Control And Manage Stress
If youre under any stress, you need to control, manage or avoid it. When youre stressed, your body triggers the release of chemicals such as cytokines which can attack your immune system and lead to inflammation.
If you need help managing things around you, make sure you ask for help from relatives or friends. While we cant eliminate stress altogether, we can change our relationship to it by bringing in stress resilience tools to help ourselves cope like meditation, yoga, walking, or calling a friend.
What Are The Causes Of Ulcerative Colitis
The exact cause of ulcerative colitis is unknown. The following possible causes have been suggested:
- Ulcerative colitis is thought to be a type of autoimmune disease, in which the body’s immune system malfunctions and attacks the tissues of the bowel. This results in swelling and redness of body tissue in the infected area. Its also been suggested that no infection is involved and the immune system may just malfunction by itself, or that theres an imbalance of bacteria within the bowel.
Toxic Megacolon: Potentially Fatal Complication Of Ulcerative Colitis
In people with toxic megacolon, a particular portion of the large intestine gets paralyzed and stops working. It can also swell up to many times its normal size. Toxic megacolon is an urgent and potentially life-threatening condition that needs immediate medical attention. If this condition is left untreated, a portion of the large intestine can become severely damaged to the extent that it develops a hole. Perforation of the large intestine could potentially cause severe infection and even death.10,11
Warning signs of toxic megacolon to watch out for include:
- A sudden decrease in the number of daily bowel movements
However, owing to the current therapies for ulcerative colitis, toxic megacolon is not a common condition, but these warning symptoms still require immediate medical attention.
Anytime you experience severe or rapidly worsening abdominal pain along with vomiting, fever, or dehydration, all these should be treated as warning signs that require urgent medical evaluation.12
To prevent toxic megacolon from developing, avoid the following when you have a ulcerative colitis flare-up:
- Taking non-steroidal anti-inflammatory drugs
Don’t Miss: How To Detect A Bleeding Ulcer
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
Can I Treat Ibd If I Am Pregnant Or Breastfeeding
Yes, but your doctor may change the type or amount of the medicine you take. Some medicines, such as methotrexate and thalidomide, cause birth defects and other health problems and should not be taken while you are pregnant or breastfeeding.31
Before you get pregnant, make a plan with your obstetrician and gastroenterologist about the medicines you will take during and after pregnancy. Take your medicines as your doctor tells you to. If you stop taking your medicines and your symptoms come back , it may be difficult to get them back under control.31
Talk with your doctor about your medicines and breastfeeding before you give birth. You can search for your medicine in the LactMed database to find out if your medicine passes through your breastmilk and, if so, if it has any possible side effects for your nursing baby.
Recommended Reading: How Bad Is Ulcerative Colitis
What Does The Colon Do
The large intestine, or colon, is the final part of your digestive system . By the time food has passed through the 6.5 metres of your small intestine and reaches your colon, most of it has been absorbed and only waste products are left. It is the job of your colon to absorb the excess water, as well as some fibre and potassium, from the waste and move the waste to the rectum. This becomes your stools .
Inflammatory bowel disease is a medical term used to describe a group of conditions in which the intestine becomes inflamed . There are two major types of IBD and they require different treatments.
- Crohn’s disease can occur in any part of your intestine.
- Ulcerative colitis only affects your large intestine . Small ulcers can develop on the colon’s lining, and can bleed, produce pus and become inflamed.
Note that IBD should not be confused with irritable bowel syndrome , which is a different condition requiring different treatment.
Favorite Resource For Diet Advice
This book by A. Hillary Steinhart, MD, provides dietary strategies and recipes to help manage inflammatory bowel disease. The head of the combined division of gastroenterology for Mount Sinai Hospital and the University Health Network in Torontos Mount Sinai Hospital, Dr. Steinhart worked with the clinical dietitian Julie Cepo to offer well-researched dietary advice for people to maintain health during flare-ups as well as periods of remission. The book is packed with 150 recipes, from risotto to stew, to help anyone with IBD eat well and prevent malnutrition.
Doctors assured Danielle Walker that her diet was not a factor in her ulcerative colitis flares. But after years of suffering and multiple hospitalizations, Walker realized that she needed to make dietary changes. At the two-year remission mark, the mom, wife, and self-trained chef began blogging about her experience and sharing recipes to help others struggling with IBD. You can buy Walkers cookbooks on her website, which is loaded with nutritional resources including a blog and videos.
