Complications Of Ulcerative Colitis
UC increases your risk of developing colon cancer. The longer you have the disease, the higher your risk of this cancer.
Because of this increased risk, your doctor will perform a colonoscopy and check for cancer when you receive your diagnosis.
Repeat screenings are recommended thereafter, according to the American Cancer Society. Regular screenings help lower your risk of colon cancer. Follow-up screenings can detect precancerous cells early.
Other complications of UC include:
- thickening of the intestinal wall
- intestinal bleeding
What Are The Symptoms During A Flare
- Diarrhoea. This varies from mild to severe. The diarrhoea may be mixed with mucus or pus. An urgency to get to the toilet is common. A feeling of wanting to go to the toilet but with nothing to pass is also common . Water is not absorbed so well in the inflamed colon, which makes the diarrhoea watery.
- Blood mixed with diarrhoea is common .
- Crampy pains in the tummy .
- Pain when passing stools.
Feeling generally unwell is typical if the flare-up affects a large amount of the colon and the rectum , or lasts for a long time. High temperature , tiredness, feeling sick , weight loss and anaemia may develop.
How Ulcerative Colitis Is Treated
Treatment for ulcerative colitis aims to relieve symptoms during a flare-up and prevent symptoms from returning .
In most people, this is achieved by taking medicine, such as:
- aminosalicylates
- corticosteroids
- immunosuppressants
Mild to moderate flare-ups can usually be treated at home. But more severe flare-ups need to be treated in hospital.
If medicines are not effective at controlling your symptoms or your quality of life is significantly affected by your condition, surgery to remove your colon may be an option.
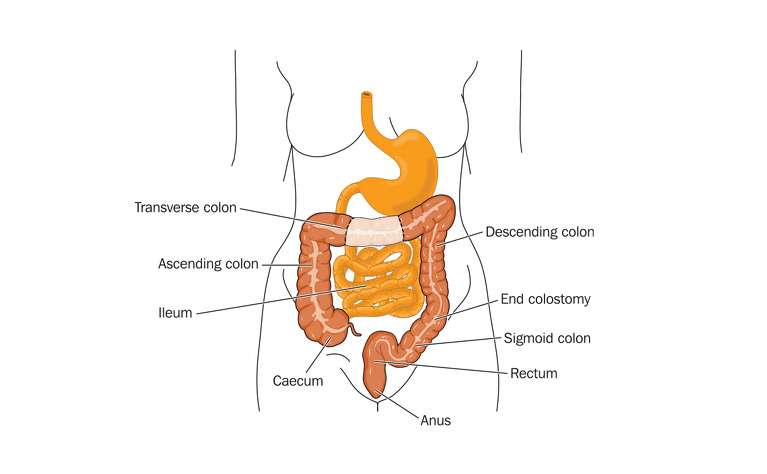
During surgery, your small intestine will either be diverted out of an opening in your abdomen or be used to create an internal pouch that’s connected to your anus called an ileoanal pouch.
Also Check: Ulcers On Legs From Diabetes
Treatments For Ulcerative Colitis
Ulcerative colitis is a chronic condition, which means you will have to manage it for the rest of your life. There is no cure for ulcerative colitis.
However, there are a variety of treatment options that can help you manage your symptoms and have long-term remission. Your treatment will depend on the severity of your condition, your symptoms, your overall health, and your goals. UCHealth specialists will work closely with you to formulate the right treatment plan.
UC medications
Medications are usually the first treatment for ulcerative colitis. There are many different types to help you manage different symptoms.
Anti-inflammatory medications
- 5-aminosalicylates: These medications work by blocking the chemicals that trigger inflammation. They can be taken by mouth or as a suppository.
- Corticosteroids: Corticosteroids are powerful medications that reduce inflammation and immune system activity. They are usually used in moderate or severe cases of UC that dont respond to other treatments. Long-term use of corticosteroids can have negative side effects.
