What Should I Tell My Doctor Before Starting Humira
Tell your doctor about all of your health conditions, including if you:
- Have an infection, are being treated for infection, or have symptoms of an infection
- Get a lot of infections or infections that keep coming back
- Have TB or have been in close contact with someone with TB, or were born in, lived in, or traveled where there is more risk for getting TB
- Live or have lived in an area where there is an increased risk for getting certain kinds of fungal infections, such as histoplasmosis, coccidioidomycosis, or blastomycosis. These infections may happen or become more severe if you use HUMIRA. Ask your doctor if you are unsure if you have lived in these areas
- Have or have had hepatitis B
- Are scheduled for major surgery
- Have or have had cancer
- Have numbness or tingling or a nervous system disease such as multiple sclerosis or Guillain-Barré syndrome
- Have or had heart failure
- Have recently received or are scheduled to receive a vaccine. HUMIRA patients may receive vaccines, except for live vaccines. Children should be brought up to date on all vaccines before starting HUMIRA
- Are allergic to rubber, latex, or any HUMIRA ingredients
- Are pregnant, planning to become pregnant, breastfeeding, or planning to breastfeed
- Have a baby and you were using HUMIRA during your pregnancy. Tell your babys doctor before your baby receives any vaccines
Development Of Integrin Inhibitors
Although TNF inhibitors are widely used in the treatment of UC, there are patients who either do not attain a response to an anti-TNF agent, who lose their response, or who develop adverse events associated with anti-TNF therapy. The need for alternative biologic agents for this population led to the development of the integrin inhibitors, which block the migration of leukocytes into the mucosal tissue.30
The main risk associated with vedolizumab is nasopharyngitis.32 Infusion reactions are infrequent, abnormal liver chemistries are rare, and no cases of PML have been observed in any trials.
Abdominal And Rectal Pain
People with ulcerative colitis often experience rectal or abdominal pain. Having a large amount of abdominal pain may be a sign that youre having a flare-up or that your condition is getting worse. Pain can range from mild to severe and may also affect your rectum.
Pain may be accompanied by persistent muscle spasms and cramping.
Don’t Miss: How Do You Treat A Duodenal Ulcer
You And Your Care Team Are In Control
While there is no cure for UCwhile also knowing it can progress and symptoms can get worse over timeits important to remember that you and your doctor can get your disease under control. Recognizing the signs early and getting treatment right away is key. Thats why having open conversations with your doctor and being prepared for every appointment is crucial to managing your UC.
Speak openly with your doctor about how much your UC is truly impacting you. Make a personal action plan to see how much of your time your disease is affecting and get customized steps to help you and your doctor get control of your disease.
Also Check: Can Ulcers Cause Chest Pain And Shortness Of Breath
Talk With Others Who Understand
MyCrohnsAndColitisTeam is the social network for people with inflammatory bowel disease and their loved ones. On MyCrohnsAndColitisTeam, more than 148,000 members come together to ask questions, give advice, and share their stories with others who understand life with Crohns disease and ulcerative colitis.
Are you living with Crohns disease or ulcerative colitis? How was your diagnostic process? Share your experience in the comments below, or start a conversation by posting on your Activities page.
Recommended Reading: Foods To Eat With Ulcerative Colitis Flare Up
You May Like: Can Ulcerative Colitis Go Away On Its Own
New Guideline Provides Recommendations For The Treatment Of Mild
Bethesda, MD Most patients with ulcerative colitis have mild-to-moderate disease characterized by periods of activity or remission, but practice variations exist in disease management. A new clinical guideline from the American Gastroenterological Association published in Gastroenterology, the official journal of AGA, addresses the medical management of these patients, focusing on use of both oral and topical 5-aminosalicylates medications, rectal corticosteroids and oral budesonide, to promote high-quality care for UC patients.
AGAs new clinical guideline is meant to help with the management of patients with mild-to-moderate UC, but not all patients will effectively respond to the outlined therapies. In those cases, there may be a need to escalate treatment to systemic corticosteroids, immunomodulators and/or biologic therapies for induction and maintenance of remission. However, the use of biologic therapies and/or immunomodulators are not specifically addressed within the guideline.
The guideline recommends the following for the medical management of mild-to-moderate ulcerative colitis: 1. Use either standard dose mesalamine or diazo-bonded 5-ASA rather than low dose mesalamine, sulfasalazine or no treatment in patients with extensive mild-moderate UC.
