Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
Ulcerative Colitis And Colorectal Cancer
Ulcerative colitis increases the risk of colorectal cancer. Colorectal cancer often begins as small growths on the inside of the large intestine. The risk of colorectal cancer increases based on:
- the length of time a person has had ulcerative colitis
- how much of the colon is affected by ulcerative colitis
People with ulcerative colitis should have more frequent tests for polyps and colorectal cancer than people at average risk. The gold standard screening test is a colonoscopy. Polyps can be removed during a colonoscopy. This reduces the risk of colorectal cancer. Ask your doctor how often you should be checked for colorectal cancer.
Surgery to remove the entire colon eliminates the risk of colon cancer.
Does Uc Compromise The Immune System
If a person does not manage their condition correctly, UC may lower their immune systems overall function. Excessive immune activity in the gut could mean less immune activity in the rest of the body.
The following table shows a list of immunosuppressive drugs that can treat IBD, as well as drugs that do not suppress the immune system:
| Immunosuppressant treatment for IBD |
|---|
| 5-aminosalicylates:Mesalamine, balsalazide, olsalazine, sulfasalazine |
| Immunomodulators: Azathioprine, 6-mercaptopurine, methotrexate |
, the current evidence suggests people with inflammatory bowel disease , which includes UC and Crohns disease, are not at higher risk of COVID-19 than the general population.
Immunomodulators and biologics are all unlikely to raise a persons risk of infection.
The American College of Gastroenterology adds that most people taking standard IBD therapies do not have a higher risk of getting COVID-19. They listed the following statements that a person with IBD may find useful regarding COVID-19:
2021 review found that treatments for IBD did not increase the risks of COVID-19 complications, except for people taking aminosalicylates and steroids.
In people with IBD who tested positive for COVID-19, 27% of people required treatment in a hospital, and mortality rates were less than 5%.
Researchers also found that taking biologics reduced negative outcomes.
In a position statement on COVID-19 vaccines, the Crohns and Colitis Foundation states:
You May Like: Stage 2 Pressure Ulcer Treatment Cream
Association Of Ulcerative Colitis And Autoimmune Haemolytic Anemia
- Berraida R1*, Rouibaa F2, Alaomari A2, EI Hamdouchi H2, Jamal S2, Touibi Y2 and Aouragrh A2
- 1 Department Of Gastroenterology, Mohamed V Military Training Hospital, Rabat, Morocco
- 2 Department Of Gastroenterology I, Mohamed V Military Training Hospital, Rabat, Morocco
*Corresponding Author:
Email:Received DateAccepted DateDOI:
Primary Sclerosing Cholangitis And Gastrointestinal Immune Mediated Diseases
PSC is predominant in men and most frequent in UC. We found PSC to be associated with both types of IBD and both genders. Most striking is the association with CD which is less often described. Studies suggest that PSC is more frequent when colon is affected and a distinct subtype, PSC-IBD has been suggested. This study does not include data on localization, severity or extension. Several PSC risk genes are shared with IBD and other IMDs. Gene mutations influencing IL 10 signaling are identified in CD, UC and PSC. The absence of IL 10 can cause severe CD due to lack of Th1 and macrophage inhibition. Interestingly, hepatobiliary inflammation is thought to be induced by microbial metabolites and changes in the microbiota and this inflammation is linked to the FUT2 gene, which is also found in CD.
You May Like: Ulcerative Colitis And Lung Disease
How To Manage Symptoms Of Uc
Keeping symptoms of UC in remission can be protective against infection with the virus that causes COVID-19. Therefore, it is important a person knows how to manage their condition. A doctor can provide the most accurate and individualized information. Some treatment methods a doctor may recommend could include:
Should I Have The Flu Vaccine This Year
This year, more people across the UK will be offered the flu vaccine – including those who are clinically extremely vulnerable, or live with someone who is. Find out more in our information on the flu vaccine.
If you take a medicine that weakens your immune system, like a biologic or immunosuppressant, you should have the annual flu vaccine to reduce your risk of complications – so you should speak to your doctor about whether you may be eligible to have the vaccine for free. You may find our open letter to vaccine providers explaining who with Crohn’s or Colitis is eligible for the free flu vaccine helpful.
