Treating Stage 3 Bedsores
Wound care is essential to start the healing process for a pressure injury. Those with stage 3 bedsores should go to a doctor right away for treatments.
Treatment of stage 3 bedsores may include:
- Antibiotics to fight infection
- A special bed or mattress to help with recovery
- Debridement the surgical removal of dead tissue
- Taking pressure off of the bedsore
Treating these injuries can be difficult because deep sores often require surgery and heal slowly. That said, its important to seek treatments because the alternatives a risk of stage 4 bedsores or life-threatening infections are much worse.
Do you or your loved one have a stage 3 bedsore? Learn if you qualify for compensation to cover medical bills. Call .
Questions For Your Doctor
- What should I do if I or a loved one has pressure sores and is too heavy to move?
- Does an adjustable bed help reduce the risk of pressure sores?
- Can you die from an infected pressure sore?
- Is diabetic foot ulcer the same as a pressure sore?
- Can you get pressure sores from sitting in the same position in your job for longer than 2 hours at a time?
Also Check: Diabetic Foot Ulcer Treatment Guidelines
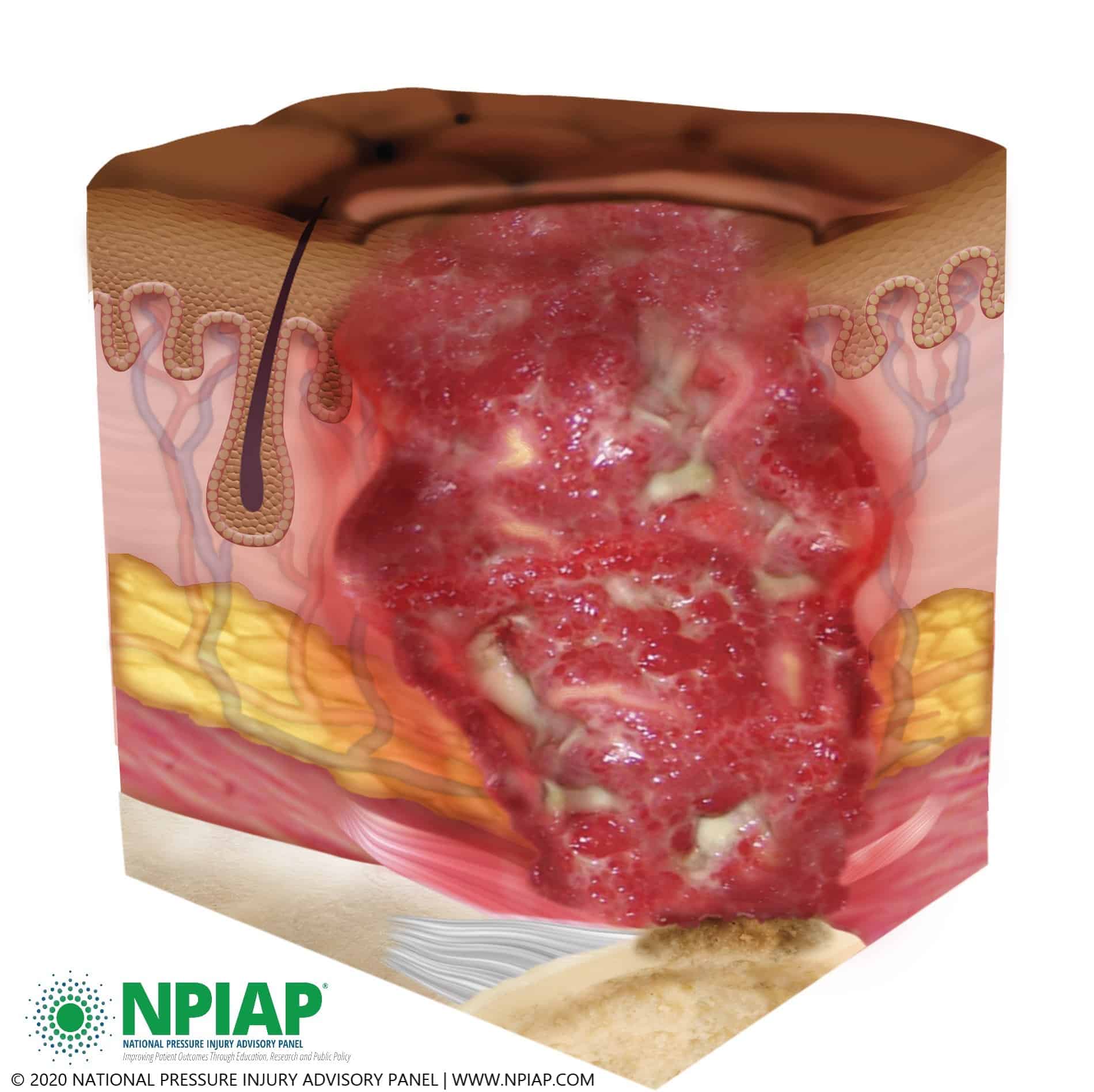
Diagnosing A Stage 3 Bedsore
A medical professional relies on a bedsores appearance to diagnose its stage.