Read Also: Early Symptoms Of Ulcerative Colitis
Are Chia Seeds Good For Intestines
Chia seeds can also act as a cleansing agent for your digestive system since they turn into a sticky gel-like substance when soaked in water. This is a great way to get rid of toxins. If you are suffering from digestive problems, chia seed can help you out.
The seeds are rich in omega-3 fatty acids, which have been shown to help with digestive issues such as constipation, bloating, gas, and diarrhea. In addition, they are high in protein, fiber, vitamins A, C, D, E, K, B12 and K2, as well as B-vitamins B1 and B2.
Also Check: How Do You Diagnose An Ulcer
Key Points About Ulcerative Colitis
Also Check: Natural Cures For Gastritis And Ulcers
What Mycrohnsandcolitisteam Members Say About Flaxseed
Some MyCrohnsAndColitisTeam members report experiencing benefits using flaxseed as a supplement. Have you tried adding flaxseeds to your diet? asked one. Works for me. Another finds flaxseed helpful in coping with side effects from disease-modifying antirheumatic medications: Its helped control UC, but it causes constipation now. I grind the flaxseed and add it to a cup of cooled boiled water, then drink two cups of warm water. It really does help.
Other members have found that flaxseed triggers their IBD symptoms. I started flaxseed this week and noticed some cramping, wrote one. I finally stopped taking them, said another. Too much diarrhea and cramping. One member even blamed flaxseed for triggering their latest flare-up: My most recent flare began a month after I added two tablespoons of ground flaxseed daily to my diet. It took me a few days, but I finally realized that it had to be the flax. I stopped taking it immediately.
Others are afraid to try flaxseed due to fears about flares. I found any type of seeds or nuts really irritate my Crohns to the point Im almost ready for the emergency room, said one. But, then again, everyones different.
Ultimately, what works for one person may not work for another. Flaxseed may cause temporary symptoms, but it should not induce a flare. If you are experiencing a flare, its important to limit your flaxseed ingestion.
You May Like: Turning Patients To Prevent Pressure Ulcers
Black Cumin Prevents Lung Inflammation
Black Cumin has been shown to reduce oxidative stress and inflammation. In one study, Nigella sativas antioxidant properties decreased oxidative stress induced by lipopolysaccharide in the rats. This study found the Black Cumin was thus an effective antioxidant and anti-inflammatory agent in lung inflammation. It prevented tissue damage and heightened inflammation that oxidative stress usually causes.
Don’t Miss: Ulcerative Colitis Flare Up Symptoms
How Is Ulcerative Colitis Diagnosed
Colitis shares many symptoms with other common conditions, such as Crohn’s disease, irritable bowel syndrome, gastroenteritis and coeliac disease. Your doctor will examine you and take a detailed history of your symptoms to help rule these out.
There is no single test that can be used to diagnose UC, so a combination of tests is usually required:
- Blood tests help to rule out other medical conditions, and certain markers in the blood can indicate that inflammation is present.
- A stool sample may find other possible causes of diarrhoea and inflammation, such as an infection.
- A colonoscopy may be performed, where a thin, flexible tube that contains a tiny camera looks inside the bowel for ulcers, inflammation and bleeding.
- A biopsy may be taken from inside the bowel so a pathologist can examine it under a microscope to look for signs of disease.
Other types of imaging are sometimes used to help in the diagnosis and to help rule out other diseases.
