How Does Ulcerative Colitis Affect Your Stool
Changes in stools are directly related to how UC affects your colon and rectum. In UC, the immune system attacks healthy cells in the digestive tract. The attack increases white blood cells in your colon and rectum, and repeated attacks lead to chronic inflammation.
Inflammation causes your colon to contract and empty frequently, which is why you may experience frequent diarrhea and urgent bowel movements.
When inflammation destroys the cells lining your colon, sores or ulcers can develop. These ulcers can bleed and produce pus, resulting in bloody diarrhea.
Some people with UC also have constipation, but this isnt as common as diarrhea. Constipation typically occurs when inflammation is limited to the rectum. This is known as ulcerative proctitis.
Other symptoms related to ulcerative colitis include abdominal pain, painful bowel movements, fatigue, anemia, weight loss, and fever.
Symptoms Of Ulcerative Colitis
Some people with ulcerative colitis have only occasional symptoms. For others, the symptoms are constant. The symptoms a person experiences can vary depending on the severity of the inflammation and where it occurs in the large intestine.
Common symptoms include:
- diarrhea, often with blood and mucus
- cramping abdominal pain, especially in the lower abdomen
- a frequent sensation of needing to have a bowel movement
- little advance warning before a bowel movement
- the need to wake from sleep to have bowel movements
- feeling tired
- dehydration
- low red blood cell count
Some people with ulcerative colitis develop pain or soreness in the joints, irritated eyes, and rashes.
The symptoms of ulcerative colitis can suddenly get worse. This is called a flare. Then symptoms may fade away. This is called remission. Some individuals with ulcerative colitis have symptoms only rarely, others have flares and remissions, others have symptoms all or most of the time.
Clinical And Demographic Data
All participants were asked to provide the following demographic data: sex, age,ethnicity, marital status, educational level, tobacco and alcohol use, andweight and height , which were used to calculate bodymass index . We also asked participants to complete a checklist ofmedications previously reported as being implicated in the development of MC, and to respond to questions regarding the presence of common autoimmunediseases associated with MC, including coeliac disease, thyroid disease, rheumatoid arthritis,psoriasis, autoimmune hepatitis, and type 1 diabetes. Patients were asked toreport their stool frequency, as well as if they had ongoing GI symptoms thatthey attributed to MC. The latter was recorded as a dichotomized outcome aseither yes or no.
IBS-type symptoms, according to the Rome III criteria, included abdominal pain or discomfort occurring at least 3 days per monthover the past 3months, with the onset of discomfort at least 6monthspreviously, associated with two or more of the following: an improvement of painor discomfort with the passage of stool, more or less frequent stools, or looseror harder stools.
Don’t Miss: How To Treat Skin Ulcer On Leg
Feeling Chills And Ibd
Not every symptom of Crohns disease and ulcerative colitis is gastrointestinal-related. Although many of these conditions symptoms affect the digestive tract and bowel, other common symptoms are extraintestinal, meaning they affect other parts of the body. In addition to abdominal pain, cramping, bloating, diarrhea, and weight loss, people with inflammatory bowel disease can experience chills.
Its important to contact your doctor if youre experiencing fever and chills, especially if the symptoms intensify over time. Fever and chills could be a sign of a medication allergy or that your IBD is becoming more severe.
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
Read Also: How To Use Aloe Vera Gel For Ulcerative Colitis
Does Ulcerative Colitis Shorten Your Life
Most people with this condition can have a full life expectancy. However, complications can increase the risk of an early deathTrusted Source , according to one 2003 Danish study. Very severe ulcerative colitis could impact your life expectancy, especially within the first couple of years after your diagnosis.
How Can Fatigue Affect You
If you experience fatigue with your UC, you might notice that you have a hard time performing physical activity, your memory and concentration might be impacted, and you might be more emotional than normal. If you feel like your brain is foggy, you’re experiencing fatigue. But not all hope is lost use the following tips and tricks to help combat your fatigue.
