What To Do During A Flare
Medications are used to manage flares and induce remission as quickly as possible.
Doctors may prescribe a corticosteroid , antibiotic, 5-aminosalicylate, immunomodulator or biologic.
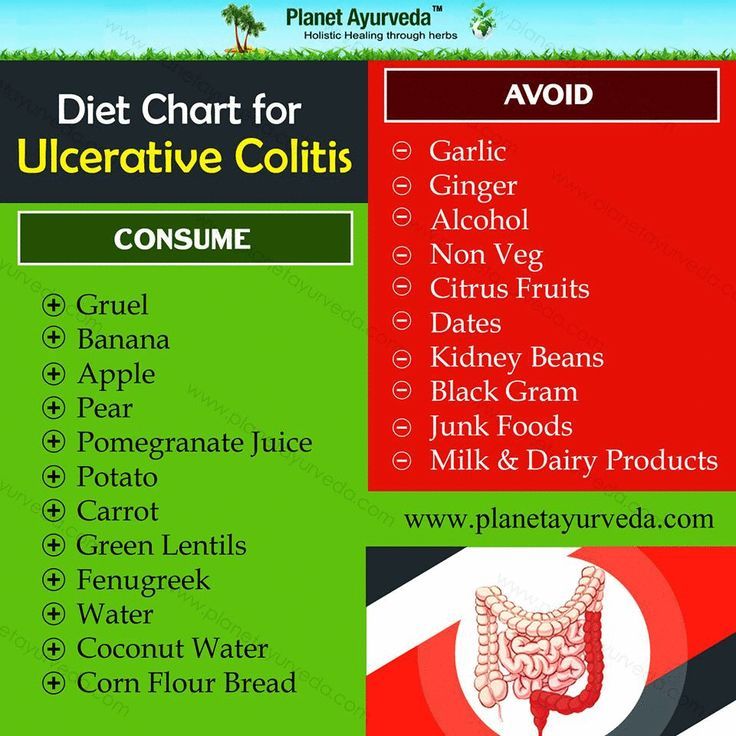
In addition, certain diet changes may help shorten flares. Some tips to keep in mind:
- Keep a food and symptom journal during flares to identify bothersome foods. This also ensures that foods are not avoided without cause.
- Eat small, more frequent meals as opposed to 3 large meals in a day .
- Ask your doctor whether to limit fiber until symptoms pass. Eating a maximum of 10 grams of fiber per day may reduce irritation and lower the risk of intestinal blockage. Once you are in remission, gradually increase your fiber intake, depending on how much you can tolerate, until you reach the recommended daily intake of 2530 grams.
- Drink plenty of fluids to avoid dehydration.
What Causes Ulcerative Colitis
The cause of ulcerative colitis is unknown but it is believed to be caused by a combination of several factors including an overactive immune system, genetics, and the environment.
- Overactive immune system: It is believed that in ulcerative colitis, the immune system is triggered to mistakenly attack the inner lining of the large intestine, causing inflammation and symptoms of ulcerative colitis.
- Genetics: Ulcerative colitis can run in families. The genetic link is not entirely clear but studies show that up to 20% of people with ulcerative colitis have a close family member with the disease.
- Environment: Certain environmental factors including taking certain medications , and eating a high-fat diet may slightly increase the risk of developing ulcerative colitis.
Physical or emotional stress and certain foods do not cause ulcerative colitis, however, they may trigger symptoms in a person who has ulcerative colitis.
Olive Oil Coconut Oil Omega
Fat is an important component of a balanced diet. A good quality olive oil is best for sautéing over low heat and making cold dressings or sauces.
Coconut oil is worth trying, especially if you have a difficult time digesting fat. As a medium-chain triglyceride, its more easily and more completely digested without the help of bile salts than other plant oils. For that reason, it can be a good oil for people with malnutrition and malaborption problems.
Coconut is solid at room temperature, so it is versatile and can be used like butter for both sautéing over high heat and for baking.
Omega-3 fats are important because we cannot make them in our body. They are found in nuts, avocadoes, freshly ground flaxseed, and fish. Wild salmon and sardines are preferable to other fish as a source of omega-3s because of their low heavy metal content.