Immunosuppressants
Ulcerative colitis is an autoimmune condition. So, if anti-inflammatory medications arent working, your doctor may prescribe medications to suppress your immune system to stop UC from attacking your large intestine. Certain commonly prescribed immunosuppressants for UC can affect your liver and pancreas, however, so you will need to have regular follow-ups with your doctor.
Biologics
Other UC medications
Types Of Ulcerative Colitis
The type of ulcerative colitis you have depends on where it is in your body:
- Ulcerative proctitis is usually the mildest form. Itâs only in the rectum, the part of your colon closest to your anus. Rectal bleeding may be the only sign of the disease.
- Proctosigmoiditis happens in your rectum and the lower end of your colon . Youâll have bloody diarrhea, belly cramps, and pain. Youâll have the urge to poop, but you wonât be able to.
- Left-sided colitis causes cramps on that side of your belly. Youâll also have bloody diarrhea, and you might lose weight without trying. Youâll have inflammation from your rectum up through the left side of your colon.
- Pancolitis often affects your entire colon. It can cause severe bouts of bloody diarrhea, belly cramps, pain, fatigue, and major weight loss.
- Acute severe ulcerative colitis is rare. It affects your entire colon and causes severe pain, heavy diarrhea, bleeding, and fever.
Also Check: Best Way To Treat Mouth Ulcers
Could My Symptoms Be Ibs
Irritable Bowel Syndrome is a different condition from IBD, although some of the symptoms are similar. Like Crohn’s and Colitis, IBS can cause abdominal pain, bloating and bouts of diarrhoea or constipation. However, it does not cause the type of inflammation typical of Colitis, and there is no blood loss with IBS.
Some people with Colitis may develop IBS-like symptoms, for example experiencing diarrhoea even when their Colitis is inactive. These symptoms may need slightly different treatment from their usual IBD symptoms. IBS is more common in people with IBD than in the general population.
If you develop diarrhoea with bleeding and abdominal pain, your doctor may suspect you have Colitis, particularly if you are a young adult or have a family history of Crohn’s or Colitis. You will need tests and physical examinations to confirm a diagnosis. See Tests and Investigations for IBD.
You may need to have tests repeated from time to time to check on your condition and how your treatment is working.
Some drug treatments may also require a series of blood tests and, occasionally, x-rays or scans to check for any potential side effects. Your specialist will avoid giving you any unnecessary tests or investigations.
You may need more regular colonoscopies when you have had Ulcerative Colitis for a long time to check for any signs of cancer.
Extraintestinal Manifestations And Complications
Aphthous ulcersPyoderma gangrenosum
UC is characterized by immune dysregulation and systemic inflammation, which may result in symptoms and complications outside the colon. Commonly affected organs include: eyes, joints, skin, and liver. The frequency of such extraintestinal manifestations has been reported as between 6 and 47%.
UC may affect the mouth. About 8% of individuals with UC develop oral manifestations. The two most common oral manifestations are aphthous stomatitis and angular cheilitis. Aphthous stomatitis is characterized by ulcers in the mouth, which are benign, noncontagious and often recurrent. Angular chelitis is characterized by redness at the corners of the mouth, which may include painful sores or breaks in the skin. Very rarely, benign pustules may occur in the mouth .
UC may affect the eyes. Inflammation may occur in the interior portion of the eye, leading to uveitis and iritis. Uveitis can cause blurred vision and eye pain, especially when exposed to light . Untreated, uveitis can lead to permanent vision loss. Inflammation may also involve the white part of the eye or the overlying connective tissue , causing conditions called scleritis and episcleritis. Uveitis and iritis are more commonly associated with ulcerative colitis, whereas episcleritis is more commonly associated with Crohn’s disease.
You May Like: How Long Does Ulcerative Colitis Flare Up Last
How Long Will Ulcerative Colitis Symptoms Last
A flare is a period of time in which symptoms of ulcerative colitis are severe. Generally speaking, flares can last for days or even weeks, although ulcerative colitis is experienced differently from person to person, and duration of symptoms varies greatly for each individual.
