Living With Pressure Sores
Living with pressure sores requires a plan to move and turn frequently. Good hygiene will always be required. Pressure sores should be kept covered with a bandage or dressing. Sometimes gauze is used. The gauze must be changed once a day. Newer materials include a see-through film and a hydrocolloid dressing. A hydrocolloid dressing is a bandage made of a gel. It molds to the pressure sore and promotes healing and skin growth. These dressings can stay on for several days at a time.
Dead tissue in the sore can interfere with healing and lead to infection. Dead tissue looks like a scab. To remove dead tissue, rinse the sore every time you change the bandage. Special dressings can help your body dissolve the dead tissue on its own. The dressing must be left in place for several days. Another way to remove dead tissue is to put wet gauze bandages on the sore. Allow them to dry. The dead tissue sticks to the gauze until it is removed. For severe pressure sores, dead tissue must be removed surgically by your doctor.
Removing dead tissue and cleaning the sore can hurt. Your doctor can suggest a pain medicine. Take it 30 to 60 minutes before changing the dressing.
Healthy eating helps sores heal. Make sure youre eating the proper number of calories and protein every day. Nutrients are important too, including vitamin C and zinc. Ask your doctor for advice on a healthy diet. Be sure to tell them if youve lost or gained weight recently.
+ Best Dressing For Stage 2 Pressure Ulcer On Buttocks Png
Read Also
What is the treatment for a pressure ulcer? This video discusses how to assess and provide localized wound care for a pressure injury, and includes a demonstration of how to clean and . Without treatment, they can get worse. Their international classification recognises four categories or stages of pressure ulcer and two categories of unclassifiable pressure injury. In the early stages of bedsores, the area may heal with relief of pressure and by applying care to the affected skin.
What Is A Pressure Injury
A pressure injury is an area of injured skin. A pressure injury happens when force is applied on the surface of the skin. This force can be a constant pressure on an area of skin or a dragging force between the skin and another surface. These injuries usually happen over bony parts of the body . A pressure injury can become life-threatening if it advances to a deep wound or becomes infected.
Read Also: Xeljanz Vs Entyvio For Ulcerative Colitis
Stage 4 Bedsore: What To Do Next
When a resident suffers from a stage 4 bedsore, it is often due to nursing home neglect. Fortunately, families have options if neglect or abuse has caused a stage 4 bedsore.
They can:
- Contact an ombudsman or Adult Protective Services
- Move their loved one to a hospital or another nursing home to recover
- Reach out to a lawyer to file a legal claim and pursue compensation
Over 17,000 lawsuits involving bedsores are filed each year. The best way to find out if you can sue for a stage 4 bedsore is to contact a nursing home abuse lawyer.
Get a free case review now to see what actions may be best for your case. You may be able to file a stage 4 bedsore lawsuit.
Pressure Ulcers Vs Bedsores
Pressure Ulcers are also known as Bedsores, Decubitus Ulcers, Pressure Sores, or Pressure Injuries. However, while Pressure Ulcers can develop during prolonged surgery or a hospital stay, a Bedsore generally develops on a person who has been immobile for long periods. It can be someone confined to a wheelchair or who cannot get out of bed.
Recommended Reading: Stomach Pain From Ulcerative Colitis
When To Get Medical Advice
If you’re in hospital or a care home, tell your healthcare team as soon as possible if you develop symptoms of a pressure ulcer. It’ll probably continue to get worse if nothing is done about it.
You should be regularly monitored and offered advice and treatment to reduce the risk of pressure ulcers, but sometimes they can develop even with the highest standards of care.
If you’re recovering from illness or surgery at home, or you’re caring for someone confined to bed or who is a wheelchair user, contact your GP surgery if you think you or the person you’re caring for might have a pressure ulcer.
Get medical advice immediately if there is:
- red, swollen skin
- pus coming from the pressure ulcer or wound
- cold skin and a fast heartbeat
- severe or worsening pain
- a high temperature
These symptoms could be a sign of a serious infection that needs to be treated as soon as possible.
When Should I Call The Doctor
If you suspect you have a pressure injury, speak with your doctor. A pressure injury is easier to heal if it is discovered in the early stages. It is important to prevent a wound from becoming infected. Healing is delayed in an infected wound and the infection could cause problems in other areas of the body.
You May Like: Foods To Avoid With Ulcers Mayo Clinic
Treatment Of Stage 3 And Stage 4 Pressure Ulcers
The goal of treatment for stage 3 and 4 pressure ulcers, is to properly debride and dress the wound cavity, create or maintain moisture for optimal healing, and protect the wound from infection. The goal of properly unloading pressure from the area still applies. At these pressure ulcer stages, more emphasis should be placed on proper nutrition and hydration to support wound healing. If the extent of the pressure ulcer or other factors prohibit it from healing properly, surgery may be necessary to close the wound.