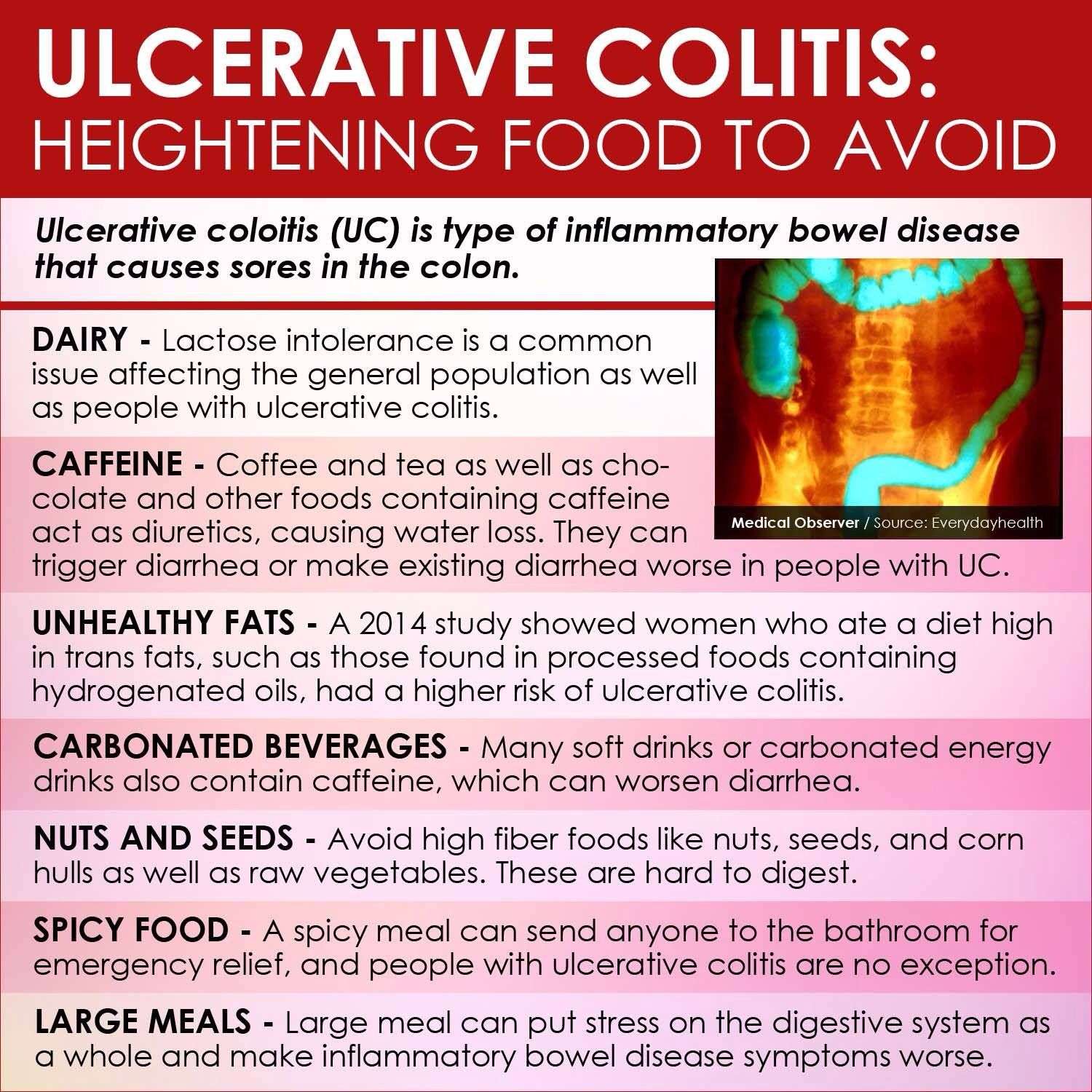
Artificial trans fats should be avoided altogether because it increases the risk of developing heart disease. Trans fat is used to make crackers, cookies, and other processed food because it extends the shelf life.
Don’t Miss: Colon Surgery For Ulcerative Colitis
What Side Effects Of Ibd Can Cause Malnutrition
There are several reasons why people with IBD may be at risk for malnutrition. The following list includes some side effects that contribute to malnutrition.
- Inadequate food/fluid intake may by caused by nausea, abdominal pain, loss of appetite or altered taste sensation
- Increased losses â intestinal inflammation during acute flares results in increased protein losses, losses from fistula fluids, diarrhea and bleeding
- Increased nutritional needs â inflammation or infection increases metabolic requirements
- Malabsorption with Crohns disease may be caused by severe intestinal inflammation, resection of small intestine and medications, such as prednisone and sulfasalazine
The Best Diet For Ulcerative Colitis: Splitting Fact From Fiction
Many people claim to have cured ulcerative colitis with diet or supplements.
