Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms can vary, depending on the severity of inflammation and where it occurs they typically develop over time. Most people experience mild to moderate symptoms, but the course of ulcerative colitis may vary and some people have long periods of remission. The symptoms depend on the location of the disease-causing inflammation. If you have ulcerative colitis, you may have the following signs and symptoms:
- Diarrhea, often with blood or pus
- Abdominal pain and cramping
- An increased risk of blood clots in veins and arteries
How A Professional Can Help
Living with ulcerative colitis can be frustrating, and its better if you dont have to go at it alone. Working with a gastroenterologist and a registered dietitian can help. Medications can ease symptoms, and diet changes can help to control flares. Its especially important to include a registered dietitian if youre trying an elimination diet since they will work with you to prevent any nutritional deficiencies.
Since everyone with UC has different triggers, figuring out what works best for youand the trial and error that goes along with itwill be much easier with the help of health professionals.
Managing Ulcerative Colitis With Diet
Dietary changes are among the best ways to control ulcerative colitis. The food you eat can affect the tissue inside your digestive system and trigger inflammation. Avoid trigger foods and replace them with foods that are easier to digest to reduce the chances of a flare-up.
Foods that are generally easily tolerated include the following:
- Cooked vegetables if they are skinless and seedless
- Calcium-rich foods such as yogurt, collard greens, and certain dairy products
- Food with probiotics such as kimchi, miso, and sauerkraut
Foods that are more likely to cause a flare-up of symptoms include the following:
- Insoluble fiber
Recommended Reading: Ulcer On Eye From Contact Lens
We Are Leaders In Research
The Foundation has been a leader in inflammatory bowel disease research since our founding more than 50 years ago. We fund cutting-edge research studies and clinical trials at major medical institutions, and finance underdeveloped areas of research. We enthusiastically nurture investigators in the early stages of their career to help build the next generation of IBD researchers.
We are proud that the National Institutes of Health has commended us for uniting the research community and strengthening IBD research.
Diet Plan For Ulcerative Colitis
Ulcerative Colitis is a health condition that causes sores and inflammations in the inner lining of the rectum and colon, causing ulcers. Diet plan for ulcerative colitis, Anyone of us can before the age of 30 be affected by the condition, showing up some of the most common symptoms like abdominal cramps and pains, blood in the stool, and diarrhea. If your condition is severe, you may also face frequent diarrhea, loss of appetite, and fever. Weight loss and consistent weakness.
Ulcerative Colitis is mostly a chronic health condition, with repeated flare-ups and remissions. In most cases, people suffering from ulcerative colitis have mild symptoms, but the conditions can rapidly deteriorate, resulting in serious complications.
But all said and done, ulcerative colitis can be effectively treated with the right diet and medication. It is believed that medication is just a segment of the overall treatment, a diet plan for ulcerative colitis, has a huge role to play. Even some healthcare professionals advocate that diet is the most important factor in the whole treatment process of the condition.
Recommended Reading: What Can I Do For Mouth Ulcers
What Should I Eat
Its not always easy knowing what foods best fuel your body, especially when you have Crohn’s disease or ulcerative colitis. Your diet and nutrition are a major part of life with inflammatory bowel disease , yet there is no single diet that works for everyone.
Nutrition affects not just your IBD symptoms, but also your overall health and well-being. Without proper nutrients, the symptoms of your Crohns disease or ulcerative colitis can cause serious complications, including nutrient deficiencies, weight loss, and malnutrition.
We have several tips for a healthy diet thats well-balanced and nutrient rich. These tips are for educational purposes only. You should work with your doctor or a dietitian specializing in IBD to help you develop a personalized meal plan.
Watch our with Emily Haller, registered dietitian at Michigan Medicine! Tune in to hear Emily review diet facts, debunk myths, speak about restrictions, and highlight ongoing research.
Creatures Of Sonaria Unreleased
May 02, 2022 · High-fiber foods, including whole grains, can increase bowel movements, abdominal cramping, and gas. Meats, especially fatty meats, can trigger ulcerative colitis symptoms. Excess fat may not be properly absorbed during a flare, and this can make symptoms worse. Red meat can be high in sulfate, which triggers gas..
cadance daniel
Diet and Nutrition. Living with inflammatory bowel disease means paying special attention to what you eat. Eating certain foods can help ease your symptoms, while other things you like to eat may make your symptoms worse. Restoring and maintaining good nutrition is a balancing act. Your diet needs to include enough calories and and ….