The following precautions can help minimize the risk of developing pressure ulcers in at-risk patients and to minimize complications in patients already exhibiting symptoms:
- Patient should be repositioned with consideration to the individualâs level of activity, mobility and ability to independently reposition. Q2 hour turning is the standard in many facilities, but some patients may require more or less frequent repositioning, depending on the previous list.
- Keep the skin clean and dry.
- Avoid massaging bony prominences.
Diagnosing A Stage 4 Bedsore
A doctor determines the by its appearance. In the case of a stage 4 bedsore, the large wound has passed the bodys fatty tissue layer, exposing muscles, ligaments, or even bone.
In some cases, however, health care professionals may not be able to immediately diagnose a late-stage bedsore by examining it.
A stage 4 bedsore may be initially diagnosed as:
- UnstageableWhen a doctor cannot see the bottom of an open sore, they must clean it out to properly stage it.
- Suspected Deep Tissue Injury This diagnosis happens when the surface of a patients skin looks like a stage 1 or 2 sore, but it is actually affecting deeper tissues underneath.
Also Check: Can Ulcerative Proctitis Be Cured
Don’t Miss: How To Know If I Have Ulcerative Colitis
Wound Cleaning And Dressing
To heal, pressure sores need to be cleaned, dead skin needs to be removed , and dressings need to be applied.
The wound is cleaned when the dressing is changed. Health care practitioners often flood the wound, particularly its deep crevices, with saline to help loosen and clean away hidden debris.
A doctor may need to remove dead tissue with a scalpel, a chemical solution, a whirlpool bath , a special dressing, or biosurgery . Removal of dead tissue is usually painless, because pain is not felt in dead tissue. Some pain may be felt because healthy tissue is nearby.
Dressings Dressings Topical drugs are a mainstay of treating skin disorders. Systemic drugs are taken by mouth or given by injection and are distributed throughout the body… read more are used to protect the wound and promote healing. Dressings are used for some stage 1 pressure sores and all others. When the skin is broken, a doctor or nurse considers the location and condition of the pressure sore when recommending a dressing. The amount of drainage oozing from the sores helps determine which type of dressing is best.
What Are The Complications Of Bedsores
Once a bedsore develops, it can take days, months, or even years to heal. It can also become infected, causing fever and chills. An infected bedsore can take a long time to clear up. As the infection spreads through your body, it can also cause mental confusion, a fast heartbeat, and generalized weakness.
You May Like: How To Sleep With Stomach Ulcer
Can A Stage 4 Pressure Ulcer Be Prevented
Yes. Like many nursing home injuries, late-stage bedsores are largely preventable with proper care. They can be prevented by treating a stage 3 bedsore or avoiding a lower-stage bedsore from forming in the first place.
Nursing home staff can help prevent stage 4 bedsores by:
- Carefully monitoring earlier-stage bedsores to ensure they are healing
- Contacting health care providers if a patients wound is not improving
- Keeping residents mobile by walking and repositioning them
- Making sure residents have access to regular meals, water, and skincare
- Treating early-stage bedsores as soon as possible with proper wound care practices
Pressure Ulcers: What To Look For And Document About A Deep Tissue Injury
The professional staff at nursing homes and hospitals must conduct a comprehensive head-to-toe skin assessment on patients most at risk for developing decubitus ulcers. The skin may be compromised, requiring daily skin care to promote health.
Any detected bedsore should be fully documented in the residents healthcare plan to ensure they receive the best care for healing.
Documentation identifying a detectable pressure sore should include:
- The sores location
- The stage of the ulcer
- Pressure ulcers size, including its width, depth, and length, measured in centimeters
- Any identifiable sinus tract, tunneling, or undermining
- The presence of exudate , including its location, amount, and color
- The appearance and size of the wound bed, including a description of visible tissue
- A description of the sores edges, including any evidence of redness, rolled edges, maceration , or induration
- A description of the area surrounding the sore
- The absence or presence of pain
- The absence or presence of any foul odor
The nursing home team must ensure that patients most at risk for developing bedsores are moved at least once every 2 hours. If the patient is sitting in a wheelchair, chair, or recliner, they should readjust their body weight at least once every 15 minutes.
People highly susceptible to developing pressure sores need assistance from nurses, nursing aides, and licensed practical nurses to minimize the potential of falling and causing injury.