Stage 3 bedsores have the following characteristics:
- Black or rotten outer edges
- Crater-like indentation
- Dead, yellowish tissue
- Visible fat tissues
Stage 3 bedsores are quite deep, but tendons, ligaments, muscles, and/or bones will not be visible. If they are, the patient likely has a stage 4 bedsore. That said, health care providers may not be able to properly stage every severe bedsore.
Two complications may delay a stage 3 bedsore diagnosis:
- Deep tissue injuries: A deep tissue injury occurs when there is no open wound but the tissues beneath a patients skin are damaged.
- Unstageable injuries: If a doctor cannot see the base of the sore due to slough or eschar in the wound bed, they cannot make a diagnosis.
Even if a bedsore cannot be staged, doctors can still recommend treatments to start the healing process.
Also Check: How To Treat Oral Ulcers
Negative Pressure Wound Therapy
This is an invaluable tool in the management of pressure sores and involves the application of sub-atmospheric pressure to a wound using a computerised unit to intermittently or continuously convey negative pressure to promote wound healing. NPWT, is effective for deep, cavitating, infected and copiously discharging pressure ulcers, particularly with exposed bone. With growing clinical experience it can be said with certainty that it assists wound healing, and its benefits can be summarised thus:
- Assists granulation.
- Applies controlled, localised negative pressure to help uniformly draw wounds closed.
- Helps remove interstitial fluid allowing tissue decompression.
- Helps remove infectious materials and quantifies exudates loss.
- Provides a closed, moist wound healing environment
- Promotes flap and graft survival.
- Both hospital and domiciliary use.
- Reduces hospital/dressings/nursing cost .
Protect The Periwound Skin
Askina® Barrier Cream acts as a protectant and moisture barrier against maceration caused by incontinence or body fluids, to protect sensitive, fragile skin and severely dry skin, including periwound areas. It is indicated for use on intact skin.
Askina® Barrier Film Swab andAskina® Barrier Film Spray are sterile liquid dressings which form a transparent film when applied to the skin. The film possesses good oxygen and moisture permeability. Both dressings are indicated for use on intact or damaged skin.
Recommended Reading: How To Know If You Have A Bleeding Ulcer
Key Points About Bed Sores
- Bedsores are ulcers that happen on areas of the skin that are under pressure from lying in bed, sitting in a wheelchair, and/or wearing a cast for a prolonged period.
- Bedsores can happen when a person is bedridden, unconscious, unable to sense pain, or immobile.
- Bedsores can be prevented by inspecting the skin for areas of redness every day with particular attention to bony areas.
Evaluation Of The Healing Progress Of Pressure Ulcers Treated With Cathodal High
2016, Advances in skin & wound care
Abstract
To investigate the effectiveness of high-voltage monophasic pulsed current as an adjunct to a standard wound care for the treatment of Stage II and III pressure ulcers . Prospective, randomized, double-blind, controlled clinical study. Two nursing and care centers. Patients with PrUs that did not respond to previous treatment for at least 4 weeks were randomly assigned to the electrical stimulation group or to the control group . Both the ES and control groups received standard wound care and respectively, cathodal HVMPC applied continuously for 50 minutes once a day, 5 times a week, or sham HVMPC. Percentage area reduction over 6 weeks of intervention. In the ES group, there was a statistically significant decrease in WSA after 1 week of…
Recommended Reading: How To Ease A Stomach Ulcer
Who Is At Risk Of A Pressure Ulcer
People immobile due to illness or injury are at greatest risk of getting a pressure ulcer.
- They may be unable to change position without assistance eg, see Skin complications of paraplegia and tetraplegia.
- They may have nerve damage from injury or illness, such as spina bifida, diabetes or stroke, and are unable to sense pain or the signals that normally make people move.
- Older people are at greater risk because their skin is thinner and more fragile.
- A pressure ulcer may develop underneath a plaster of Paris or fibreglass plaster .