You May Like: What Not To Eat With Bleeding Ulcers
What Should I Do If I Think Im Having An Ibd Flare
We have treatments available that are safe to start even while this pandemic is going on. There’s guidance that we’ve developed and published that will give people more information about which treatments to use and when to use them. If a patient has more severe inflammatory bowel disease, the usual treatments we use for IBD are safe and appropriate to be used in this setting. Patients shouldn’t ignore their IBD symptoms or any other digestive symptoms. Keep in touch with your physician to get it back under control quickly. The last thing we want is for patients to be living with these symptoms and afraid to notify their doctor or come to the clinic.
Should I Stop Taking My Medicine
The short answer is, âNo.â If you stop taking your medicine because youâre worried about your immune system, your symptoms may flare. Some medicines take months to leave your system anyway. So stopping them now wouldnât change your risk of COVID-19 now. And you definitely donât want to have to go to a hospital now because of a flare.
It may be a good idea to avoid steroids if you can. But you shouldnât stop taking them suddenly. As a general rule, donât change any of your medications without first talking to your doctor.
Recommended Reading: Can Ulcerative Colitis Cause Cancer
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
Also Check: Can I Donate Blood If I Have Ulcerative Colitis
How Do I Know The Difference Between An Ibd Flare
It may be hard to tell the difference between a flare up and COVID-19 infection because their symptoms can be similar. Loss of appetite, abdominal discomfort, more frequent bowel movements or loose stools are symptoms of both conditions.
We have testing options that do not require an in-person visit. These simple tests can help identify the cause of your symptoms.
Will I Still Be Able To Have Surgery
Some scheduled operations and procedures are being delayed because of the coronavirus pandemic. Its understandable to be concerned if this happens, but your healthcare team will have carefully weighed up all the risks before deciding to delay your surgery. If you have a higher risk of severe complications from coronavirus, it is better where possible to delay your surgery until the virus is less of a risk in hospitals. Your IBD team will be keeping a close eye on the situation, and will rebook your surgery as soon as it is safe to do so. Your hospitals IBD Nurse will be able to offer you advice on keeping well while you wait for surgery.
The NHS will always be able to provide urgent or emergency operations for people who need it most. People with surgical complications of perianal Crohns Disease should still be able to access emergency drainage of abscesses.
If your symptoms start to get worse, its important to let your IBD team know. Its understandable to be concerned about going into hospital during the coronavirus pandemic, but if you delay seeking medical help your condition could get worse, and require more treatment and a longer stay in hospital. It would be a good idea to keep an eye on your symptoms and keep a record if they change, including a description, date and time.
If your concerns about cancelled surgery have not been resolved by your hospital team, you may find it helpful to speak to your local Patient Advice and Liaison Service .
You May Like: Treating Leg Ulcers With Sugar
Tips To Treat Episodes Of Ulcerative Colitis
To properly treat an episode of ulcerative colitis, its extremely important that you receive a medical diagnosis. A health professional can determine if the symptoms you experience are due to ulcerative colitis or other problems like Crohns disease or diverticulosis.
The medical examination might include blood tests, stool samples, a barium enema, or colonoscopy, among others. Then, if the symptoms correspond to an episode of ulcerative colitis, the doctor might suggest some medicine and lifestyle changes. In the most serious cases, surgery might be necessary.
Generally, there are some tips that can help prevent and treat these outbreaks. They are simple measures that you can take in your daily life, both in times of remission and during episodes. Put them in practice!
Are There Extra Precautions That Pregnant Women With Ibd Should Be Taking During The Covid
We’ve learned some information about COVID-19 in pregnant women, which applies to pregnant patients with Crohnâs disease or ulcerative colitis as well. We have seen that women who are pregnant and develop COVID-19 recover similarly to the general population. Although their babies might be born a bit early or a little underweight, for the most part, the babies seem to do well.
At this time, we have not seen cases of pregnant women becoming infected with COVID-19 in the first trimester. The data we have from prior coronavirus epidemics and other types of infections suggest patients may be fine. Because this is a novel coronavirus, we still need to monitor those patients carefully.
