require antibiotics, usually at home but sometimes in hospital. In very rare cases, chronic pressure ulcers can cause skin cancer. It’s important to recognise pressure ulcers early and to act quickly to prevent complications.
Vitamin And Mineral Supplements
If you cannot eat enough foods containing key vitamins and minerals then you may need to take a supplement. If you are unable to manage a varied diet, or have a poor appetite, an A to Z type vitamin and mineral supplement may be necessary and these are available from many high street chemists. If you are managing to eat a full and varied diet then there is no benefit in taking high levels of vitamins and mineral supplements – in fact, this can be harmful.
Read Also: Is Cranberry Juice Good For Ulcers
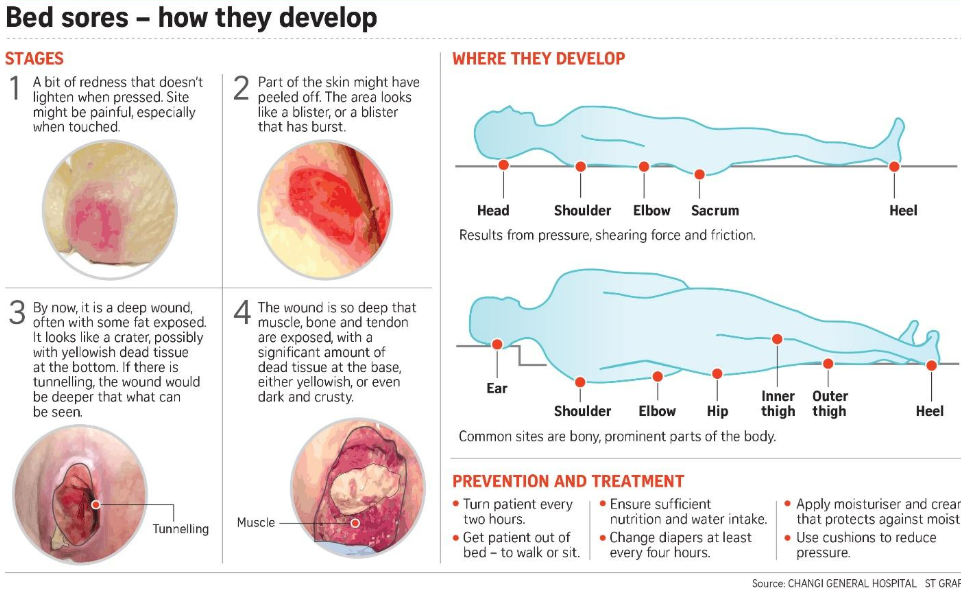
Causes Of Pressure Sores
Pressure sores happen if you cant move around and so stay in one position for a long time. We normally move about constantly, even in our sleep. This stops pressure sores developing.
People who are unable to move around tend to put pressure on the same areas of the body for a long time. If you are ill, bedridden or in a wheelchair, you are at risk of getting pressure sores.
A number of things can increase your risk of pressure sores, including:
- being unable to move around easily due to old age or illness
- weight loss – you may have less padding over bony areas
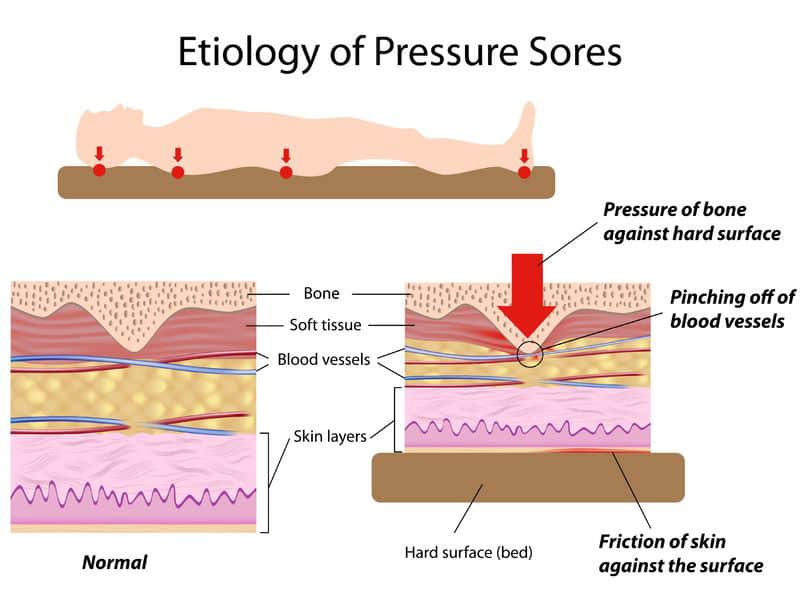
- sliding down in a bed or chair – pressure on the skin cuts off blood supply because the skin is being pulled in different directions
- friction or rubbing of the skin, for example against sheets
- a poor diet
- moist skin – for example, due to sweating or incontinence
- other medical conditions, such as diabetes
- having a previous pressure ulcer
Preventing Sacral Pressure Ulcers
Turning and repositioning protocolscombined with the implementation of pressure-reducing and pressure-relieving devicesare crucial to addressing the risk of sacral pressure ulcers.