What Causes A Pressure Ulcer
A pressure ulcer is caused by a lack of blood flow due to mechanical stress on the skin and tissues over a bony area that has been under pressure for a prolonged period. If the blood supply is cut off to an area of skin for more than 23 hours, the skin is deprived of oxygen and begins to die. In addition, when slowly sliding down a bed or chair, friction to the outer skin layer such as from wrinkled bedding and clothing contribute to skin injury and ulceration. Excessive exposure to moisture, such as sweat, blood, urine or faeces, also increases the likelihood of developing a pressure ulcer.
Don’t Miss: Ulcer On Bottom Of Foot
What Are The Complications Of Bedsores
Once a bedsore develops, it can take days, months, or even years to heal. It can also become infected, causing fever and chills. An infected bedsore can take a long time to clear up. As the infection spreads through your body, it can also cause mental confusion, a fast heartbeat, and generalized weakness.
Bedsores And Nursing Home Neglect
Stage 3 bedsores in nursing homes are often caused by nursing home neglect. Many older adults and their loved ones rely on nursing homes and their staff to provide care. This is especially true when a resident has health problems that prevent them from moving, such as a spinal cord injury.
Nursing home staff members are trained to check on residents who are at risk of bedsores and help with repositioning. However, not all staff members follow through on their duty to help their residents.
Staff burnout, understaffing, and carelessness can prevent at-risk residents from getting the care they need. In these cases, nursing home staff members are directly responsible if a stage 3 bedsore develops.
Recommended Reading: How Does Ulcer Pain Feel
Prevention: Mattresses And Cushions
Protection is the best way to prevent ulcers. Patients who are at risk of developing pressure ulcers should have the skin carefully inspected for any damage or redness twice daily. The skin should be kept clean and dry. Any pressure causing damage to skin or tissue should be immediately eliminated. This can be done with the help of special mattresses, cushions and by many protective devices that can relieve the external pressure on vulnerable areas of body limbs. These specially designed protective devices can be very helpful in patients who thought to be at risk of developing pressure ulcers, or who have pre-existing Grade 1 or 2 pressure ulcers. Classified by their static or dynamic nature, many advanced low tech and high tech support surfaces and overlays are available for patients bound to lie on bed for long periods of time. Static surfaces do not require electrical power, while dynamic surfaces require electrical power for shifting and redistributing the pressure within the surface. Other integrated electronic beds like air fluidised beds and electronic moving air mattresses require high technology and heavy machinery to let air and ceramic sphere particles support the object on a stream mechanically are often costly, noisy and not easily available. Due to lack of substantial evidences and researches, it is difficult to firmly conclude about relative effects of support surfaces.
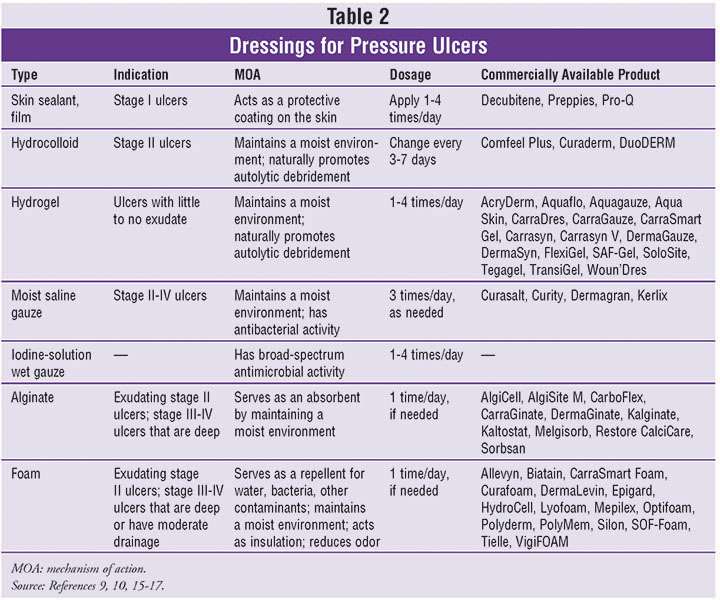
How Are Pressure Injuries Treated
Pressure injuries can be treated in many ways depending on the stage. Once the stage and severity of the wound is determined, it must be cleaned, usually with a saline solution. After the wound is cleaned, it needs to be kept clean, moist, and covered with an appropriate bandage. There are several different types of bandages your doctor may use to dress the wound. These include:
- Water-based gel with a dry dressing
- Hydrocolloid dressing
- Alginate dressing
Sometimes debridement is needed. This is a process of ridding the wound of dead tissue. Debridement is an important part of the healing process. It changes the wound from a long-lasting one to a short-term wound. There are several types of debridement. These methods include:
- Ultrasound: Using sound waves to remove the dead tissue.
- Irrigation: Using fluid to wash away dead tissue.