Unfortunately, there is no diet or pill that can cure the disease.
However, certain diet changes have shown tremendous promise in reducing symptoms and easing discomfort, helping patients live a normal life once more.
This article explains what we currently know about the role of diet in ulcerative colitis.
Contents
Recommended Reading: What Can You Eat With A Peptic Ulcer
How A Professional Can Help
Living with ulcerative colitis can be frustrating, and its better if you dont have to go at it alone. Working with a gastroenterologist and a registered dietitian can help. Medications can ease symptoms, and diet changes can help to control flares. Its especially important to include a registered dietitian if youre trying an elimination diet since they will work with you to prevent any nutritional deficiencies.
Since everyone with UC has different triggers, figuring out what works best for youand the trial and error that goes along with itwill be much easier with the help of health professionals.
The Ulcerative Colitis Diet
1. Omega-3 Fatty Acids
Studies have found that an omega-3 fatty acid called eicosapentaenoic acid has the power to fight inflammation. It blocks certain chemicals in your body called leukotrienes. A benefit of fish oil is its a good source of EPA, and in some tests, people benefited from very high doses of it.
A 2010 case report published in the Journal of the Royal Society of Medicine evaluated a 38-year-old woman who had ulcerative colitis and used omega-3 fatty acids as part of her treatment. In 1998, at the age of 27, she went to the emergency department after 10 days of bloody diarrhea and lower abdominal cramping pain. She described up to 15 bowel motions daily with urgency, and she lost approximately six pounds. She was also clinically dehydrated.
After weeks of various treatments that only led to short-term results, the patient turned to omega-3 fatty acid treatments. The EPA and DHA doses were well-tolerated and had no side effects. Her bowel frequency slowly decreased, and within a week all rectal bleeding had resolved. The woman continued to take one gram of omega-3s and 2.4 grams of mesalazine, an anti-inflammatory medication that did not have the same reactions when given alone. The patient went into remission after adding omega-3s into her diet.
2. Probiotics
3. Iron-Rich Foods
4. Folate-Rich Foods
5. Turmeric
Read Also: Wound Treatment For Diabetic Foot Ulcers
Choose Fish With Omega
Scientists have not yet come to a consensus about whether or not eating red meat has any effect on people with UC, but the nutrients in fish could be beneficial. Consuming foods like fatty fish, which are rich in omega-3 fatty acids, may help with UC-related inflammation, says Diekman.
Omega-3 fatty acids are a crucial nutrient your body uses to make cells and hormones that regulate blood clotting. While some studies have shown that omega-3 fatty acids are anti-inflammatory, more research still needs to be done to prove theyre beneficial. According to the National Institutes of Health , omega-3 fatty acids, like probiotics, also support the immune system.
Unlike other fats, the body cant make this good fat on its own from other raw materials. Instead, you must get it from food sources, including fish like salmon, herring, sardines, rainbow trout, and mackerel just refrain from frying fillets, since fatty or greasy foods can exacerbate UC symptoms.
Instead, try baking or grilling fish, or try this recipe for UC-friendly salmon chowder.
Also remember that its especially important to make sure youre eating enough protein immediately after a flare-up to replace any lost nutrients and reduce the risk of anemia.
But Isnt Ulcerative Colitis Incurable
The vast majority in the mainstream say ulcerative colitis is incurable. I believe that UC is so difficult to heal that it might as well be incurable. But that difficulty has a lot to do with what sacrifices were willing to make and what were willing to do to heal.
Its taken me years to heal and the complete dismantling of my old life on every level.
To a large extent, most people arent able or willing to make the choices I have for their health.
Healing ulcerative colitis naturally requires 100% dedication and a lot of painful sacrifice.
Ive had to become a different person from who I was before I got sick.
Also Check: Left Sided Ulcerative Colitis Cancer Risk
I Have Heard That Fiber Is Good For Ulcerative Colitis What Does Onpoint Say
-
We encourage you to eat a medium/high fiber diet when you are not experiencing a flare up. A high fiber diet is almost always encouraged in all adults, part of maintaining a healthy gut as well
-
If you decide to increase your fiber intake, increase it gradually, even if you are not having GI or IBD issues presently
-
You may find a Low Residue approach helpful. We have seen it work well for some people
-
Increase or be aware of hydration and fluid intake. Try to drink at least 64 oz of water per day
-
Some studies show that a higher fiber diet can improve IBD conditions
What Can I Eat During Remission
When your UC is in remission, your instinct might be to reach for foods that are normally off-limits during a flare. But its still best to stick with generally trigger-free fare.