2. In patients with extensive or left-sided mild-moderate UC, add rectal mesalamine to oral 5-ASA.
11. In patients with mildmoderate UC , AGA makes no recommendation for use of probiotics.
Management Of Moderate To Severe Ulcerative Colitis
- Gastroenterology
Youve saved your first item
You can find your saved items on your dashboard, in the saved tab.
Youve recommended your first item
Your recommendations help us improve our content suggestions for you and other PracticeUpdate members.
Youve subscribed to your first topic alert
What does that mean?
Dont Miss: Managing Ulcerative Colitis Flare Ups
Recommended Reading: What Is The Difference Between Ulcerative Colitis And Diverticulitis
Assessing Severity Of Disease In Patients With Ulcerative Colitis
Ulcerative colitis is a chronic disease that can present at various stages of disease activity and severity. Traditionally, severity scoring has focused on disease activity during a single moment with various tools, including patient-reported symptoms, as well as clinical, laboratory-based, endoscopic, histologic, and imaging variables. Optimal delivery of care depends on the accurate assessment of disease severity, which must take longitudinal variables into account. This article reviews the history of severity scoring in UC and provides a concise, clinically oriented approach to assessing disease severity.
Keywords: Clostridium difficile
Recommended Reading: What Does An Ulcerative Colitis Flare Up Feel Like
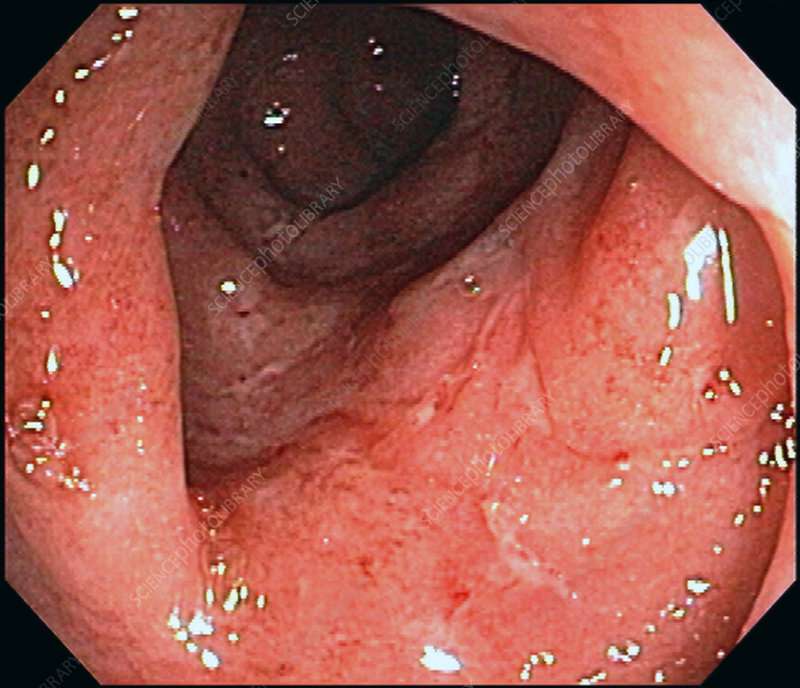
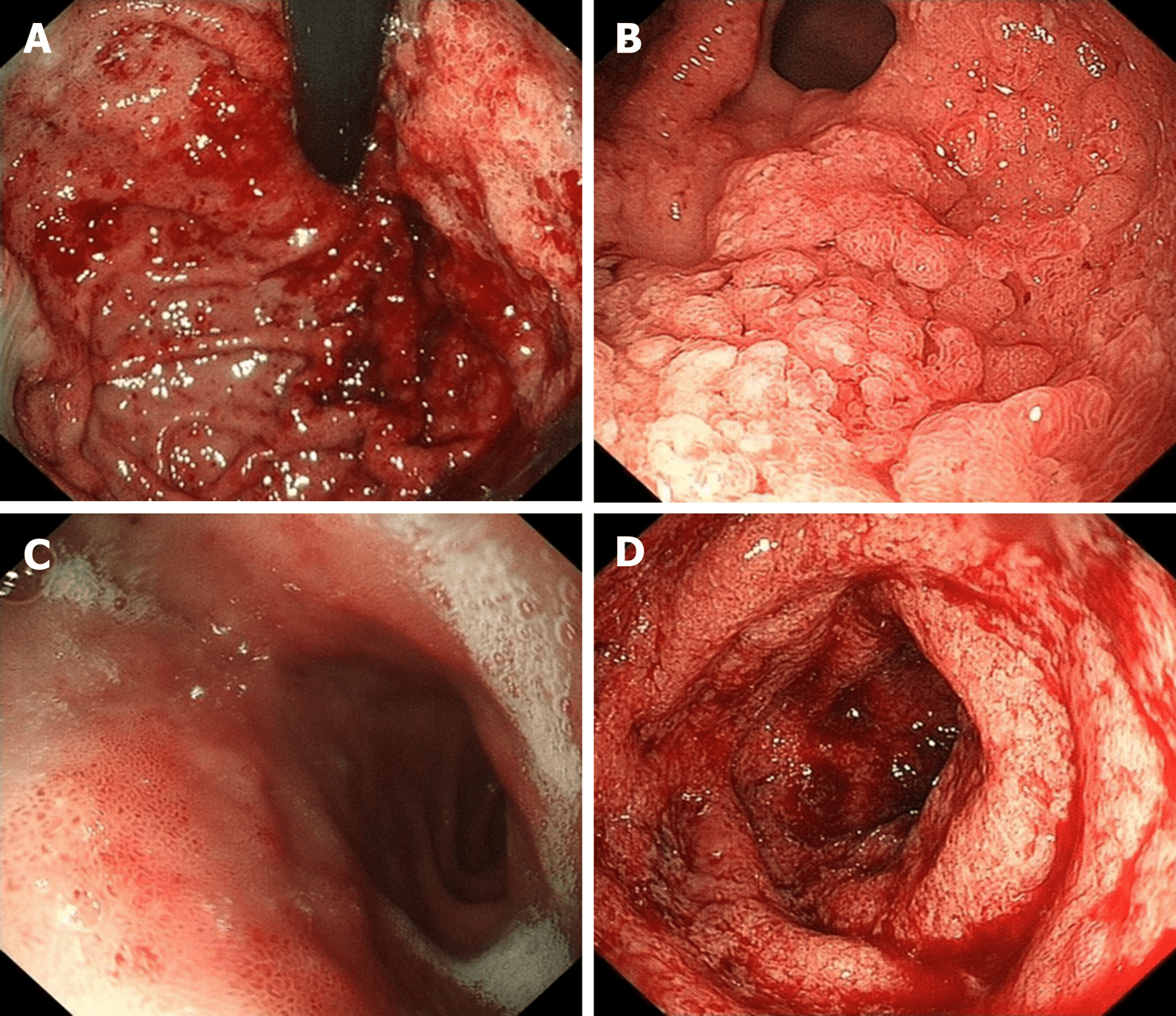
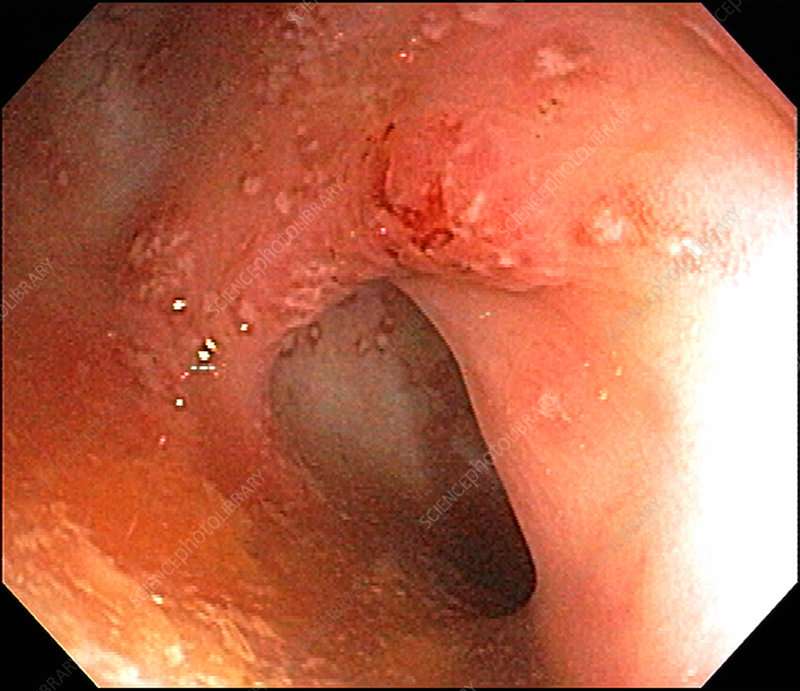
How Does Endoscopy Help Determine Severity
Endoscopy is an extremely important part of determining how severe your IBD is. Using endoscopy, doctors can visually assess the damage to your bowels by identifying and measuring lesions, looking for bleeding, and taking biopsies.