- Laser: Using focused light beams to remove the dead tissue.
- Biosurgery: Using maggots to eliminate bacteria from the wound.
- Surgery: Using surgery to remove the dead tissue and close the wound.
- Topical: Medical-grade honey or enzyme ointments.
Recommended Reading: Can Ulcers Cause Diarrhea After Eating
Can Bedsores Be Prevented
Bedsores can be prevented by inspecting the skin for areas of redness every day with particular attention to bony areas. Other methods of preventing bedsores and preventing existing sores from getting worse include:
- Turning and repositioning every 2 hours
- Sitting upright and straight in a wheelchair, changing position every 15 minutes
- Providing soft padding in wheelchairs and beds to reduce pressure
- Providing good skin care by keeping the skin clean and dry
- Providing good nutrition because without enough calories, vitamins, minerals, fluids, and protein, bed sores cant heal, no matter how well you care for the sore
Nursing Home Neglect And Stage 3 Bedsores
When a lack of care causes a resident to develop a stage 3 bedsore, nursing home neglect may have occurred.
Neglect is not the same thing as making a simple, harmless mistake its a life-threatening error or series of errors. Sadly, poorly trained or inattentive staff can provide consistently poor care to residents, which can lead to bedsores.
Nursing home neglect often goes hand-in-hand with another issue: understaffing in long-term care facilities. When there are less staff members available, residents may have to wait long hours before their health care needs are addressed.
In chronically understaffed nursing homes, care problems can go unresolved for months making it more likely for bedsores to develop.
Understaffing may lead to stage 3 bedsores, as caretakers are:
- Less likely to notice or treat bedsores in their early stages
- At a greater risk of forgetting to care for every resident
- More likely to leave a resident in bed or a wheelchair for too long
Has your loved one suffered from a stage 3 bedsore?Get a free case review to get justice.
You May Like: Icd 10 Venous Stasis Ulcer
Can You Prevent Stage 3 Bedsores
Yes, stage 3 bedsores can be prevented. Nursing home residents, loved ones, and staff members can all take steps to help prevent bedsores.
| Residents | |
|---|---|
| Work with an ombudsman on behalf of a resident to resolve complaints | Reach out to doctors and nurses if an early-stage sore worsens |
Nursing home ombudsmen are often a good starting point if residents or families are concerned about the risk of bedsores. Ombudsmen serve as advocates for residents and can help resolve care concerns by working with the nursing home facility.
While residents and loved ones play a big role in preventing bedsores, nursing home staff have the most responsibility. They are the residents daily caregivers and must ensure the most vulnerable are not harmed.
If a resident has developed a stage 3 bedsore, then staff members may be guilty of nursing home abuse or neglect. They have worsened the residents health rather than maintaining it.
Legal action is often a valuable tool for residents and family members in these cases. Holding nursing homes legally accountable can prevent other residents from developing bedsores under inadequate care.
Residents Rights Month: Raising Awareness for Nursing Home Abuse JusticeBreaking News for Older Veterans: President Biden Signs The PACT ActPunishments for Elder Abuse
Nursing Home Abuse Justice sheds light on the dangers of nursing home abuse. It provides reporting that exposes truths previously hidden.
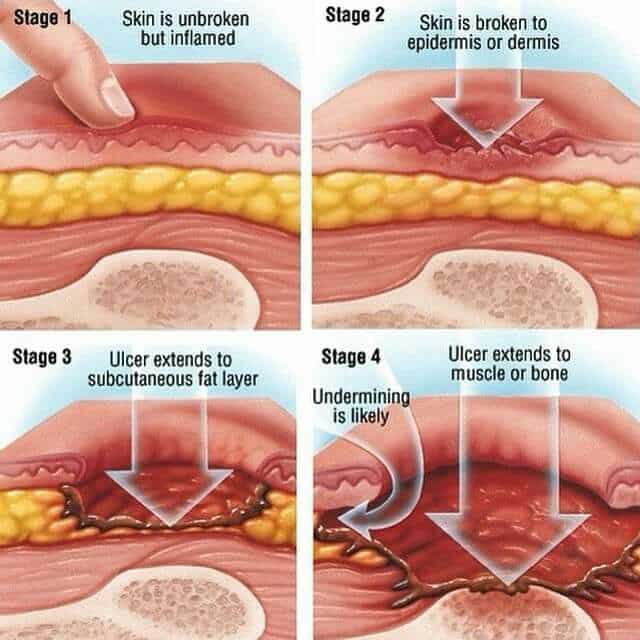
What Are The Stages Of A Pressure Sore
Pressure sores, also known commonly as pressure ulcers, bedsores or decubitus ulcers, are injuries to the body caused by sustained pressure. Pressure sore severity can be categorized according to four main phasesfrom a stage one ulcer where the skin is just beginning to show damage, to a stage four ulcer with open wounds, sores and signs of infection. Whatever the stage, all should be taken seriously and treated with urgency. Here are the four stages of a pressure sore.