Donât Miss: Do Ulcers Cause Acid Reflux
You May Like: How To Find Out If You Have Ulcerative Colitis
Symptoms Of Pressure Ulcers
The parts of the body most at risk of developing pressure ulcers are those that are not covered by a large amount of body fat and are in direct contact with a supporting surface, such as a bed or a wheelchair.
For example, if you are unable to get out of bed, you are at risk of developing pressure ulcers on your:
- shoulders or shoulder blades
If you are a wheelchair user, you are at risk of developing pressure ulcers on:
- the back of your arms and legs
- the back of your hip bone
Recommended Reading: Is Ulcerative Colitis A Gastrointestinal Disease
Pressure Ulcer Staging And Prevention Guide
Pressure Ulcers represent a significant nursing care problem, and their prevention is an important perioperative nursing goal. Studies show that 17% to 29% of the general acute care population will develop a pressure sore during their hospital stay. Of patients with pressure ulcers that originated during their hospital stay, nearly one-quarter of those ulcers are triggered during their surgical procedure in the operating room. In this article you will learn:
- Pressure Ulcers vs. Pressure Injury: What’s The Difference?
- Pressure Ulcer Stages
- What is a Deep Tissue Pressure Injury
- Pressure injury causes and risk factors
- Pressure injury prevention devices
Don’t Miss: Herbal Treatment For Ulcerative Colitis
What Are Pressure Sores