To control Ulcerative Colitis, you can start making some simple changes in your lifestyles and food habits which are mentioned below, along with the diet plan for Ulcerative Colitis patients mentioned above: Dos: Having 5 small, easily digestible meals a day at proper intervals is a key to good digestive health.
doc hudson license plate
Colitis is a term used to describe inflammation of the colon. There are many causes of colitis, for example, infections , poor blood supply, and autoimmune reactions.Symptoms of colitis include:.
western mass news anchors
Eggs. Grapes. Green beans. Hard cheeses. Lean meats. Peppers. Potatoes. Tomatoes. This diet is not very restrictive, since there is a wide spectrum of foods to choose from, and is fairly easy.
puppy love short story
extraordinary families
Don’t Miss: How To Treat H Pylori Ulcer
Foods Allowed On The Spc Diet
- All fresh and unprocessed fruit, organic is preferred
- Non-starchy unprocessed vegetables like mushrooms, asparagus, and brussel sprouts
- All fresh and frozen meats, organic preferred
- Plant-based milk like almond, coconut, or oat milk
- Hard cheeses aged over 90 days
- Nuts and seeds like pumpkin seeds, almonds, walnuts, pecans, and cashews
- Dried navy beans, lima beans, black beans, green string beans, and lentils
Ulcerative Colitis: Let’s Talk
Colitis, Ulcerative Colitis, and Crohn’s are often used interchangeably – but in reality, they explain three different conditions. Colitis is the general inflammation of large intestine lining . It is synonymous with Irritable Bowel Disease and encompasses multiple conditions. Ulcerative Colitis: is a specific digestive issue, identified by ulcers on your large intestine.
You May Like: What Are The Signs Of Duodenal Ulcers
What Can I Eat During Remission
When your UC is in remission, your instinct might be to reach for foods that are normally off-limits during a flare. But its still best to stick with generally trigger-free fare.
I would advise someone to eat plenty of diverse vegetables and fruits and consider following an anti-inflammatory style diet or Mediterranean diet, says Dr. Singh.
Though, fiber, in its many forms, may be better tolerated during remission, says Freuman. Go for the raw veggies, eat the salad, have a handful of whole nuts, or leave the skin on your fruits and vegetables, she says.
That said, Freuman adds that some people find that these types of foods bother them even in remission, and thats perfectly okay. Its not worth suffering or making yourself sick to push beyond the comfortable limits of tolerance, notes Freuman.
Ultimately, she encourages her clients to eat the greatest variety of plant-based foods they can comfortably tolerate as the foundation of their diets.
Eating When You Are In A Flare
There are certain foods you may want to avoid when you are in an IBD flare, and others that may help you get the right amount of nutrients, vitamins, and minerals without making your symptoms worse.
Your healthcare team may put you on an elimination diet, in which you avoid certain foods in order to identify which trigger symptoms. This process will help you identify common foods to avoid during a flare. Elimination diets should only be done under the supervision of your healthcare team and a dietitian so they can make sure you are still receiving the necessary nutrients.
Some foods may trigger cramping, bloating, and/or diarrhea. Many trigger foods should also be avoided if you have been diagnosed with a stricture, a narrowing of the intestine caused by inflammation or scar tissue, or have had a recent surgery. Certain foods can be easier to digest and can provide you with the necessary nutrients your body needs.
Recommended Reading: How Is Ulcerative Colitis Causes
When Should You See A Doctor About Ulcerative Colitis Food Triggers
According to Dr. Schwimmer, seeing a doctor at the first sign of ulcerative colitis symptoms is your safest bet, especially if youve never been formally diagnosed. Concerning, unexplained symptoms like bloody stool, diarrhea, and abdominal cramping shouldnt be ignored, because even if its not ulcerative colitis, you might be dealing with something else that needs proper treatment.
After youve been diagnosed, your doctor might recommend making diet adjustments as a part of your ulcerative colitis treatment plan. But ultimately, FDA-approved medications, which help control the inflammation that sets off GI pain, are going to be the main course of treatment that your doctor suggests for the long haul of this chronic condition.
There is no secret treatment for inflammatory bowel disease. Everybodys looking for the secret pills. What diet can I follow? What supplement can I take? What probiotic can I take? Unfortunately, it just doesnt exist, Dr. Schwimmer says. But the medicines we have work and they work better than anything else.