Endoscopy will reveal different findings based on whether you have Crohns disease or ulcerative colitis. Two commonly used indexes to measure endoscopy results are the Simple Endoscopic Score for Crohns Disease and the Ulcerative Colitis Endoscopic Index of Severity.
Some of the important measures for Crohns disease include:
- Whether there are ulcers
- How much bowel surface is involved
- How much bowel surface has ulcers
- Whether there are strictures, or narrowings, of the intestines
- How narrow any strictures are
Some of the important measures for ulcerative colitis include:
- Whether normal intestinal blood vessels are visible or obliterated
- Whether there is blood or visible bleeding
- Whether there are erosions or ulcers
Recommended Reading: What Are The Symptoms Of A Stomach Ulcer In Adults
Point: Maintenance Of Remission With 5
Colectomy rates in UC range from 9% to 25% within 10 years following diagnosis, with the vast majority performed to address unremitting disease activity. Though the use of 5-ASA agents has not been shown to reduce colectomy rates, these agents have been shown to lead to variable degrees of mucosal healing. Achieving mucosal healing has been associated with lower rates of colectomy in both retrospective and prospective studies,, though it should be noted that evaluating and treating for mucosal healing are not without risk and cost. Taking these data into account, it is reasonable to treat patients to potentially modify their disease course and prevent colectomy, especially when we consider the favorable safety profile of 5-ASA agents.
When To Contact A Medical Professional
Contact your provider if:
- You develop ongoing abdominal pain, new or increased bleeding, fever that does not go away, or other symptoms of ulcerative colitis
- You have ulcerative colitis and your symptoms worsen or do not improve with treatment
- You develop new symptoms
There is no known prevention for this condition.
Recommended Reading: Stomach Ulcer Treatment Over The Counter
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
What Are The Medication Options For Ulcerative Colitis
There are a few types of drugs used to treat ulcerative colitis.
Aminosalicylates are typically the first kind of drug prescribed for ulcerative colitis. They work by reducing inflammation directly in your digestive tract and can be taken on an ongoing basis.
Corticosteroids, also known simply as steroids, are used to treat disease flares. Most drugs of this type work by suppressing the entire immune system, so they can have severe side effects and shouldnt be taken for long periods.
Biologics are made of antibodies that are grown in the lab and work by stopping certain proteins in the body from causing inflammation.
Small molecules are oral medications that also work on the immune system but act differently from biologics.
These drugs are used to treat moderate to severe ulcerative colitis.
Immunomodulators are a second-line drug for treating ulcerative colitis. These drugs limit inflammation at its source in the immune system.
Other drugs for ulcerative colitis may include antibiotics and certain pain relievers.
Also Check: Children’s Mouth Ulcers Treatment
Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
Prognosis In Ulcerative Colitis
UC is a chronic, lifelong disease. Most UC patients lead normal lives and have a typical lifespan. Fertility is similar to that in the general population, and most women are able to conceive and have children.
Some patients with UC become incapacitated by persistent or refractory symptoms. Rare complications include fulminant disease and toxic megacolon. Patients with UC are at greater risk of developing colorectal cancer than the general population.11 This risk is related to the extent and persistence of inflammation and the duration of the disease. Today, with the use of regular surveillance for precancerous changes and effective treatment, the risk of cancer has been markedly reduced.
Recommended Reading: How To Know You Have An Ulcer
Changes To Make To Your Diet To Help With Uc
Eating a healthy and well-balanced diet is important even for mild cases of ulcerative colitis. This could help prevent it from getting worse. While research hasnât found which specific foods cause ulcerative colitis symptoms, you may have certain âtrigger foodsâ that can make symptoms worse. Talk with your doctor about creating a meal plan. They may refer you to a dietitian who can help you find a pattern.
A diet for ulcerative colitis generally involves:
- Limiting dairy. People often find that this reduces diarrhea, cramps, and gas.
- Eating smaller meals. You may feel less discomfort if you eat five or six small meals a day instead of just a few large ones.
- Drinking lots of liquids. Stick to water and other flat, sugar-free beverages. Donât drink too much alcohol or caffeine, which stimulates your intestines, or soda or sparkling water, because carbonation can make you gassy.
- Avoid greasy, sugary, and high-fiber or âgassyâ foods. This includes takeout, sweets, and bowel-moving foods like bran, beans, and broccoli.
When To Seek Medical Advice
You should see your GP as soon as possible if you have symptoms of ulcerative colitis and you haven’t been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms. If necessary, they can refer you to hospital for further tests.
Read more about diagnosing ulcerative colitis.
If you’ve been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact your GP or care team for advice. You may need to be admitted to hospital.