When implementing protocols, it is important to take into consideration the four main risk factors for sacral pressure ulcers: pressure, friction, shear, and moisture.1 The European Pressure Ulcer Advisory Panel and National Pressure Ulcer Advisory Panel guidelines recommend that repositioning should be undertaken to reduce the duration and magnitude of pressure over vulnerable areas of the body while avoiding subjecting the skin to pressure and shear forces and using an alternating 30-degree tilted side-lying position.2 The Wound Ostomy and Continence Nurses Society recommends addressing moisture with underpads that are absorbent to wick incontinence moisture away from the skin.3
Another important factor to consider when developing a turning and repositioning protocol is staff safety. Turning and repositioning puts staff at risk for musculoskeletal disorders .4 In fact, one survey found that 89% of clinicians said that they or a co-worker have experienced a back, shoulder, or wrist injury due to turning or boosting a patient.5
You May Like: Ulcerative Colitis And Bowel Obstruction
Diet And Lifestyle Changes To Avoid Pressure Sores
Changes to avoid pressure sores include:
- Make sure you eat a healthy and nutritious diet. This includes a balanced diet and fluids/water. And if necessary,youre your doctor about vitamin and nutritional supplements .
- Low body weight or being overweight can cause pressure sores, so make sure you maintain heathy body weight
- If youre malnourished or at risk of malnutrition, protein, fluid and energy intake should be increased.
- Be aware of using good hygiene practices.
- Maintain activity levels, where appropriate.
- Make sure you quit smoking.
Negative Pressure Wound Therapy
This is an invaluable tool in the management of pressure sores and involves the application of sub-atmospheric pressure to a wound using a computerised unit to intermittently or continuously convey negative pressure to promote wound healing. NPWT, is effective for deep, cavitating, infected and copiously discharging pressure ulcers, particularly with exposed bone. With growing clinical experience it can be said with certainty that it assists wound healing, and its benefits can be summarised thus:
-
Assists granulation.
You May Like: Ulcerative Colitis Is It Deadly
Read Also: What To Do When You Have A Stomach Ulcer
Is This Guidance Up To Date
Next review: 2022
NICE medical technologies guidance addresses specific technologies notified to NICE by sponsors. The case for adoption is based on the claimed advantages of introducing the specific technology compared with current management of the condition. This case is reviewed against the evidence submitted and expert advice. If the case for adopting the technology is supported, then the technology has been found to offer advantages to patients and the NHS. The specific recommendations on individual technologies are not intended to limit use of other relevant technologies which may offer similar advantages.
This guidance replaces NICE medtech innovation briefing on Mepilex Border dressings for preventing pressure ulcers .
Your responsibility
This guidance represents the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, healthcare professionals are expected to take this guidance fully into account, and specifically any special arrangements relating to the introduction of new interventional procedures. The guidance does not override the individual responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or guardian or carer.
Treatments For Pressure Ulcers
Treatments for pressure ulcers depend on how severe they are.
For some people, they’re an inconvenience that needs basic nursing care. For others, they can be serious and lead to life-threatening complications, such as blood poisoning.
Ways to stop pressure ulcers getting worse and help them heal include:
- applying dressings that speed up the healing process and may help to relieve pressure
- moving and regularly changing your position
- using specially designed static foam mattresses or cushions, or dynamic mattresses and cushions that have a pump to provide a constant flow of air
- eating a healthy, balanced diet
- a procedure to clean the wound and remove damaged tissue
Surgery to remove damaged tissue and close the wound is sometimes used in the most serious cases.
Read more about the treatments for pressure ulcers.
Also Check: Food To Avoid For Ulcer Patient
What Causes Sacral Pressure Ulcers
Pressure ulcers occur when there is prolonged pressure to the skin, usually over bony areas such as the elbows, spine, or sacral area .
Compression of the soft tissue causes blood vessels to collapse and reduces blood flow and oxygen delivery. This localized tissue damage usually happens when a person sits or lays for long periods of time in a chair, wheelchair, or bed.
Pressure ulcers begin forming under the skin, making them difficult to catch before a wound is actually visible. So its important to take these steps to help prevent sacral pressure ulcers from happening.
Keep The Skin Dry And Clean
Incontinence is one of the biggest factors associated with the development of pressure sores. When bowel movement or urine stays in contact with the skin, acids and enzymes in them will begin to cause excoriation and degradation of the skin faster than usual. When combined with limited ability to reposition oneself, a senior may develop a pressure sore in the perineal area faster.