I would advise someone to eat plenty of diverse vegetables and fruits and consider following an anti-inflammatory style diet or Mediterranean diet, says Dr. Singh.
Though, fiber, in its many forms, may be better tolerated during remission, says Freuman. Go for the raw veggies, eat the salad, have a handful of whole nuts, or leave the skin on your fruits and vegetables, she says.
That said, Freuman adds that some people find that these types of foods bother them even in remission, and thats perfectly okay. Its not worth suffering or making yourself sick to push beyond the comfortable limits of tolerance, notes Freuman.
Ultimately, she encourages her clients to eat the greatest variety of plant-based foods they can comfortably tolerate as the foundation of their diets.
Also Check: Can Ulcerative Colitis Cause Low Testosterone
Foods To Fight Ulcerative Colitis
- Salmon The essential fatty acids in salmon will help counterbalance an inflammation flare-up.
- Cultured Yogurt Cultured yogurt contains probiotics, beneficial bacteria necessary for maintaining a healthy gastrointestinal tract.
- Squash The antioxidants Beta-carotene, vitamin A, and vitamin C in squash will help repair damage done by inflammation.
- Egg Whites Rich in B vitamins and a great source of protein, eggs whites are often well tolerated by people with ulcerative colitis and may help reduce inflammation.
- Honeydew Melon Honeydew melon will help soothe the lining of your colon.
- Avocados Studies have found that 85% of people with inflammatory bowel disease are malnourished. Avocados are a great source of calories, healthy fat, and protein. Theyre also easily digested by the body.
- Instant Oatmeal Instant oatmeal is more processed than steel cut oatmeal, making it easier to digest for people who have ulcerative colitis.
- Turkey For a healthy intake of protein, try turkey and other lean meats like skinless poultry and lean pork loin. The unsaturated fat in other meats may trigger a symptom flare-up.
What Should I Eat If I Have Ulcerative Colitis
If you have ulcerative colitis, you should eat a healthy, well-balanced diet. Talk with your doctor about a healthy eating plan.
Ulcerative colitis symptoms may cause some people to lose their appetite and eat less, and they may not get enough nutrients. In children, a lack of nutrients may play a role in problems with growth and development.
Researchers have not found that specific foods cause ulcerative colitis symptoms, although healthier diets appear to be associated with less risk of developing IBD. Researchers have not found that specific foods worsen ulcerative colitis. Talk with your doctor about any foods that seem to be related to your symptoms. Your doctor may suggest keeping a food diary to help identify foods that seem to make your symptoms worse.
Depending on your symptoms and the medicines you take, your doctor may recommend changes to your diet. Your doctor may also recommend dietary supplements.
Read Also: Ulcerative Colitis Lower Back Pain
What Is Uc Again And Why Does Diet Matter
If youre reading about UC and diet, you probably have some of the basics already down but just in case this is all new to you: Ulcerative colitis causes chronic inflammation in the colon and rectum, triggering frequent and urgent diarrhea, bloody stools, and abdominal pain and cramping.
Its not just a poop problem though. It can lead to nutrient deficiencies, actual malnutrition, and weight loss along with body-wide inflammation, which can spur joint pain, fatigue, and more. And these are all issues that can be influenced for better or worse by what you eat .
Whats tricky, though, is that theres no specific ulcerative colitis diet.
In fact, there isnt even a set list of trigger foods that applies to every single person with UC.
Just like everyones specific set of UC symptoms is unique, so too are their problem foods. So, what the heck are you supposed to do with that? Find yourself a guide, thats what.
The best way to figure out how to make your diet work for your UC is to seek the advice of a registered dietitian. Ask your gastroenterologist if they can refer you to an R.D. they trust.
In the meantime, get up to speed on which foods do commonly worsen symptoms in people with UC, along with what goes into a healthy diet in general. While you cant manage UC with diet alone, arming yourself with this knowledge can be a key piece of the puzzle.
Energy And General Health
If youre following a restricted or relatively bland diet to help cope with a flare of ulcerative colitis symptoms, or youre on a liquid-only diet as your body heals from surgery, you may be getting fewer calories and nutrition. As a result, you might not have as much energy as you typically do.