People living with ulcerative colitis typically experience periods of both active disease, or flare-ups, and remission, when there are few or no symptoms.
The goal of treatment is to achieve remission.
Ulcerative Colitis: Diet And Management
After you have been diagnosed with ulcerative colitis, you might be asking what you should and shouldnt eat to best take care of your body. Eating well is especially important with ulcerative colitis, since symptoms can lead to weight loss and malnutrition. Unfortunately, there are no hard-and-fast rules when it comes to UC and diet.
Your healthcare team may recommend that you go on an elimination diet. This is a temporary diet that involves avoiding, and then slowly reintroducing, certain foods to see what foods trigger your symptoms. Only follow this diet under our doctors supervision to make sure you are getting adequate nutrition.
Other tips you can try include:
Recommended Reading: Hindgut Ulcers In Horses Treatment
Continuous Signs And Symptoms
Ulcerative colitis can cause signs and symptoms such as diarrhea, blood in the stool, nausea, fatigue, and abdominal pain. One of the goals of treatment is to stay on top of the inflammation that may contribute to these symptoms.
The symptoms of ulcerative colitis can lower a persons quality of life significantly, as well as affect personal relationships and the ability to have a rewarding and successful career. While it does take time and effort to develop a treatment plan, the result can be the cessation of the symptoms and an improvement in quality of life.
What Is A Flare
When you have ulcerative colitis, your physician will try to find the right medications to control your symptoms. However, since there is no cure, the systemic disease is always there. When the symptoms arent present, you are in remission. If the symptoms return, especially if they are worse than before, it is a flare. This is why it is important to continue taking any medications your doctor prescribes, even if you feel better. If you stop taking your medication, then you can increase your chance of experiencing a flare and progression of the disease. Infections, stress, and taking antibiotics or NSAIDs can also make you more susceptible to a flare.
Also Check: Medications For Ulcers Over The Counter
Whats The Difference Between Ulcerative Colitis And Colitis
Colitis refers to inflammation of the inner lining of the colon. Colitis causes symptoms such as abdominal pain and cramping, bloating, and diarrhea.
An inflamed colon can be caused by several conditions. UC is one possible cause. Other possible causes of colitis include:
- infection
- Crohns disease
- an allergic reaction
To diagnose the cause of colitis, a doctor will order a series of tests. These tests will help them understand what other symptoms youre experience and rule out conditions based on what youre not experiencing.
Treatment for colitis will depend on the underlying cause and other symptoms you have.
Ulcerative Colitis Risk Factors
Most people with UC dont have a family history of the condition. However, about 12 percent of people with UC do have a family member with IBD, according to research from 2014.
UC can develop in a person of any race, but its more common in white people. If youre of Ashkenazi Jewish descent, you have a greater chance of developing the condition than most other groups.
Young people with IBD may also be dealing with acne at the same time. Some older studies have suggested a possible link between the use of the cystic acne medication isotretinoin and UC. However, newer research has yet to find a definitive causal relationship.
Theres no solid evidence indicating that your diet affects whether you develop UC. You may find that certain foods and drinks aggravate your symptoms when you have a flare-up, though.
Practices that may help include:
- drinking small amounts of water throughout the day
- eating smaller meals throughout the day
- limiting your intake of high fiber foods
- avoiding fatty foods
- lowering your intake of milk if youre lactose intolerant
Also, ask a doctor if you should take a multivitamin.