Also Check: How To Heal Mouth Ulcers Fast
Homeopathic Treatment For Ulcerative Colitis
Homeopathic treatment for Ulcerative Colitis is natural and very effective. Homeopathic medicines for ulcerative colitis work by moderating the overactive immune system. The homeopathic medicines for ulcerative colitis work on three levels. Firstly they aim to control the acute symptoms of diarrhea containing blood/mucus and tenesmus in ulcerative colitis. Here the intensity and frequency of symptoms are controlled. Secondly, they help in halting the progress of inflammation and ulcer formation in colon and rectum. Thirdly, they help in improving general health that has been deteriorated from long standing ulcerative colitis. Homeopathic medicines for ulcerative colitis are totally safe for use . Even if they are used for a long periods, homeopathic .
The homeopathic medicines for ulcerative colitis that I have found to be the most effective are Merc Cor, Merc Sol, Nux Vomica, Phosphorus and Colchicum.
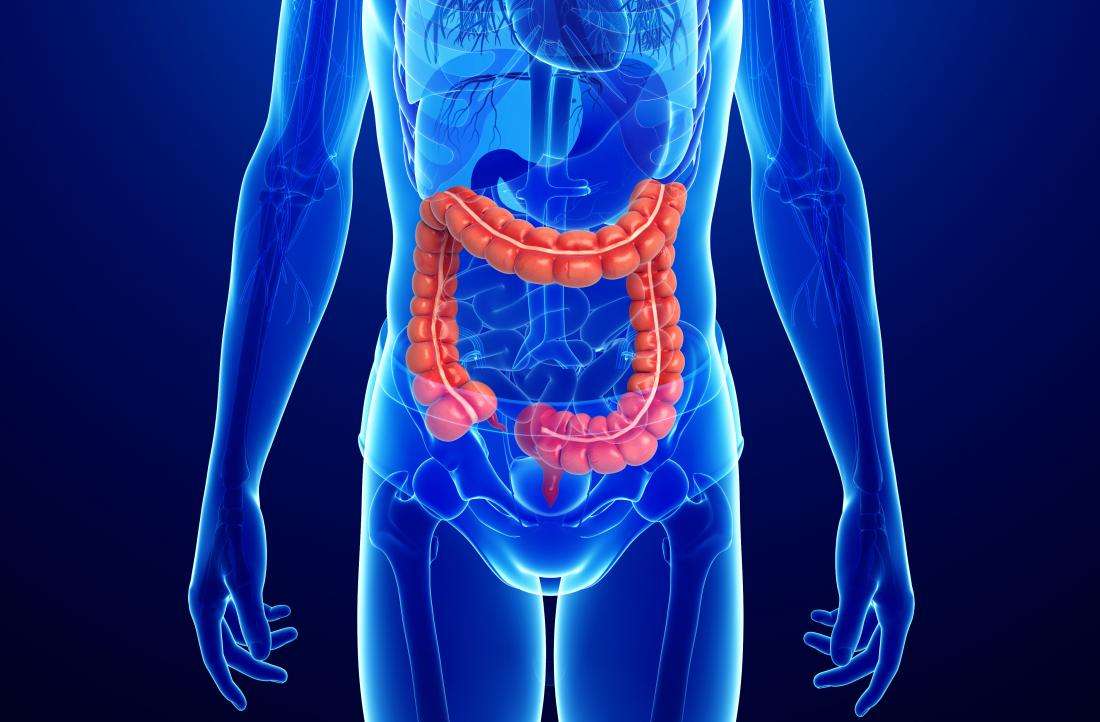
What is Ulcerative Colitis?
Ulcerative Colitis is a disease in which inflammation and ulcers occur in the colon and rectum. Colon refers to the large intestine of our body. In ulcerative Colitis any part of colon can get affected. Ulcerative Colitis is one of the two diseases which fall under the term inflammatory bowel disease. The other being Crohns disease.
What Causes Ulcerative Colitis?
What are the Symptoms of Ulcerative Colitis?