Its important that you try your best to eat enough each day to meet your bodys nutrition and energy needs. Not only to help manage ulcerative colitis but to maintain your overall health.
Complications from IBD, such as infections, may be more likely if your body is weakened from malnourishment, vitamin deficiencies, and dehydration.
Preventing nutritional deficiencies may help prevent flares: In 2017, research from Beth Israel Deaconess Medical Center indicated that people with ulcerative colitis who are in remission may be more likely to experience a relapse of symptoms if they are deficient in vitamin D.
Don’t Miss: What Are The Side Effects Of An Ulcer
What Should I Eat
Its not always easy knowing what foods best fuel your body, especially when you have Crohn’s disease or ulcerative colitis. Your diet and nutrition are a major part of life with inflammatory bowel disease , yet there is no single diet that works for everyone.
Nutrition affects not just your IBD symptoms, but also your overall health and well-being. Without proper nutrients, the symptoms of your Crohns disease or ulcerative colitis can cause serious complications, including nutrient deficiencies, weight loss, and malnutrition.
We have several tips for a healthy diet thats well-balanced and nutrient rich. These tips are for educational purposes only. You should work with your doctor or a dietitian specializing in IBD to help you develop a personalized meal plan.
Watch our with Emily Haller, registered dietitian at Michigan Medicine! Tune in to hear Emily review diet facts, debunk myths, speak about restrictions, and highlight ongoing research.
Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms can vary, depending on the severity of inflammation and where it occurs they typically develop over time. Most people experience mild to moderate symptoms, but the course of ulcerative colitis may vary and some people have long periods of remission. The symptoms depend on the location of the disease-causing inflammation. If you have ulcerative colitis, you may have the following signs and symptoms:
- Diarrhea, often with blood or pus
- Abdominal pain and cramping
- An increased risk of blood clots in veins and arteries
Don’t Miss: Foods To Avoid With Ulcers Mayo Clinic
Which Nutrients Are Important In Crohns And Colitis
Vitamins and mineralsYour body needs vitamins and minerals to work and stay healthy. Your Crohns or Colitis may stop you absorbing enough vitamins and minerals from your food. Vitamins and minerals that you may not absorb properly include iron, vitamin B12, vitamin D and calcium.Eating a healthy, balanced diet may help improve the level of vitamins and minerals in your body. If blood tests show you have low levels of vitamins and minerals, your doctor or specialist nurse may recommend you take supplements to restore your vitamin and mineral levels.Speak to your doctor, specialist nurse or dietitian if you think you may have low levels of any of these nutrients.
IronHaving low levels of iron is common in people with Crohns or Colitis. Possible causes include a lack of iron in the diet, blood loss and problems absorbing iron from food. Lack of iron can lead to anaemia, where there are fewer red blood cells to carry oxygen around the body.Common symptoms of anaemia include:
- feeling tired and lacking in energy
- feeling short of breath
- fast or irregular heartbeat
Its important to speak to a dietitian before cutting down on fibre so you dont miss out on the health benefits. For example, they may suggest that some people cut down on fibre for a short time during a flare-up, before slowly adding it back in to the diet.Fibre-rich foods include:
- diarrhoea loose and runny stools.
- sipping a cold drink
Green Banana & Applesauce
Both green bananas and cooked and cooled apples are high in soluble fibers and resistant starches which help to slow down transit and soak up excess moisture which can be helpful if diarrhea is a concern. According to theUniversity of Wisconsin Health, applesauce is helpful for ulcerative colitis and are a rich source of vitamins and minerals like potassium.
Read Also: Are Eggs Bad For Ulcerative Colitis
Read Also: Stomach Ulcer And Back Pain
Specific Diets For Ibd
A number of specific diets have been explored for IBD, including the Mediterranean diet, specific carbohydrate diet, Crohns disease exclusion diet, autoimmune protocol diet, and a diet low in fermentable oligo-, di-, monosaccharides, and polyols .
Although the IOIBD group initially set out to evaluate some of these diets, they did not find enough high-quality trials that specifically studied them. Therefore, they limited their recommendations to individual dietary components. Stronger recommendations may be possible once additional trials of these dietary patterns become available. For the time being, we generally encourage our patients to monitor for correlations of specific foods to their symptoms. In some cases, patients may explore some of these specific diets to see if they help.