Read Also: What Causes Acute Ulcerative Colitis
Pathophysiology Of Ulcerative Colitis
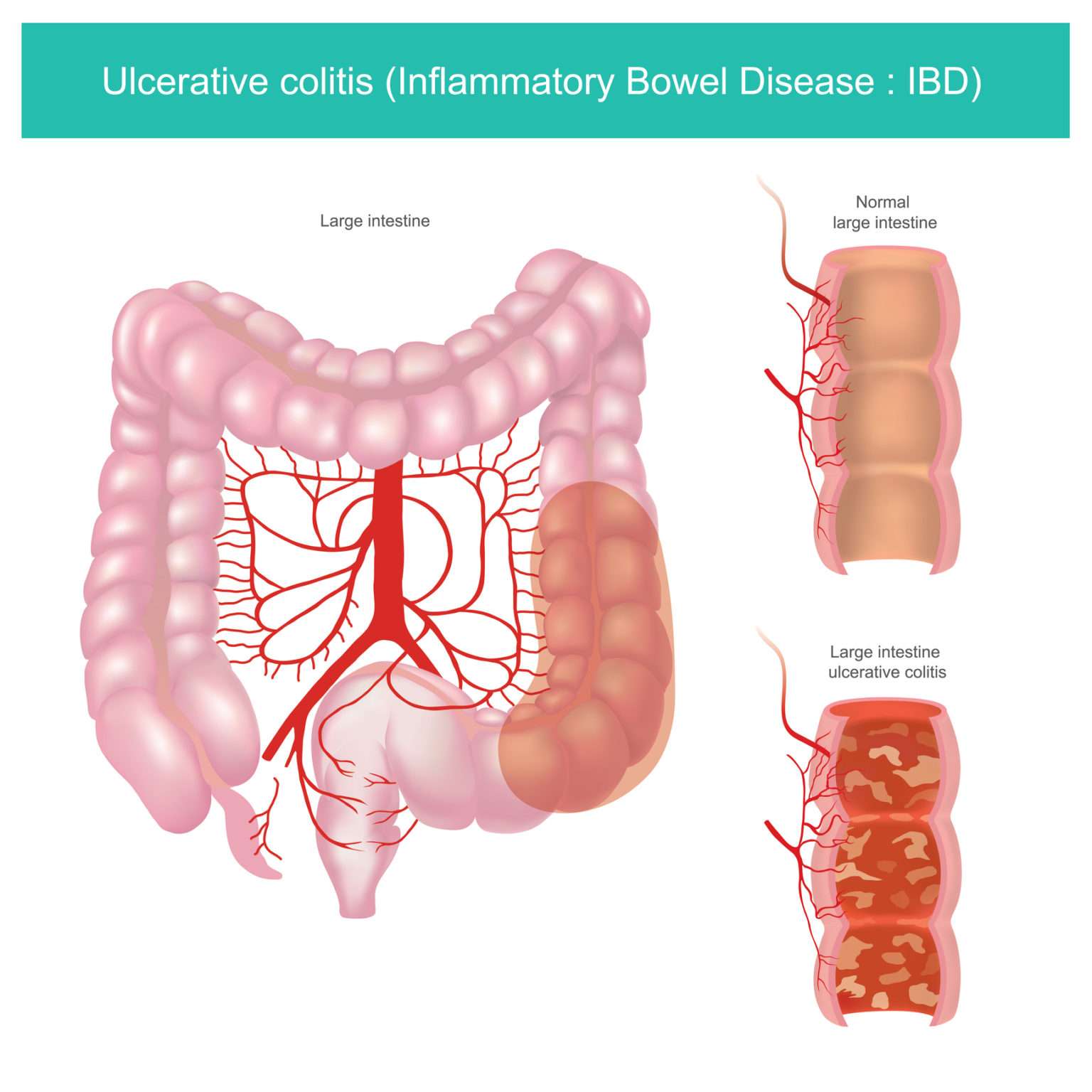
Ulcerative colitis usually begins in the rectum. It may remain localized to the rectum or extend proximally, sometimes involving the entire colon. Rarely, it involves most of the large bowel at once.
The inflammation caused by ulcerative colitis affects the mucosa and submucosa, and there is a sharp border between normal and affected tissue. Only in severe disease is the muscularis involved. Early in the disease, the mucous membrane is erythematous, finely granular, and friable, with loss of the normal vascular pattern and often with scattered hemorrhagic areas. Large mucosal ulcers with copious purulent exudate characterize severe disease. Islands of relatively normal or hyperplastic inflammatory mucosa project above areas of ulcerated mucosa. Fistulas and abscesses do not occur.