Recommended Reading: What Are The First Signs Of A Stomach Ulcer
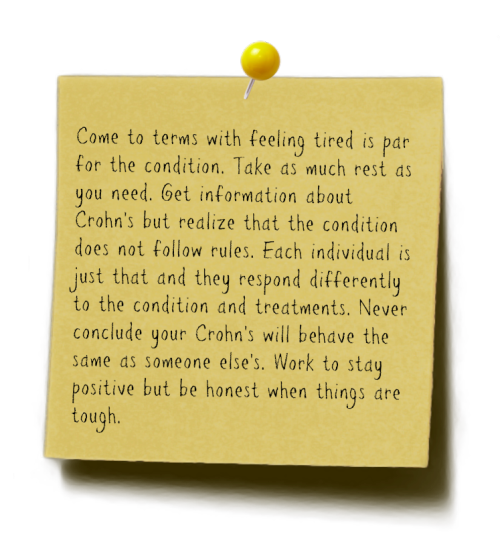
Many Of Those Who Suffer From Inflammatory Diseases Such As Crohn’s Disease And Ulcerative Colitis Also Struggle With Fatigue
True fatigue is something that can be hard for those who dont have it to understand.
Clinically speaking, fatigue is an overwhelming sense of tiredness, exhaustion and lack of energy. Its exhaustion that doesnt disappear after rest or sleep.
Many people describe it as feeling like their battery is completely discharged. They cant manage to do anything at all, says Katrine Brække Norheim at Stavanger University Hospital.
They may also have brain fog, which means they have difficulty concentrating, forget what they are doing and find it difficult to absorb information.
In recent years it has become clear that fatigue is a major aspect of different inflammatory diseases, such as lupus, arthritis, psoriasis and inflammatory bowel diseases , including Crohn’s disease and ulcerative colitis.
Now Norheim and her colleague Tore Grimstad have conducted a review of the research on fatigue in patients with IBD.
Their conclusion is that fatigue is a significant and often underestimated aspect of these illnesses. They also say we need to know more about the mechanisms behind the phenomenon, to find new treatment options.
Underdiagnosed and undertreated
The two researchers looked at 28 different studies of fatigue and IBD, and concluded that people with the diseases experience extreme exhaustion much more frequently than normal.
While 2 to 12 per cent of the general population reports being fatigued, fatigue affected between 22 and 77 per cent of IBD patients.
Sickness Behaviour
How To Deal With Gas And Bloating Related To Ibd
Many people who have inflammatory bowel disease also find that they have symptoms of abdominal bloating or distention. One cause of this uncomfortable problem may be gas in the digestive tract.
Bloating and gas can be painful, embarrassing, and might limit your wardrobe choices to pants and skirts with elastic waistbands. Fortunately, there are several ways to deal with a bloated stomach.
Also Check: Mouth Ulcer On Tongue Remedies
Read Also: Natural Ways To Heal Ulcerative Colitis
Why Does Colitis Make You So Tired
Anaemia, a common complication of Crohns or Colitis, may worsen fatigue. People with anaemia carry less oxygen in their blood, which can mean they easily become exhausted. Low vitamin D levels may also contribute to fatigue. Vitamin D is important for keeping your bones, muscles and immune system healthy.
Also Check: Can I Take Imodium If I Have Ulcerative Colitis
About Our Health Information
At Bupa we produce a wealth of free health information for you and your family. This is because we believe that trustworthy information is essential in helping you make better decisions about your health and wellbeing.
Our information has been awarded the PIF TICK for trustworthy health information. It also follows the principles of the The Information Standard.
Also Check: What Are Infusions For Ulcerative Colitis
Are Potatoes Ok For Ulcerative Colitis
Avoid all raw or undercooked vegetables, including corn. Its fine to consume canned vegetables and potatoes, as long as the skin has been discarded. Try pureed vegetable soups for an easy way to digest vegetables. Vegetables provide many important nutrients and its important to incorporate them in your diet.
Dont Miss: Preventing Pressure Ulcers In Nursing Homes
When To Get Medical Advice
You should see a GP as soon as possible if you have symptoms of ulcerative colitis and you have not been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms.
If necessary, they can refer you to hospital for further tests.
If you have been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact a GP or your care team for advice.
You may need to be admitted to hospital.