Stage 1 Pressure Sores and Ulcers: Early on in pressure ulcer development, the skin is developing injury. While no open sores or broken skin are present yet, skin may appear redder, warmer or firmer than usual. Known as a non-blanchable erythema of intact skin, the color change may indicate the beginnings of a serious injury to the deep tissue.
Stage 2 Pressure Sores and Ulcers: This is where the true sore, or ulcer, develops as a break in the skin and an open sore. It is often very painful, and can create serious damage within the skin. Known as partial-thickness skin loss with exposed dermis, these bed wounds can quickly become something worse and may even present as a blood-filled blister.
Stage 3 Pressure Sores and Ulcers: In stage three, the pressure ulcer has developed into the soft tissue underneath the skin. Known as full-thickness skin loss, this stage may show a deep wound, especially in an area with more adipose tissue.
You May Like: Aip Diet For Ulcerative Colitis
Bone And Joint Infection
Infection can also spread from a pressure ulcer into underlying joints and bones .
Both of these infections can damage the cartilage, tissue and bone. They may also affect the joints and limbs.
Antibiotics are required to treat bone and joint infections. In the most serious of cases, infected bones and joints may need to be surgically removed.
How Pressure Ulcers Develop
Pressure ulcers can develop when a large amount of pressure is applied to an area of skin over a short period of time. They can also occur when less pressure is applied over a longer period of time.
The extra pressure disrupts the flow of blood through the skin. Without a blood supply, the affected skin becomes starved of oxygen and nutrients, and begins to break down, leading to an ulcer forming.
Pressure ulcers tend to affect people with health conditions that make it difficult to move, especially those confined to lying in a bed or sitting for prolonged periods of time.
Conditions that affect the flow of blood through the body, such as type 2 diabetes, can also make a person more vulnerable to pressure ulcers.
Learn more about the causes of pressure ulcers.
Read Also: What Foods Should I Avoid If I Have An Ulcer
Failure Of Reactive Hyperaemia Cycle
It is a known fact that tissue distortion causes ischaemia that in turn stimulates protective movements to relieve pressure and circulatory activity to restore normal blood flow in the affected areas. These protective movements are often reflexes as the person is unaware of making them. However, if these prompt actions prove insufficient to relieve ischaemia, the central nervous system is stimulated by constant signals of discomfort and pain to make sure that the pressure is relieved before any permanent damage occurs. Once the pressure is relieved, and the circulation restored, local capillaries begin to dilate and increased blood flow takes place, referred to as reactive hyperaemia. As a result, a bright pink transitory patch appears on the skin, often called blanching erythema because it blanches on pressure unlike the dull red non-blanching erythema that indicates tissue damage . Reactive hyperaemia ensures a rapid restoration of oxygen and carbon dioxide balance it also flushes out waste products. Erythema subsides as soon as tissues are restored to their resting state.
Various grading of pressure ulcer . A very severe trochanteric pressure ulcer where destruction is so severe that the femoral head dislocated and came out
Measuring Key Processes Of Care
5.2.1 Why measure key processes of care?
While measuring pressure ulcer rates is the ultimate test of how your facility or unit is performing, pressure ulcer rates are limited in that they do not tell you how to improve care. If your pressure ulcer rate is high, on what specific areas should you focus? To know where to focus improvement efforts, it is important to measure key processes of care. Many important processes of care could be measured in assessing pressure ulcer prevention. We recommend initially looking at no more than three:
- Performance of comprehensive skin assessment within 24 hours of admission.
- Performance of standardized risk assessment within 24 hours of admission.
- Performance of care planning that addresses each deficit on standardized risk assessment.
5.2.2 What data sources should be used in measuring key processes of care?
Much pressure ulcer preventive care may not be documented. Nonetheless, we recommend medical record reviews as the source of data on the performance of key processes of care. While rates may initially be low because of poor documentation, this finding will encourage improved documentation of the care actually being provided.
Tools
Use this tool developed by the Quality Improvement Organization program for abstracting medical record data .
5.2.3 How do we ensure performance of comprehensive skin assessment within 24 hours of admission?
Tools
A sample protocol for checking skin assessments is available in Tools and Resources .
Tools
Don’t Miss: How To Calm Down An Ulcerative Colitis Flare Up