If the area appears to become reddened, the senior may have developed a Stage I pressure sore. When this occurs, it is best to assume the area has been subject to more intense pressures and proceed with an appropriate treatment, such as the use of a barrier cream to help prevent further excoriation due to bodily substances. However, the use of a barrier cream does not negate the need for continued repositioning and movement to help prevent worsening of the area.
Also Check: How Do You Diagnose A Stomach Ulcer
Risk Factors For Pressure Sores
A pressure sore is caused by constant pressure applied to the skin over a period of time. The skin of older people tends to be thinner and more delicate, which means an older person has an increased risk of developing a pressure sore during a prolonged stay in bed.
Other risk factors for pressure sores include:
- immobility and paralysis for example due to a stroke or a severe head injury
- being restricted to either sitting or lying down
- impaired sensation or impaired ability to respond to pain or discomfort. For example, people with diabetes who experience nerve damage are at increased risk of pressure sores
- urinary and faecal incontinence skin exposed to urine or faeces is more susceptible to irritation and damage
- malnutrition can lead to skin thinning and poor blood supply, meaning that skin is more fragile
- obesity being overweight in combination with, for example, immobility or being restricted to sitting or lying down can place extra pressure on capillaries. This then reduces blood flow to the skin
- circulation disorders leading to reduced blood flow to the skin in some areas
- smoking reduces blood flow to the skin and, in combination with reduced mobility, can lead to pressure sores. The healing of pressure sores is also a slower process for people who smoke.
If youre bedridden, pressure sores can occur in a number of areas, including:
- back or sides of the head
- rims of the ears
Patients Inclusion And Exclusion Criteria
The CKF method was applied in elderly patients admitted to restore severe sacral PUs defects during the period of 20122015 in our unit. Patients were eligible for inclusion if they were: aged 70 years or above, suffered NPUAP stage 3, 4 or deep tissue pressure injury, not in need of life-saving support, and underwent CKF surgery immediately to close the resultant defects . Patients were excluded if they were: younger than 70 years, declined to participate, NPUAP stage 1 and 2, with a previous severe injury or surgery to the buttocks, laboratory tests indicating low hemoglobin levels and albumin levels, high level white blood cells and C-reactive protein, X-ray indicating osteomyelitis, or existence of comorbidities for anesthesia and surgery, such as diabetes with target organ complication, venous thrombosis, cancer, Parkinsons disease, dementia or receiving end of life care.
Read Also: Is Constipation A Symptom Of Ulcerative Colitis
Try To Maintain Nutrition
There is a strong correlation between nutrition deficits and pressure ulcer risk. If your loved one has an appetite, try to maintain adequate nutrition with nutrient-rich foods . If his appetite is waning, offer supplements such as Ensure or Boost to help bolster nutrition.
Nutrition is often a problem in palliative care patients and its important to note here that you should never try to force your loved one to eat.
What Is A Sacrum Dressing
- To prevent pressure ulcers from forming
- To treat already existing medium to high exuding sacral wounds like pressure injuries and ulcers
- Mepilex border combines the ability to handle and retain draining fluid so exudate is managed with less risk of maceration or skin break down.
- Mepilex uses Safetac technology which reduces pain and tissue damage during dressing changes.
- Mepilex dressings with Safetac technology do not stick to the wound bed they seal the wound edge to prevent maceration, they dont strip skin when removed while providing an optimal wound bed for quicker healing.
- Mepilex Border Sacrum dressing is an all-in-one foam dressing for pressure ulcers and other chronic and acute wounds of the sacral area.