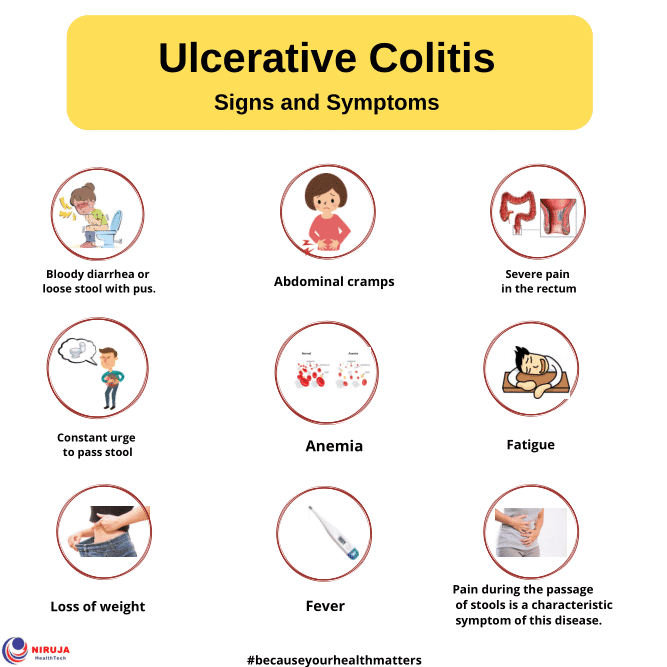
Signs And Symptoms Of Ulcerative Colitis
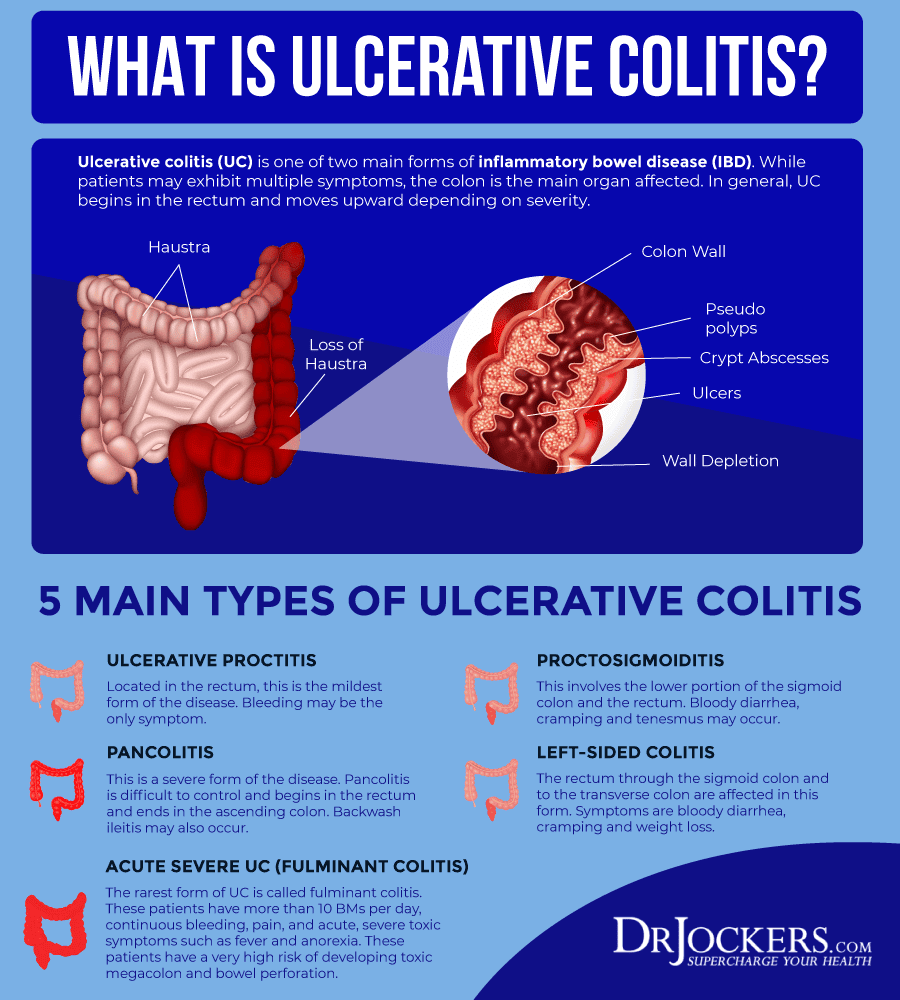
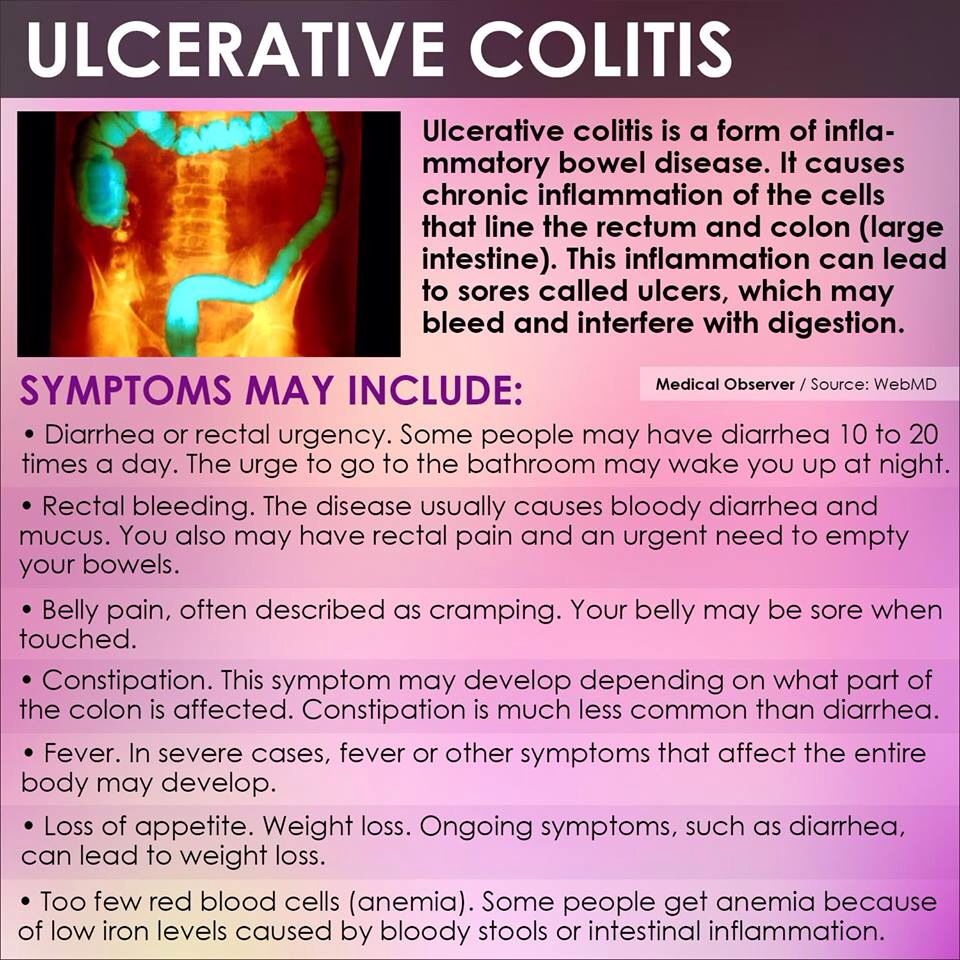
Classified as an inflammatory bowel disease , ulcerative colitis is a disease that primarily affects the digestive tract, but usually also has an impact on other parts of the body. It can cause symptoms of bloody diarrhea, abdominal pain, and an urgent need to empty the bowels. Symptoms can cycle through periods of remission and active disease.
Symptoms may differ from person to person, which can make diagnosis and treatment challenging, but there are a few that hint at having the condition.
Recommended Reading: How To Treat Venous Stasis Ulcers
Whats The Difference Between Ulcerative Colitis Vs Crohns Disease
The list of symptoms for ulcerative colitis and Crohns disease are very similar, including diarrhea, abdominal pain, and rectal bleeding. The biggest difference can be found in the location of the active inflammation. Since Crohns can appear anywhere in the gastrointestinal tract, you might see things like inflammation of the small bowel that you wouldnt see with ulcerative colitis. Another difference is that Crohns doesnt stop at the intestine lining. It can actually affect the entire thickness of the bowel wall.6
Medications For Ulcerative Colitis
Medications can calm the inflammation inside your colon. The first one youâll usually try is from a group called aminosalicylates. If that doesn’t help, your doctor might prescribe a steroid like prednisone. A third option is an immune modifier, which lowers inflammation by changing the activity of your immune system. It can take up to 3 months before you feel the benefits.
Also Check: How To Calm Down An Ulcer
What Other Conditions Are Related To Ulcerative Colitis
Ulcerative colitis is a type of IBD, but it’s not the same as irritable bowel syndrome .
Although the disorders share some of the same symptoms, such as abdominal pain and diarrhea, inflammation and ulcers do not occur with IBS.
Another disease often mentioned alongside ulcerative colitis is Crohns disease. Ulcerative colitis and Crohns are different types of IBDs that affect the digestive tract in different ways.