Ulcerative Colitis Diet: Foods To Eat And Foods To Avoid
Here in Canada, we have one of the highest rates of ulcerative colitis in the world it is thought that our environment + lifestyle weigh heavily on our risk for the disease.
Most people with ulcerative colitis report that food impacts their symptoms, so its important that nutrition is not overlooked in the management of the disease. Recent evidence suggests that intake of certain foods is associated with a higher risk of ulcerative colitis, including:
- Meat, particularly red meat
- Sugar, and sugar sweetened beverages
- Omega 6 fatty acids
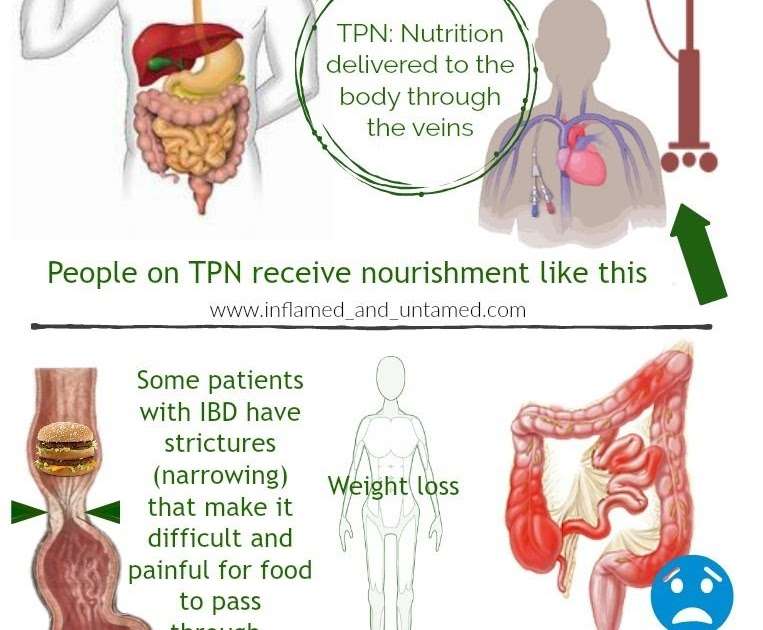
We also know that the inflammation and increased bowel movements in ulcerative colitis and Crohns disease can lead to malabsorption, low food intake and nutrient deficiencies along with osteoporosis. So everyone with ulcerative colitis should be receiving adequate nutrition therapy.
Don’t Miss: Can Ulcerative Colitis Cause Blood In Urine
Ulcerative Colitis And Colorectal Cancer
Ulcerative colitis increases the risk of colorectal cancer. Colorectal cancer often begins as small growths on the inside of the large intestine. The risk of colorectal cancer increases based on:
- the length of time a person has had ulcerative colitis
- how much of the colon is affected by ulcerative colitis
People with ulcerative colitis should have more frequent tests for polyps and colorectal cancer than people at average risk. The gold standard screening test is a colonoscopy. Polyps can be removed during a colonoscopy. This reduces the risk of colorectal cancer. Ask your doctor how often you should be checked for colorectal cancer.
Surgery to remove the entire colon eliminates the risk of colon cancer.
Stress And Ulcerative Colitis
Experts havenât found an exact link. But they have some theories about the connection between the two.
Inflammation. Your body goes into fight-or-flight mode when stressed. That triggers the release of lots of chemicals, including cytokines. Those are molecules that turn on your immune system and lead to inflammation. People with UC might be more sensitive to this process.
Brain-gut axis. Stress changes the signals that travel between your brain and gut. This can cause all kinds of digestion problems, even in people who donât have UC. These changes are also linked to irritable bowel syndrome , food allergies, and heartburn.
Other reasons. Research shows stress might:
- Damage the lining of your gut
- Disturb gut bacteria
- Change how fast or slow your digestive muscles work
- Make your gut more sensitive to pain
Recommended Reading: Can Ulcer Cause High Blood Pressure
Ways To Lessen Stress
You canât get rid of stress entirely. But you can learn to manage it. And studies show you can boost your quality of life when you take care of your mental health.