Read Also: Easy To Digest Foods For Ulcerative Colitis
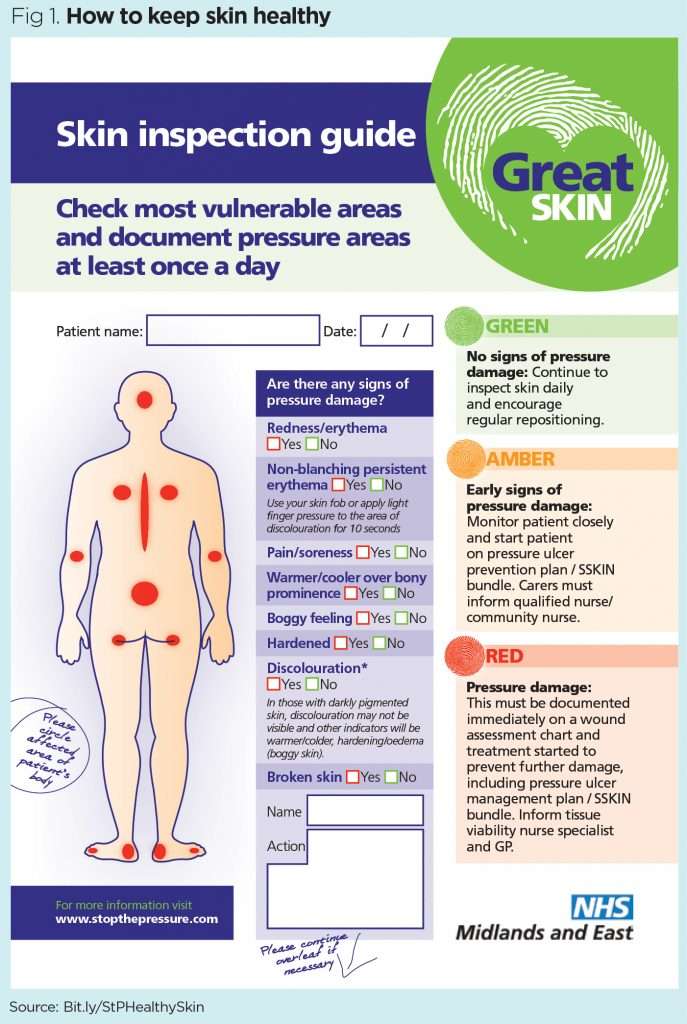
Assessing Sacral Pressure Ulcers
Pressure-induced skin and soft tissue injuries are often classified using the National Pressure Ulcer Advisory Panel staging system . Under this rubric, the wound should be staged to its deepest extent. This means selecting the highest number stage that accurately describes any part of the wound.
- Stage 1 Pressure Injury: Non-blanchable erythema of intact skin
- Non-blanchable is redness that stays despite applying pressure. This means the erythema is not caused by blood within capillaries . Purple or maroon discoloration is not part of stage 1, but rather indicates a deep tissue pressure injury.
Simple Ways To Prevent Sacral Pressure Ulcers
Pressure ulcers, also called bed sores, are among the most common wounds seen in the hospital, long-term care facilities, and even in the home. These wounds can be painful, difficult to heal, and lead to serious complications.
Luckily, there are some simple and effective things you can do to prevent sacral pressure ulcers!
Read Also: How To Prevent Skin Ulcers
Encourage Seniors To Maintain A Healthy Diet
The benefits of a well-functioning circulatory system are only as good as the nutrients it delivers. Seniors should strive to eat a well-balanced, healthy diet, explains Medscape. In fact, optimizing the nutritional status of a senior living with a pressure sore is key to ensuring successful treatment. For seniors living with metabolic disorders, such as diabetes, a healthy diet can go much further than simply preventing or encouraging the healing of pressure sores.
How Can I Prevent Pressure Ulcers
Pressure ulcers can be avoided, but often you may need help. If you have difficulty moving, preventing pressure ulcers might require a team effort, involving your health team, carer or a family member.
To protect your skin and prevent pressure ulcers, the following will help:
- Keep active and move as much as you can .
- Eat a variety of nutritious foods, including plenty of fruits and vegetables.
- Drink plenty of fluids to make sure you are hydrated.
- Avoid smoking because this reduces blood flow to your skin.
- Avoid firm massage, especially over bony areas.
- Keep your skin dry as far as possible.
- If you feel any skin pain or a feeling of burning, tell your doctor.
There are several things that will help you care for your skin:
- Instead of soap, use a mild cleanser and dry the skin gently afterwards.
- Apply moisturisers if the skin is dry, flaky or seems to crack easily.
- Use barrier cream in skin folds.
- Use warm water when having a bath or shower.
It is important to move around as often as you are able. Continuous pressure on the same areas can lead to a pressure ulcer developing very quickly. The following may help you avoid this:
- Change positions in bed at least every 30 minutes and, if you can, stand up and walk around.
- If you cant stand, move as much as you are able for example, lean forward or move side to side in your chair for 2 minutes to take the pressure off your bottom and hips.
- Try to avoid slumping or sliding forward in your chair.
Don’t Miss: Medications For Ulcers Over The Counter
How Can Friends And Family Help
Caregivers might sometimes provide too much help. For instance, they might turn someone over in bed although the person is actually still capable of turning over in bed themselves, perhaps with just a little assistance. It is better to only help as much as needed, so the person stays as independent as possible, helping to prevent pressure ulcers.
If you are caring for a family member at home or go to visit them in the hospital or at a nursing home, you can help them move short distances, for instance when taking a few steps to the table to sit down and eat.
If someone needs to lie in bed for a long time, a nursing care plan is usually made together with nursing professionals. This may include information such as how many times a day a person needs to be repositioned. It is important for everyone to make sure that the plan is followed properly. This also includes regularly changing diapers or incontinence pads.
You should tell the nurses or doctors immediately about any red or sore areas of skin. They can then take a closer look at the affected area. It is always important to take pressure off that part of your body.