What Are The Risk Factors Of Ulcerative Colitis
It is estimated that as many as one million Americans have IBD with that number evenly split between Crohns disease and ulcerative colitis. Males and females appear to be affected equally. The usual age of diagnosis with ulcerative colitis is in the mid-30s, although the disease can occur at any age. Men are more likely than women to be diagnosed with ulcerative colitis in their 50s and 60s. The incidence is greater in whites than non-whites, and a higher incidence is found in Jews than in non-Jews.
IBD tends to run in families. Studies have shown that up to 20 percent of patients with ulcerative colitis will have a close relative with either Crohns disease or ulcerative colitis. There is no way to predict which, if any, family members will develop ulcerative colitis.
Home Remedy For Ulcerative Proctitis With Chitosan
Chitosan is an all-natural Chinese medicine based on chromium and amongst the best natural remedies for ulcerative proctitis with hemorrhage. Its made from natural marine red crab shells, this medicine has no contraindications.Take two pills per day around 5-7 in the morning on an empty stomach.The easiest way is to dissolve the capsules in ½ cups of warm water beforehand. In addition, licorice tea is amazing.
How Is Proctitis Detected
A health care professional may take a blood sample of your blood and send the sample to a lab to test. A blood test can show signs of certain conditions and diseases that can cause proctitis, such as STDs and other infections. rectal culture link. A rectal culture can show signs of infections that cause proctitis.
Recommended Reading: Is Omeprazole Good For Ulcers
Medications Used To Treat Ulcerative Colitis
Currently, there is no cure for ulcerative colitis. The goal of medical treatment, therefore, is to modulate the inflammatory response. Several groups of drugs are used to treat ulcerative colitis. They are:
Reducing Diarrhea Bloating And Gas
Certain foods can worsen symptoms of your condition and aggravate your rectum. Mayoclinic.com recommends limiting dairy intake to reduce diarrhea. In some cases, you might need to eliminate it completely. You should work with a dietitian to ensure adequate calcium intake from other sources.
Foods that contribute to gas and bloating include cruciferous vegetables like broccoli and cabbage, beans, popcorn, fatty and greasy foods and raw fruit juice. Alcohol and caffeine stimulate the intestines, which can worsen diarrhea, while carbonated drinks can cause gas.
Read Also: Ulcerative Colitis Back Pain Treatment
What Research Is Happening On The Coronavirus And Crohns And Colitis
Scientists and healthcare professionals across the world are united in their mission to better understand the coronavirus, to find treatments and develop a vaccine. This includes the dedicated community of Crohns and Colitis researchers and IBD teams. There are many current and future studies on the coronavirus and Crohns and Colitis, investigating areas such as:
- Symptoms, like pain or gastrointestinal symptoms, and flares during the pandemic.
- The impact of different Crohns and Colitis medicines on the severity of COVID-19 illness.
- The development of antibodies in people with Crohns and Colitis in those infected with the coronavirus or in response to the vaccine.
Complementary Treatments And Therapies
You may consider these approaches in addition to what your doctor prescribes. But itâs important to talk to your medical team about any and all of them because some, like supplements, can interfere with treatments from your doctor. Letâs take a look at a few:
Mind-body therapies:Stress and anxiety are well-known triggers for many people with ulcerative colitis, so it is not surprising that mind-body relaxation techniques could help. These techniques help nurture a healthy connection between your mind and body as well as between you and the outside world. In some cases, they encourage behavior changes in your everyday life. They may be worthwhile if only to lessen anxiety and depression linked to UC and improve quality of life. In addition, there is some evidence that yoga, meditation, and gut-centered hypnotherapy could help with some physical symptoms or flare-ups of UC. Some of the techniques, like cognitive behavioral therapy and patient support groups, have been so successful that they have slowly become a part of mainstream treatment for IBD.
Keep in mind that the FDA doesnât regulate supplements, so claims on packaging may not be accurate. Thatâs yet another reason why itâs important to talk to your doctor before you start taking any supplements for your UC.
Recommended Reading: Difference Between Ulcerative Colitis And Crohn’s Disease Ppt
What Are The Potential Complications Of Ulcerative Proctitis
Frequent bleeding due to ulcerative proctitis can lead to anemia, a condition where you dont have enough red blood cells to carry oxygen to the various tissues in your body, or iron deficiency, says Dr. Yoon. According to the National Institutes of Health , if your proctitis isnt treated or doesnt respond to treatment, complications can also include:
- Rectal stricture, which is an abnormal narrowing of the rectum
- Ulcers, or sores in the lining of the intestines
Progression to ulcerative colitis can also lead to other complications. With any severe inflammation, theres a risk for perforation of the colon wall, which weakens the whole colon, says Dr. Lerrigo. This means long-term inflammation of the colon has compromised the intestine wall so much that a hole forms, which can be very dangerous, as bacteria can infiltrate places it shouldnt be and cause an infection3.
Chronic inflammation in any organ for a long period of time causes damage at the cellular level, increasing the risk of colon cancer, Dr. Lerrigo adds. Thats why he recommends colonoscopies every year to two years for people who have progressed to ulcerative colitis and have had severe symptoms for many years.