Ask your doctor for extra help if youâre not sure where to start. They can set you up with a counselor or health psychologist who works with people who have IBD.
They might suggest:
- Tai chi
- Guided imagery
You can also just take a little time each day to do something you find relaxing. That could be gardening, reading, or listening to music. Whatever you enjoy.
Drug therapy is another option. Studies show antidepressants might ease pain in people with IBD. Common choices include selective serotonin reuptake inhibitors and tricyclic antidepressants . Ask your doctor if theyâre right for you.
Favorite Ulcerative Colitis Blogger
Sam Cleasby created her blog in 2013 to raise awareness of IBD and her struggles with self-esteem. Cleasby also has a radio show on BBC Radio Sheffield where she shares about modern family life, including relationships, disability, nutrition, and kids. You can subscribe to her blog via email or follow her on or .
This book by A. Hillary Steinhart, MD, provides dietary strategies and recipes to help manage inflammatory bowel disease. The head of the combined division of gastroenterology for Mount Sinai Hospital and the University Health Network in Torontos Mount Sinai Hospital, Dr. Steinhart worked with the clinical dietitian Julie Cepo to offer well-researched dietary advice for people to maintain health during flare-ups as well as periods of remission. The book is packed with 150 recipes, from risotto to stew, to help anyone with IBD eat well and prevent malnutrition.
Doctors assured Danielle Walker that her diet was not a factor in her ulcerative colitis flares. But after years of suffering and multiple hospitalizations, Walker realized she needed to make dietary changes. At the two-year remission mark, the mom, wife, and self-trained chef began blogging about her experience and sharing recipes to help others struggling with IBD. You can buy Walkers cookbooks on her website, which is loaded with nutritional resources including a blog and videos.
Also Check: What To Eat When You Have Ulcers And Acid Reflux
When You’re In The Hospital
You were in the hospital because you have ulcerative colitis. This is a swelling of the inner lining of your colon and rectum . It damages the lining, causing it to bleed or ooze mucus or pus.
You probably received fluids through an intravenous tube in your vein. You may have received a blood transfusion, nutrition through a feeding tube or IV, and medicines to help stop diarrhea. You may have been given medicines to reduce swelling, prevent or fight infection, or help your immune system.
You may have undergone a colonoscopy. You also may have had surgery. If so, you may have had either an ileostomy or colon resection .
People Describe How They Were Diagnosed With Ulcerative Colitis
Ulcerative colitis, or UC for short, is a form of inflammatory bowel disease that affects portions or all of your large intestine and rectum. The Centers for Disease Control and Prevention estimates that 3.1 million Americans have IBD, which also includes Crohn’s disease .
UC is a chronic condition that can cause long-term inflammation and ulceration, severe diarrhea, abdominal pain, blood and mucous in your stool, urgency, nausea, joint paint, fever, weight loss, and fatigue. UC is also a risk factor in colorectal cancer, according to the Mayo Clinic. And while there’s no known cure for ulcerative colitis, removal of the colon and rectum in a procedure called a proctocolectomy can eliminate the disease.
Other treatment options include corticosteroids, anti-inflammatory drugs called 5-aminosalicylates, immunosuppressant biologics , and bowel resection or removal. Patients can also manage symptoms with pain medication, anti-nausea medication, and antidiarrheals, though all medications should be taken under the care of a doctor. IBD is often confused with irritable bowel syndrome , a disorder that causes pain and cramping of the large intestine. But unlike IBD, IBS doesn’t cause long-term damage to your intestinal tissue or increase your risk of colorectal cancer.
Managing UC is a complex puzzle of treatment options and unpredictable symptoms. We spoke with nine women to find out what life is like with the disease.
Responses have been edited for length and clarity.
Related:
Don’t Miss: How To Treat Sacral Pressure Ulcer