Thats why doctors who specialize in IBD caution that self-treatment with diet is not enough. If you arent working within the framework of a plan that includes proven, FDA-approved medication, you are at a higher risk of complications from your ulcerative colitis, including malnutrition.
Track The Good And The Bad
There’s no single diet that will help everyone with UC. The condition can also change over time, so your plan will need to be flexible, too. The key is to find what works for you.
To stay organized, keep a food diary. Use your smartphone or a small notebook to record what you eat and drink and how they make you feel, both good and bad. It takes a bit of time and patience, but it will help you track your condition and fine-tune your diet plan.
When you prepare your meals, don’t forget that a well-balanced diet gives you enough protein, whole grains, and fresh fruits and vegetables.
You might not be able to eat everything in the grocery store or on the menus at the restaurants you like. But try to focus on the ones that you can enjoy without triggering your symptoms. Some simple tweaks in your meal prep can make it easier to eat some foods, like steaming veggies or switching to low-fat dairy.
Some people follow a low-residue diet or low-fiber diet every so often, getting about 10-15 grams of fiber a day. That can help you go to the bathroom less often.
Watch out for items that can be troublemakers if you have UC, including:
Also Check: How To Heal An Ulcer At Home
Can Certain Foods Really Cause Inflammation
The link between what we eat and chronic inflammation in the body isnt fully understood. What is known is that there does seem to be some connection.
Lets jump into the science: The liver produces something called C-reactive protein as a response to inflammation in the body. In short, higher levels of CRP mean more inflammation, and certain foods have been shown to increase levels of CRP in the blood.
Now, the specifics of what foods cause this increase is somewhat up for debate, but its possible that things like processed sugar can trigger the release of inflammatory messengerslike CRPa sign that they may potentially be contributing to an inflammatory state.
On the other hand, foods like fruits and vegetables may help fight oxidative stress, which is a trigger for inflammation. Certain diets, like the Mediterranean diet, already include many foods that are considered to be anti-inflammatory such as whole grains, legumes, a rainbow assortment of fruits and vegetables, and fish.
Foods That May Fight Uc
Some research shows that certain nutrients may help fight the irritation and swelling in your gut caused by UC. Scientists have studied how linoleic acid affects people with the condition. Although everyone needs this “good” fat, donât overdo it, since there is some evidence it may play a role in inflammation if you get too much.
Other studies show that an omega-3 fatty acid called EPA may fight inflammation. This is another âgoodâ fat that blocks certain chemicals in your body called leukotrienes. Fish oil is a good source of EPA. In some studies, folks with UC saw some benefits when they took high doses. Many people, though, didn’t like the fishy taste. There is also some evidence that adding fish oil to aminosalicylates may be helpful, but this isnât proven. DHA is another omega-3 found in fish oil that can fight inflammation and is used by some people with UC.
Some research also shows that yogurt with gut-healthy bacteria, called probiotics, eases inflammation. Scientists are still studying how they may help people with UC and similar conditions. Some people also believe that a diet low in FODMAPs — a type of highly-fermentable carbs found in meats, fruits, dairy, and lots of other foods — may help ease UC symptoms. But the evidence is unclear if it does. And without close monitoring, any diet that restricts certain foods may lead to poor nutrition and other problems.
Show Sources
You May Like: Best Cure For Leg Ulcers
Swap Whole Nuts For Nut Butter Spread
While nuts and seeds are chock-full of fiber and healthy fats, they can be difficult to digest for people with UC. The worst offenders are the hard varieties like peanuts, almonds, and hazelnuts, but all nuts should be avoided if youre sensitive to them, especially during a flare.
Fortunately, substitutes abound for nut lovers in the form of peanut butter and other nut butters, such as almond or cashew. Keeping these in your diet is a plus, because they contain monounsaturated fats, which can soothe inflammation, says Lillian Craggs-Dino, RDN.
Breakfast To Control Diarrhea And Cramping
A low-fiber and low-residue diet eases bouts of diarrhea and abdominal cramping associated with ulcerative colitis. Follow this type of diet for the short term and after physician consultation, because it restricts your nutrition intake. Breakfast may include 1/2 cup of apple juice, one scrambled egg with one slice of toasted white bread and a side of plain grits. Plain hot or cold cereal can replace grits, and you may add one slice of cheese to the eggs if you can tolerate dairy. Choose cranberry juice or strained and pulp-free orange juice as an alternative to apple juice. Top the toast with margarine or low-sugar jelly.