Pressure sores are sores on your skin. Theyre caused by being in a bed or wheelchair nearly all the time. Sometimes theyre called bedsores or pressure ulcers. The sores usually develop over the bony parts of your body. Those are places with little padding from fat. Sores are common on heels and hips. Other areas include the base of the spine , shoulder blades, the backs and sides of the knees, and the back of the head.
People who need to stay in bed or in a wheelchair for a long time are at greater risk of developing pressure sores. This can include people who are paralyzed and those who arent able to get up on their own. But even some people with short-term illness and injuries can get pressure sores. Sores can happen if they have to stay in bed or a wheelchair while they heal. Lastly, some chronic diseases make it hard for pressure sores to heal. Those include diabetes and hardening of the arteries.
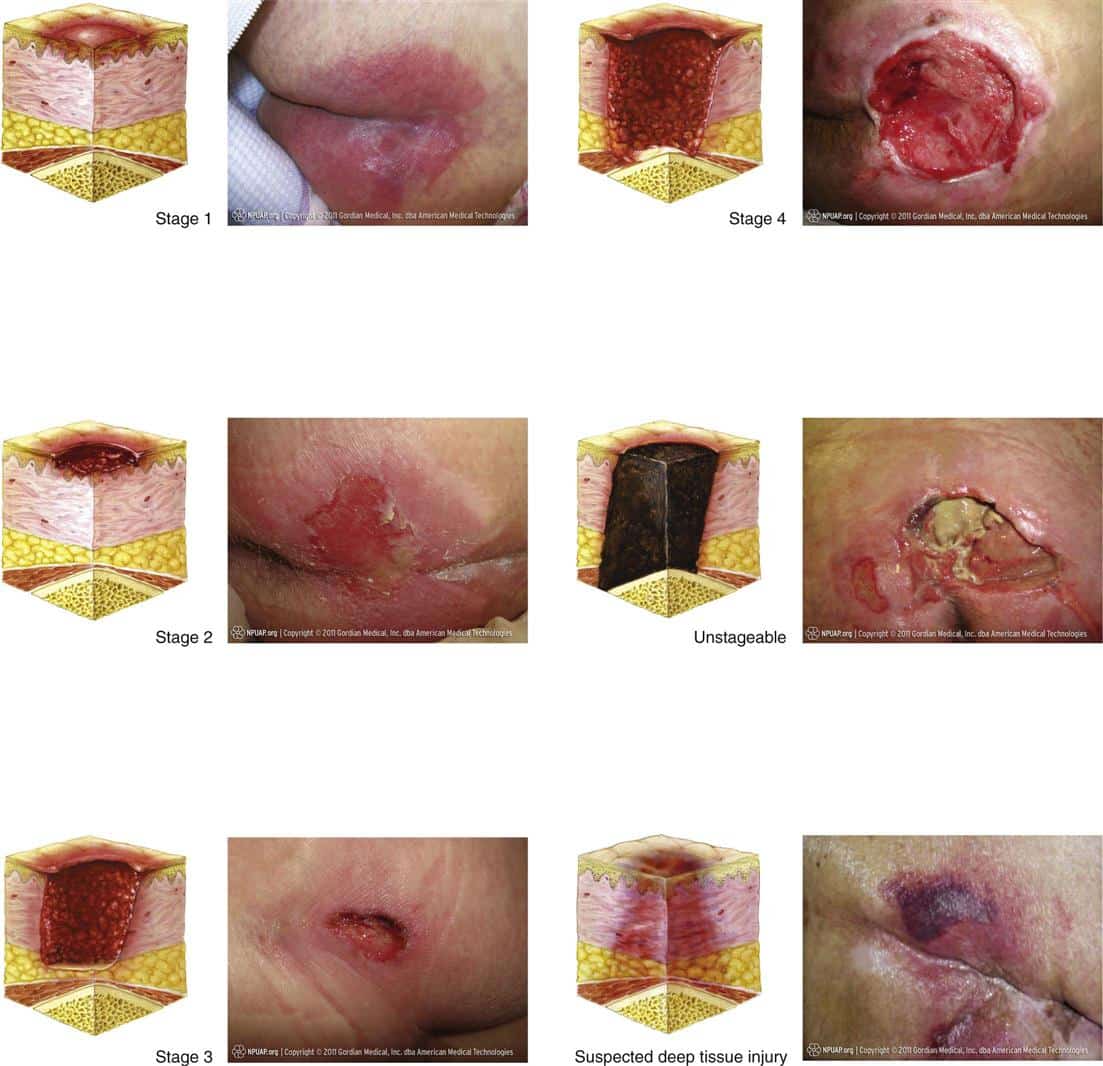
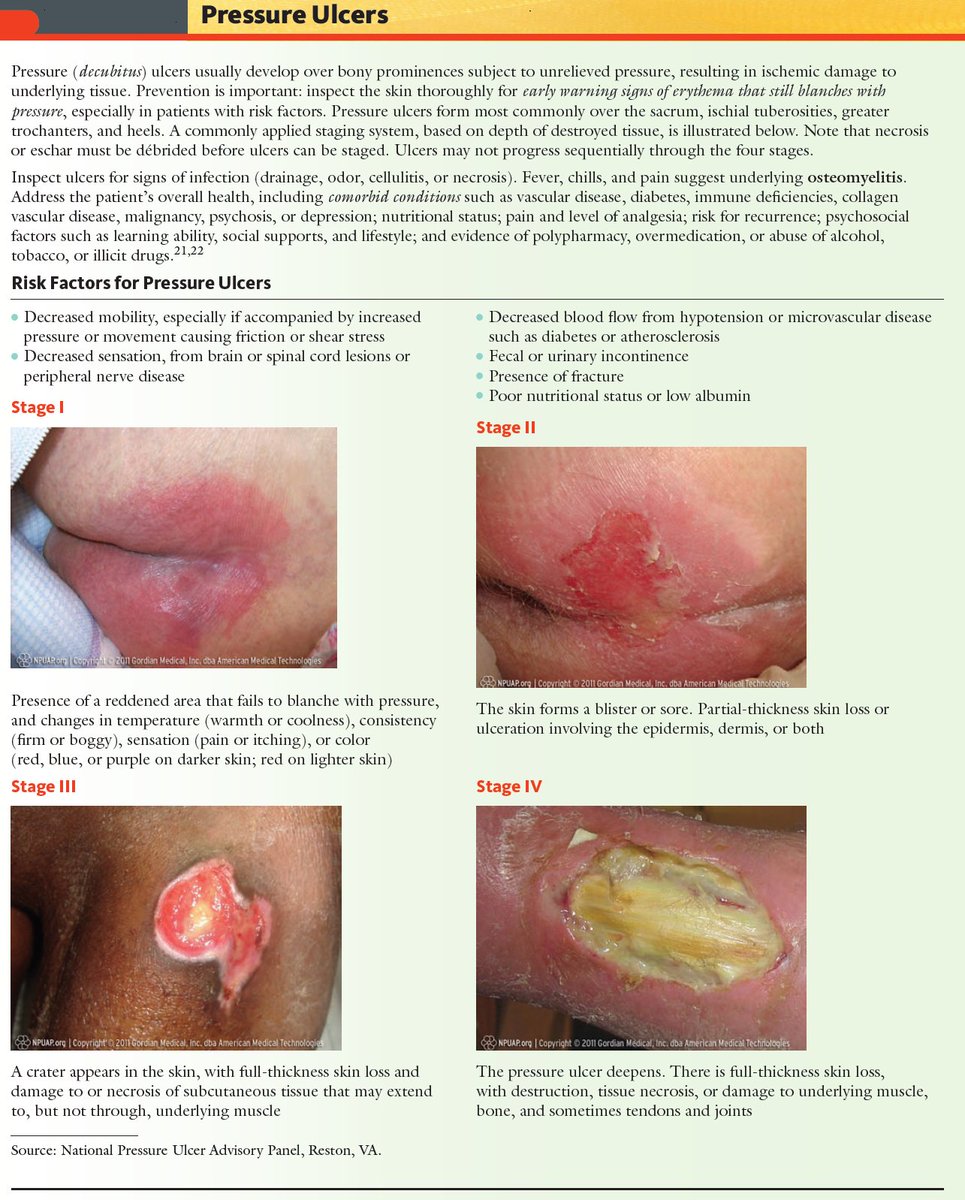
What Are The Stages Of A Pressure Sore
Pressure sores, also known commonly as bedsores or decubitus ulcers, are injuries to the body caused by sustained pressure. Their severity can be categorized according to four main phasesfrom a stage one ulcer where the skin is just beginning to show damage, to a stage four ulcer with open wounds, sores and signs of infection. Whatever the stage, all should be taken seriously and treated with urgency. Here are the four stages of a pressure sore.