The two diseases have a lot of common symptoms, but certain symptoms may make your doctor suspect one disease versus the other.
While diarrhea, rectal bleeding, and abdominal pain are common in both diseases, Crohns disease more often causes nausea, weight loss, and vomiting. The types of abdominal pain are often somewhat different.
You Begin Doing The Things You Used To Do
You will know the treatment and medication are working when you start doing the things you enjoyed doing before. For instance, going out or taking on extra activities. As long as you are maintaining your treatment plan and avoiding triggers, there should be no problem with doing the things you enjoyed doing before.
Read Also: What Should You Not Eat With Ulcerative Colitis
Dietary And Lifestyle Modifications
As most nutrients are absorbed higher up in the digestive tract, those with ulcerative colitis generally do not have nutrient deficiencies however, other factors might influence your nutritional state. Disease symptoms may cause food avoidance, leading to food choices that might not provide a balanced diet. If bleeding is excessive, problems such as anemia may occur, and modifications to the diet will be necessary to compensate for this.
Generally, better overall nutrition provides the body with the means to heal itself, but research and clinical experience show that diet changes alone cannot manage this disease. Depending on the extent and location of inflammation, you may have to follow a special diet, including supplementation. It is important to follow Canadas Food Guide, but this is not always easy for individuals with ulcerative colitis. We encourage you to consult a registered dietitian, who can help set up an effective, personalized nutrition plan by addressing disease-specific deficiencies and your sensitive digestive tract. Some foods may irritate the bowel and increase symptoms even though they do not worsen the disease.
In more severe cases, it might be necessary to allow the bowel time to rest and heal. Specialized diets, easy to digest meal substitutes , and fasting with intravenous feeding can achieve incremental degrees of bowel rest.
Search Strategy And Selection Criteria
We searched for relevant manuscripts in PubMed/MEDLINE, Embase, and Cochrane Central from their inception until March 1, 2016. The search combined the MeSH terms ulcerative colitis and inflammatory bowel disease with the subheadings epidemiology, etiology, physiopathology, innate and adaptive immunity, diagnosis, genetics, diagnosis, endoscopy, therapy, surveillance, and complications. Bibliographies of included articles were searched and experts in inflammatory bowel disease were consulted to identify additional studies. Relevant articles and abstracts published in English were critically reviewed. Priority was given to manuscripts published in the past 5 years, randomised placebo-controlled trials, and meta-analyses.
Also Check: Ulcerative Colitis Is It Deadly
Oral Vs Rectal Treatments
Most physicians prescribe ulcerative colitis patients oral versions of 5-ASAs or corticosteroids, since this is a patient-preferred delivery method of medication. However, even if they have a specially designed release mechanism, they might not reach and treat the area where the disease is most active.
For example, when you apply sunscreen to your skin, you need to make sure that you cover every exposed part to protect it from the sun. Similarly, when applying these treatments to your rectum and lower colon, you need to make sure that the product covers all of the inflamed areas.
Oral tablets might not be the optimal way to reach the end of the colon, where stool and the fact that ulcerative colitis patients have diarrhea, might interfere with its effectiveness. Unfortunately, this is also the area in the colon where a flare usually starts. The best way to reach this particular area is by inserting the drug directly into the rectum.
Rectal preparations are particularly good at treating urgency and bleeding, symptoms that often are very bothersome. A positive response often occurs within days of treatment.
Living With Ulcerative Colitis Symptoms
Your ulcerative colitis symptoms will likely come and go, with longer periods in between flares when you may not experience any discomfort at all. Those periods are called remission, and they can span months or even years. Because there is not yet a cure for ulcerative colitis, your symptoms will eventually return.
Ulcerative colitis is an unpredictable disease, and the length of periods of remission between flares can make it difficult for doctors to evaluate whether your course of treatment has been effective or not.
Recommended Reading: Is Pizza Bad For Ulcerative Colitis
Can Ulcerative Colitis Go Into Remission Without Medication
If a person with ulcerative colitis has a deep remission without any sign or symptoms for many years, it might be possible to stop treatment, but theres little information to support this, he says. For most people, continuing to take your medication is the best way to stay in remission and avoid a flare.
Read Also: Can You Get An Ulcer In Your Colon