Autoimmune Diseases And Your Va Benefits Claim
Autoimmune disease is a term that covers at least 80 different known conditions. An autoimmune disease or autoimmune disorder occurs when the immune system is unable to distinguish between foreign invaders and healthy tissue, producing antibodies that destroy the bodys own tissue instead of the infection.
Some of the most commonly-recognized autoimmune diseases include lupus, rheumatoid arthritis, ulcerative colitis, Crohns disease, celiac disease, psoriasis, and fibromyalgia. Autoimmune diseases can be debilitating and they are difficult to diagnose because symptoms are broad, including fatigue, chronic joint pain, digestive problems, muscle weakness, inflamed skin, hair loss, and chronic, unspecified pain.
Rules for VA Compensation
In order for you to receive compensation through the VA, you must have been honorably discharged, served on active duty or in active or inactive duty training, and have a disability rating for your service-connected condition. In addition, one of the following must be true:
- You got sick or injured while serving in the military and can link this to your current illness or injury
- You had an illness or injury before joining the military which was worsened by your service
- You have a disability-related to your active-duty service that did not appear until after you ended service
Connecting Autoimmune Disease to Your Service
Read Also: How To Gain Muscle With Ulcerative Colitis
Ways To Manage Up And Uc
When it comes to treating both UP and UC, there are a number of different paths you can take. But unfortunately, there isnt a cure for either condition yet.
Like most inflammatory conditions, treatment of UP and UC is multifaceted. Your treatment plan will be designed to ease your , while also addressing the underlying inflammation. The end goal of treatment is to help you reach remissiona period of time when you are symptom-free. Your will depend on the severity of your condition, and may involve a combination of therapies, says Dr. Kinnucan. For example, if your symptoms are relatively mild and limited to the rectum, then your doctor may recommend rectum therapies such as steroids and mesalamine , Dr. Kinnucan says. In more severe cases, or if the inflammation has spread into other parts of the colon, systemic medications like biologics or other small molecule therapies may be necessary, she adds.
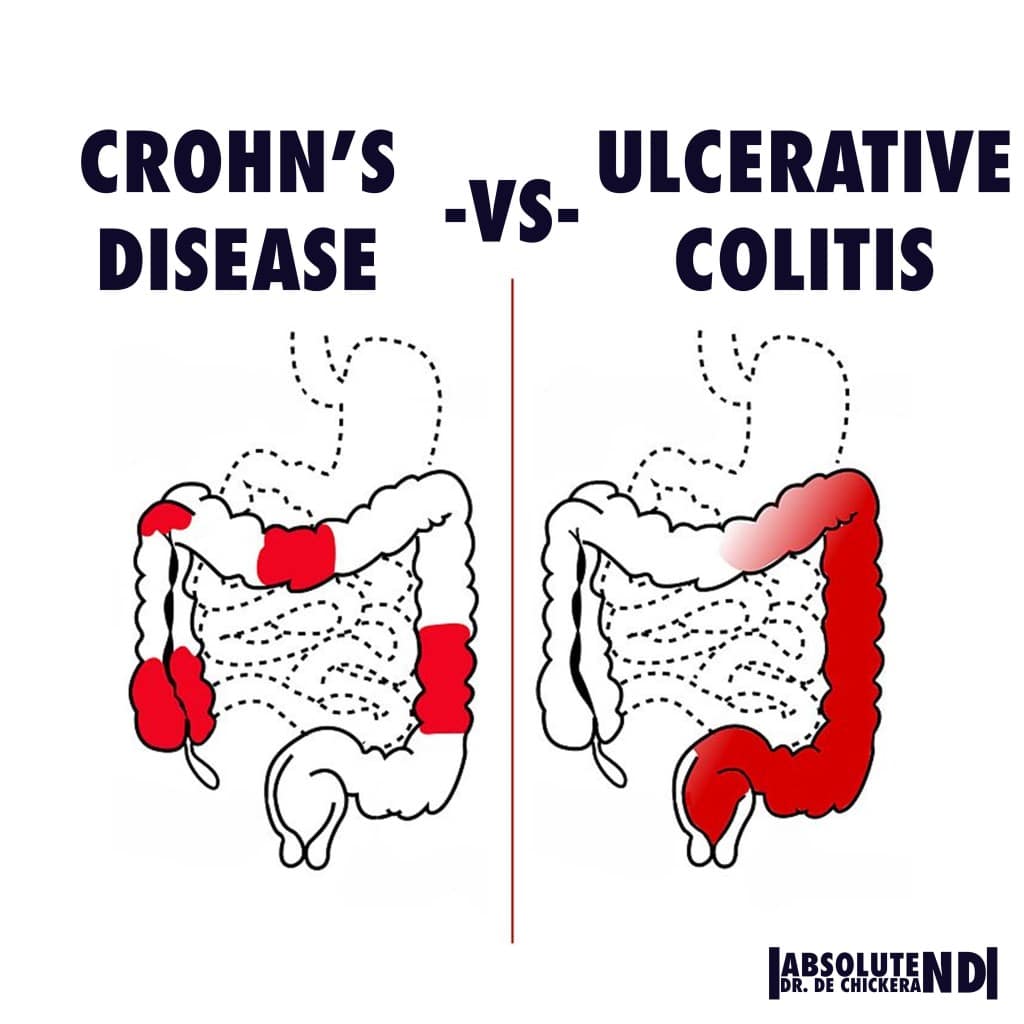
How Can I Tell If I Have Ulcerative Colitis Or Crohns Disease
Its important that you, your healthcare provider, and a GI specialist work together closely to figure out whats causing your symptoms. This is especially important since the symptoms of Crohns disease and ulcerative colitis can be similar. Your providers may check blood work and a stool sample. To get an accurate diagnosis, your GI specialist may do a colonoscopy, where a camera is pushed into the colon. Your provider will look at the inside of the colon and take tissue samples, which are important for making the right diagnosis. Your providers might get a CT scan or an MRI of your abdomen to check for complications related to your condition.