If you cannot contact your GP or care team, call NHS 111 or contact your local out-of-hours service.
Read Also: Artificial Sweeteners And Ulcerative Colitis
Seeking Relief From Crohns Disease Symptoms
People with Crohns disease are familiar with symptoms like abdominal pain and cramping. Even with a solid treatment plan, there are a number of reasons you might feel pain and discomfort with Crohns disease, says Vijay Yajnik, MD, a gastroenterologist and an assistant professor of medicine at Harvard Medical School in Boston. These include:
- Ongoing inflammation
- Swelling caused by narrowing or blockages in the intestine
- Cracks and tears in membranes in the intestines
- Your level of sensitivity to gut pain
- Perceptions of pain that may be rooted in the stress of managing Crohns disease
Whatever the cause, its important to find strategies to help you feel better. This might go beyond prescription medications to trying home remedies and other tactics that could help you gain more complete relief from Crohns disease symptoms. Consider discussing these seven ways to find relief with your doctor as part of your overall Crohns disease treatment plan.
Should You Stop Taking Your Ibd Medication
First of all, do not make any changes to your medication regimen without first talking to your doctor.
According to the ACG, keeping IBD well-controlled or in remission may help protect you from contracting COVID-19.
Right now the real hotspots for spread of this infection are in health care settings, says Dr. Ungaro. If your condition is well-controlled and you stop taking your usual medications, you risk having a flare. We do not want patients to have a flare in the midst of this pandemic and end up in the ER where they could be exposed .
If youre using steroids: Topical steroids, which are taken via suppositories or enemas, are unlikely to cause problems. Systemic steroids, however, are another story. If youre on oral steroids, now is a good time to start tapering off them if you can, says Dr. Ungaro, but do not stop taking steroids cold turkey. Call your gastroenterologist, discuss whether it is a good idea for you to start decreasing your dose, and find out how to do so slowly and safely.
If youre using aminosalicylates, biologics, or immunomodulators: If youre doing well on a drug in one of these classes, stick with it, says Dr. Morganstern. If you stop, youre at risk of flaring.
One exception, however, may be for patients who are stable and taking both an immunomodulator and a biologic. If someone is in remission on combination therapy, I might try removing the immunomodulator and keeping the biologic, says Dr. Morganstern.
Read Also: How Can You Tell You Have An Ulcer
What Are The Symptoms Of Ibs
-
Bloating and gas
-
Diarrhea, especially after eating or first thing in the morning
-
Feeling a strong urge to have a bowel movement
-
Feeling like you still need to have a bowel movement after youve already had one
-
Stomach pain and cramping that may go away after having a bowel movement
The symptoms may get worse when youre under stress, such as when you travel, attend social events, or change your daily routine. Your symptoms may also get worse if you dont eat enough healthy foods or after youve eaten a big meal. Some people are bothered by certain foods. Women who have IBS may notice more frequent symptoms during their periods.
Read Also: What To Eat If You Have Peptic Ulcer
Tips For Managing Fatigue
- Keep a close eye on those blood testsChecking on iron levels, vitamin B12 and other chemical or nutrient deficiencies can help your treatment team to find the right mix of medication for you. Adding iron supplements or reducing the dosage of a medication can make a world of difference to energy levels for some people.
- Focus on keeping fitWhile being careful not to overstress yourself, try gradually increasing the amount of physical activity you do. Make use of a gym membership, walk rather than catching the bus for shorter trips, or commit to a team sport. Improving your overall fitness can ensure your energy stores are higher, potentially reducing the impact of those fatigue-ridden days.
- Assess your dietDo you have any foods that make you feel heavier, or sluggish? Complex carbohydrates such as cereals or porridge can provide you with energy over a longer time frame, while simple carbohydrates will give you a short burst of energy, often followed by a low. Consider if you are getting a good mix of fruits and vegetables, carbohydrates for energy, and rich protein.
- Manage your workloadWherever possible, ensure your workplace, family or education provider is aware of your condition and see what flexibility is available with responsibilities, work hours and prior planning. For example, taking the afternoon off following a doctors appointment may be a welcome break to rest, recover and prepare for the next week.