Should You Get A Colonoscopy During The Pandemic
Many IBD patients get a colonoscopy every year or two to keep tabs on their symptoms. If youre due for one, is it safe at this time? According to a new review, published in the journal Lancet Gastroenterology & Hepatology, IBD patients and their providers need to weigh the pros of accurate disease monitoring against the risks of possible exposure to COVID-19.
The authors advise that most IBD patients should postpone routine colonoscopies, but that there are certain circumstances in which it is wiser not to delay. For instance, someone who has symptoms of a bowel obstruction or is experiencing bleeding and other symptoms of severe acute colitis likely needs to have a colonoscopy as soon as possible. A person who develops IBD symptoms for the first time might also need a colonoscopy in order to get the correct diagnosis.
Don’t Miss: How You Know If You Have A Stomach Ulcer
Symptoms Of Ulcerative Colitis
Some people with ulcerative colitis have only occasional symptoms. For others, the symptoms are constant. The symptoms a person experiences can vary depending on the severity of the inflammation and where it occurs in the large intestine.
Common symptoms include:
- diarrhea, often with blood and mucus
- cramping abdominal pain, especially in the lower abdomen
- a frequent sensation of needing to have a bowel movement
- little advance warning before a bowel movement
- the need to wake from sleep to have bowel movements
- feeling tired
- dehydration
- low red blood cell count
Some people with ulcerative colitis develop pain or soreness in the joints, irritated eyes, and rashes.
The symptoms of ulcerative colitis can suddenly get worse. This is called a flare. Then symptoms may fade away. This is called remission. Some individuals with ulcerative colitis have symptoms only rarely, others have flares and remissions, others have symptoms all or most of the time.
How Can You Reduce Your Chances Of Getting Covid
If you have Crohns disease or ulcerative colitis, consider that you could be immunosuppressed at least to a certain degree. You should be practicing social distancing to the fullest extent that you can.
Ideally, stay home and let someone else do the food shopping, says Dr. Morganstern. You should also be extra strict about good hand hygiene, wearing a face mask in public places, and regularly disinfecting commonly used surfaces in your home.
Dr. Ungaro adds that this is a stressful time for everyone, and that many IBD patients report that their symptoms get worse when theyre stressed even if blood tests dont always show that inflammation has increased.
There is a very strong brain/gut connection, he says. Its normal to have anxiety, but if you can do something proactive about it like connect with a psychologist or social worker through telemedicine its a good idea.
You can also try to exercise more at home, download and use a meditations app, or do anything else that helps you unwind. You can get mental health advice for coping with coronavirus-related anxiety and other issues through our GHLF Patient Support Program.
Also Check: Can I Eat Oatmeal With Ulcerative Colitis
Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
How Is Ulcerative Colitis Diagnosed

To diagnose ulcerative colitis in children, teenagers and adults, your healthcare provider has to rule out other illnesses. After a physical exam, your provider may order:
- Blood tests: Your blood can show signs of infection or anemia. Anemia is a low level of iron in your blood. It can mean you have bleeding in the colon or rectum.
- Stool samples: Signs of infection, parasites , and inflammation can show up in your poop.
- Imaging tests: Your healthcare provider may need a picture of your colon and rectum. You may have tests including a magnetic resonance imaging scan or computed tomography scan.
- Endoscopic tests: An endoscope is a thin, flexible tube with a tiny camera. Specialized doctors can slide the endoscope in through the anus to check the health of the rectum and colon. Common endoscopic tests include colonoscopy and sigmoidoscopy.
Read Also: What To Do When You Have A Stomach Ulcer
What Research Is Happening On The Coronavirus And Crohn’s And Colitis
Scientists and healthcare professionals across the world are united in their mission to better understand the coronavirus, to find treatments and develop a vaccine. This includes the dedicated community of Crohns and Colitis researchers and IBD teams. There are many current and future studies on the coronavirus and Crohns and Colitis, investigating areas such as:
- Symptoms, like pain or gastrointestinal symptoms, and flares during the pandemic.
- The impact of different Crohns and Colitis medicines on the severity of COVID-19 illness.
- The development of antibodies in people with Crohns and Colitis in those infected with the coronavirus or in response to the vaccine.
Find out more about the studies investigating coronavirus and Crohns and Colitis