Limit foods high in saturated fats because these increase the amount of waste passing through your colon. Choose well-cooked or tender cuts of meat and nonfat or low-fat dairy as tolerated. Lunch may include a tuna sandwich with an iceberg lettuce slice on white bread, 1/2 cup of cooked carrots on the side and a medium banana. Add a cup of low-fat milk or fruit juice to complete the meal. Instead of bread, wrap the tuna in a white grain pita or tortilla and opt for steamed salmon or flounder as a fish alternative. Use herbs, pepper or plain gravy instead of salt to flavor foods.
Also Check: What Are The Signs And Symptoms Of Ulcerative Colitis
How Can I Track Foods That Cause Flare
The Crohnâs and Colitis Foundation of America recommends people with ulcerative colitis keep a food journal to keep track of what they eat. Note what you eat and drink, and how you feel afterward, noting any symptoms that arise. Start to keep a list of any foods you suspect may trigger or aggravate your ulcerative colitis symptoms. A food diary will also help you figure out if you are getting adequate nutrition, and can help your doctor or dietician determine the right diet for you to manage your symptoms and prevent flares.
The Crohnâs and Colitis Foundation of America also has an interactive food tracking tool. It is available online or as a mobile app. www.ccfa.org/gibuddy
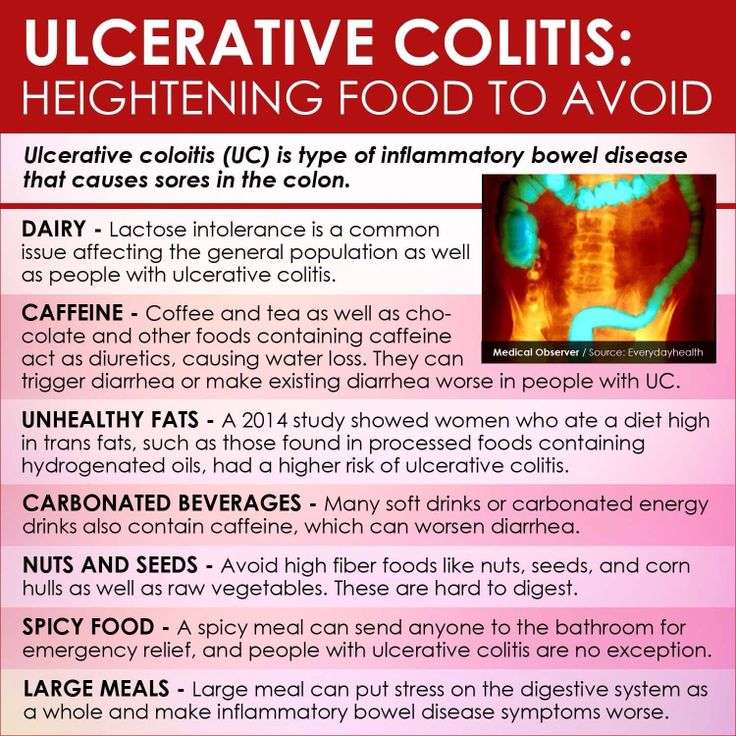
Ulcerative Colitis Diet Restrictions: Food Items To Limit
Check out foods items list to avoid with ulcerative colitis problem. Try to avoid spicy and acidic food and also need to redcue consumption of coffee and other carbonated drinks.
Don’t Miss: Can Ulcerative Colitis Cause Blood In Stool
Food Swaps For A Healthy Ulcerative Colitis Diet
Follow these tips to reduce flares while enjoying the foods you love.
The effect that food can have on a persons ulcerative colitis flares can be unpredictable. Tomatoes or onions, for example, may irritate one persons digestive system, but they may not trigger the same symptoms in someone else.
Still, even though there is no specific ulcerative colitis diet, there are some foods, generally speaking, that can worsen a flare and should be avoided.
When we think of ulcerative colitis, we have to ask, Is this person in a flare meaning, is there inflammation in the GI tract? Eating insoluble fiber like nuts, seeds, peels of fruits, and raw veggies only further irritates an ulcerated, inflamed colon, says Stacy Cavagnaro, a registered dietitian for the Inflammatory Bowel Disease Medical Home at Cleveland Clinic.
If you have UC, you may feel helpless against the flare-ups, wondering if youll ever be able to enjoy normal food again. But dietary and lifestyle modifications may help control your symptoms and extend the time between flares. Here are seven food swaps to help minimize symptoms and keep you in remission.