You May Like: Coconut Milk Good For Ulcerative Colitis
How Is Ulcerative Colitis Diagnosed
To diagnose ulcerative colitis in children, teenagers and adults, your healthcare provider has to rule out other illnesses. After a physical exam, your provider may order:
- Blood tests: Your blood can show signs of infection or anemia. Anemia is a low level of iron in your blood. It can mean you have bleeding in the colon or rectum.
- Stool samples: Signs of infection, parasites , and inflammation can show up in your poop.
- Imaging tests: Your healthcare provider may need a picture of your colon and rectum. You may have tests including a magnetic resonance imaging scan or computed tomography scan.
- Endoscopic tests: An endoscope is a thin, flexible tube with a tiny camera. Specialized doctors can slide the endoscope in through the anus to check the health of the rectum and colon. Common endoscopic tests include colonoscopy and sigmoidoscopy.
Get Support For Your Ibd Today
MyCrohnsAndColitisTeam is the social network for people diagnosed with IBD and the people who love, support, and care for them. More than 142,000 members come together to ask questions, give advice, and share their experiences of life with IBD.
Have you experienced chills with Crohns disease or ulcerative colitis? Share your experience in the comments below or by posting on MyCrohnsAndColitisTeam.
Also Check: Can Ulcerative Colitis Cause Cancer
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
The Difference Between Ulcerative Colitis And Crohn’s Disease
Crohn’s disease is also an inflammatory bowel disease . The 2 diseases affect the digestive tract differently:
- Ulcerative colitis only affects the large bowel , and inflammation is only in the surface layers of the bowel lining. It causes ulcers to form in the lining of the bowel.
- Crohn’s disease can affect any part of the digestive tract, from the mouth to the anus , but usually just the last section of the small bowel and/or the colon. Inflammation can extend into the entire thickness of the bowel wall.
You May Like: How To Stop An Ulcerative Colitis Flare
The Intensity Of Your Symptoms Might Vary Over Time
The most common ulcerative colitis symptoms are diarrhea containing blood or pus and abdominal pain, the National Institute of Diabetes and Digestive and Kidney Diseases says. Theres a lot of cramping, Cristal Steuer, 38, who was diagnosed with ulcerative colitis while she was in college, tells SELF. You might also experience things like fatigue, fevers, nausea, unintended weight loss, joint pain, and rashes. Whichever symptoms you do have, they may wax and wane, the NIDDK explains. You may have periods when youre in remission interspersed with periods when your symptoms are worse. But some people experience constant symptoms from ulcerative colitis.
Just because you can’t see it doesn’t mean that it’s not hard every single day, Tatiana Skomski, 26, who was diagnosed at 21 after years of unexplained fatigue and pain when an especially bad flare-up nearly caused her to bleed to death, tells SELF.
I’ve had to increase my tolerance for what is a background level of pain, Sam, 22, who was diagnosed with ulcerative colitis in the summer of 2019, tells SELF. I’ll have sharper moments where I can’t functionbut for the most part, it’s more like a constant level of chronic pain.
If pain or other ulcerative colitis symptoms are really interfering with your life, make sure your health care provider knows so that you might be able to tweak your treatment plan if necessary.
Most Symptoms Of Ulcerative Colitis Relate To Bowel Movements
The symptoms of ulcerative colitis can vary from person to person, based on where the disease is in the body and how bad the inflammation is.
Most common symptoms:
- Diarrhea , which is often the first symptom.
- Blood in the stool.
- Urgency, or immediate need, to go to the bathroom.
- Increased number of bowel movements.
- Belly pain and cramping.
Ulcerative colitis can cause symptoms throughout your body.
You might have weight loss or other symptoms that affect the entire body. The inflammation of ulcerative colitis can also affect your joints or skin, leading to painful joints and skin rashes. During a flare-up, symptoms may go beyond those that affect the digestive system, including:
- Rashes or patches of red, swollen skin.
- Painful or swollen joints.
- Mouth ulcers.
- Red, irritated eyes.
Keep of track of any symptoms, how often you have them, and how bad they are to talk about with your health care provider.
Read Also: Natural Treatment Of Ulcer In Hindi