If you can’t contact your GP or care team, call NHS 24 111 service or contact your local out-of-hours service.
Read Also: Can Ulcerative Colitis Cause Vomiting
Whats The Difference Between Ulcerative Colitis And Crohns Disease
UC and Crohns disease are the most common forms of IBD. Both conditions are thought to be the result of an overactive immune system.
They also share many symptoms, including:
However, UC and Crohns disease do have distinct differences. Understanding the key differences between them can help you obtain a proper diagnosis.
Location
These two conditions affect different portions of the GI tract.
Response to treatment
Similar medications are prescribed to treat both conditions. Surgery is also a treatment option. Its a last resort for both conditions, but it can be a cure for UC, whereas its only a temporary therapy for Crohns.
Is It Important To Treat A Flare Early Or Is It Ok To Wait A Bit
Inflammation typically does not resolve without treatment and early intervention has a better outcome than waiting to treat. At an early stage of a flare, a more optimal baseline treatment is often enough to get the inflammation under control. If you wait, there is a greater risk that you might need drugs with greater side effects, such as oral steroids. By waiting, you will have to manage longer with your symptoms before getting relief. Living with constant or longer periods of inflammation might increase your risk for future complications, as inflammation might cause damage to the gut wall that accumulates in severity with each flare.
If you are experiencing worsening symptoms, you have probably already had the flare for some time without symptoms. Evidence shows that a stool test for inflammation in the colon, called fecal calprotectin, is often elevated for two to three months before any symptoms appear. Your colon might also start to show visual evidence of inflammation before you have symptoms, or at least indicate an increased risk for a flare.
You May Like: Best Remedy For Stomach Ulcer
What Symptoms Do Colitis And Ulcerative Colitis Share
Colitis can cause similar belly and bowel issues no matter the cause. Some symptoms are mild while others are more serious.
General signs of colitis and UC include:
- Stomach cramps that come and go
- Constant belly pain
- Mucus or blood in your poop
- Weight loss without trying
- An urgent need to poop
- A feeling like you didnât get all your poop out
If you have periods, you may have:
- Worsening diarrhea during your period
Treatment Options For Crohns Disease
Recommended treatments may vary based on your symptoms and specific health history.
If you have mild to moderate Crohns disease your doctor may recommend:
- Aminosalicylates, like sulfasalazine
If you have moderate to severe Crohns disease, your doctor may recommend:
- Corticosteroids, such as prednisone and prednisolone
- Immunomodulators, like azathioprine and 6-mercaptopurine
- Biologics, like vedolizumab , adalimumab , infliximab , and ustekinumab
If you have severe Crohns disease or an acute flare-up, your doctor may recommend:
- Intravenous corticosteroids, such as methylprednisolone
Regardless of your level of severity, your doctor may prescribe broad-spectrum antibiotics if you have any abscesses or fistulas.
Also Check: Best Anti Diarrhea Medicine For Ulcerative Colitis
Study Selection And Data Extraction
Two researchers will independently conduct the literature retrieval, literature screening, data extraction and quality evaluation procedures. In case of disagreements, they will consult other researchers and negotiate using the original data. The 2 researchers will identify relevant literature by reading the titles, abstracts, and full-texts of the studies retrieved during the searches with reference to the eligibility criteria mentioned above. The process of study selection will be summarized in the PRISMA flowchart in Fig. Fig.1.1. The search results will be managed by NoteExpress 2.0 . The following information will then be extracted from the studies selected for inclusion using a preestablished literature extraction table: author, article title, year of publication, contact information, country, sample size, participants, diagnosis criteria, baseline characteristics, study design, randomization method, blinding, experimental intervention, control intervention, duration, treatment frequency, outcomes, adverse events, etc. The original authors of any articles which are found to have missing information will be contacted as much as possible in an attempt to obtain the data, or to perform data conversion. If the data does not prove to be available, the study in question will be discarded.
How Do Doctors Treat Ulcerative Colitis
Doctors treat ulcerative colitis with medicines and surgery. Each person experiences ulcerative colitis differently, and doctors recommend treatments based on how severe ulcerative colitis is and how much of the large intestine is affected. Doctors most often treat severe and fulminant ulcerative colitis in a hospital.
You May Like: How Does Alcohol Affect Ulcerative Colitis
Favorite Ulcerative Colitis Blogger
Sam Cleasby created her blog in 2013 to raise awareness of IBD and her struggles with self-esteem. Cleasby also has a radio show on BBC Radio Sheffield in which she shares about modern family life, including relationships, disability, nutrition, and kids. You can subscribe to her blog via email or follow her on or .