Stage 1 Pressure Sores and Ulcers: Early on in pressure ulcer development, the skin is developing injury. While no open sores or broken skin are present yet, skin may appear redder, warmer or firmer than usual. Known as a non-blanchable erythema of intact skin, the color change may indicate the beginnings of a serious injury to the deep tissue.
Stage 2 Pressure Sores and Ulcers: This is where the true sore, or ulcer, develops as a break in the skin and an open sore. It is often very painful, and can create serious damage within the skin. Known as partial-thickness skin loss with exposed dermis, these bed wounds can quickly become something worse and may even present as a blood filled blister.
Stage 3 Pressure Sores and Ulcers: In stage three, the pressure ulcer has developed into the soft tissue underneath the skin. Known as full-thickness skin loss, this stage may show a deep wound, especially in an area with more adipose tissue.
Also Check: What To Take For Ulcers
Search Methods For Identification Of Studies
Four existing Cochrane Reviews were relevant to this NMA , and the protocol for this NMA complemented the protocols for these four reviews . We automatically included trials from these reviews in this NMA if they reported complete healing outcomes we planned to use the extracted data from these reviews where possible, supplementing if necessary which was required as some reviews had not been completed.
We conducted searches to identify relevant trials not covered by the four Cochrane Reviews as well as recently published trials. We crosschecked the identified trials against those in the 2014 NICE guideline and the 2013 US Agency for Healthcare Research and Quality guideline on treating pressure ulcers to further locate any additional trials we also checked the references of 24 systematic reviews identified by our search.
Electronic searches
We searched the following electronic databases to identify reports of relevant randomised clinical trials:
- the Cochrane Wounds Specialised Register
- the Cochrane Central Register of Controlled Trials
We also searched the following clinical trials registries:
- ClinicalTrials.gov
Searching other resources
Bed Sore Stages With Pictures
Understanding bed sore stages is important to keeping your loved one safe. Why? depending on the stage, bed sores may be a non-blanchable area of the skin or a massive hole in the body. It all depends on the stage. Using the bed sore stages pictures on this site can help. Please note that this site cannot substitute for proper medical advice.
Recommended Reading: What Causes Stomach Ulcers To Flare Up
What Are The Stages Of A Pressure Injury
There are four stages that describe the severity of the wound. These stages include:
- Stage 1: This stage is discolored skin. The skin appears red in those with lighter skin tones and blue/purple in those with darker skin tones. The skin does not blanch when pressed with a finger.
- Stage 2: This stage involves superficial damage of the skin. The top layer of skin is lost. It may also look like a blister. At this stage, the top layer of skin can repair itself.
- Stage 3: This stage is a deeper wound. The wound is open, extending to the fatty layer of the skin, though muscles and bone are not showing.
- Stage 4: This stage is the most severe. The wound extends down to the bone. The muscles and bone are prone to infection, which can be life-threatening.
Preventing Stage 2 Bedsores

The best way to prevent stage 2 bedsores is to identify stage 1 bedsores and treat them before they worsen. Stage 1 bedsores have not broken the skin and usually look like reddish or discolored spots on the body. Stage 1 bedsores usually can be cured within a few days while stage 2 bedsores can take a few weeks to heal.
Nursing home attendants and nurses should regularly check residents at risk for signs of developing bedsores. Caretakers should check patients skin from head to toe. These skin assessments should take place at least once a day.
Patients who are at high risk of developing bedsores should be checked as often as is reasonable. Those at risk are often elderly or have a health condition that limits their mobility. People are at higher risk of developing bedsores if they use a wheelchair, spend a lot of time in bed, or need assistance to move. Conditions that can raise the risk of developing sores include mental conditions like alzheimers and physical conditions like paralysis.
Read Also: Mouth Ulcer On Tongue Causes