Recommended Reading: Ulcer Symptoms Blood In Stool
Does Ulcerative Proctitis Always Progress To Ulcerative Colitis
Getting treated for ulcerative proctitis can ease symptoms and even lead to remission, meaning you may not experience symptoms for a certain period of time, but thats not quite the same thing as a cure.
Progression of the disease can happen, but its not super common, although being younger at the time of your diagnosis tends to be a risk factor for more severe disease throughout life, adds Dr. Lerrigo.
Less than 15% of people with ulcerative proctitis go on to develop full-blown ulcerative colitis, according to the National Organization for Rare Disorders . A majority of the time, people with ulcerative proctitis just have ulcerative proctitis. It doesnt necessarily progress to other areas of the colon, Dr. Yoon says. In most people with IBD, wherever the disease is located, it usually stays in that area.
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
Recommended Reading: Can Ulcerative Colitis Lead To Crohn Disease
Symptoms Of Ulcerative Proctitis
The presenting symptoms of ulcerative proctitis all relate to the rectum. Blood in the stool occurs in almost everyone with the disease. Diarrhea is a common symptom, although constipation can also develop as the body struggles to maintain normal bowel function.
Inflammation of the rectum may cause a sense of urgency to have a bowel movement, discomfort after having a bowel movement, and a sensation of incomplete emptying of the bowels. Systemic symptoms such as fever, tiredness, nausea, and weight loss are rare.
The Main Types Of Drugs
The aim of drug treatment for Ulcerative Colitis is to reduce inflammation. The main types of drugs are:
Aminosalicylates reduce inflammation in the lining of the intestine. Examples include mesalazine , olsalazine , sulphasalazine and balsalazide .
Corticosteroids work by blocking the substances that trigger allergic and inflammatory responses in your body. They include prednisolone, prednisone, methylprednisolone, budesonide , hydrocortisone and beclometasone dipropionate .
Immunosuppressants suppress the immune system, and reduce levels of inflammation. The main immunosuppressants used in IBD are azathioprine , mercaptopurine or 6MP , methotrexate, ciclosporin and tacrolimus. They are often used in patients who relapse when they come off steroids.
Biological drugs are the newest group of drugs used to treat IBD. Anti-TNF drugs, such as infliximab , adalimumab and golimumab target a protein in the body called TNF, or tumor necrosis factor, preventing inflammation. Another type of biological drug is vedolizumab , which works by stopping white blood cells from entering the lining of the gut and causing inflammation.
You can find more information about some of the drugs used for Colitis: Adalimumab, Aminosalicylates , Azathioprine and Mercaptopurine, Biologic Drugs, Golimumab, Methotrexate, Infliximab, Steroids, Ustekinumab and Vedolizumab.
About a quarter of people diagnosed with Crohnâs or Colitis are children or adolescents at the time they are diagnosed.
Recommended Reading: Best Treatment For Leg Ulcers
Targeted Synthetic Small Molecules
According to the Crohns and Colitis Foundation, medications called targeted synthetic small molecules affect specific parts of the immune system and reduce inflammation.
People with UC who experience difficult responses to other treatments may benefit from targeted synthetic small molecules due to their structure, which allows them to diffuse more efficiently in the body.
Examples of targeted synthetic small molecule drugs include tofacitinib, upadacitinib, and ozanimod.
Can Ulcerative Proctitis Lead To Ulcerative Colitis
The inflammation in ulcerative colitis often begins as ulcerative proctitis, limited to the colon, according to the Cleveland Clinic. If left untreated, the inflammation can spread and affect a portion of the colon, or the entire colon. In about 30% to 50% of those with ulcerative proctitis, the condition progresses to ulcerative colitis.
UP can also cause other symptoms beyond the colon, Dr. Kinnucan adds. Patients with ulcerative colitisand even those with UPcan experience extraintestinal manifestations of their disease, including joint discomfort, she says. Beyond joint pain, people with UP may also develop complications with their skin, bones, eyes, kidneys, and liver, says the Crohns and Colitis Foundation.
Read Also: Venous Stasis Ulcer Treatment Dressings
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
You May Like: Can Diverticulitis Cause Ulcerative Colitis
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
Also Check: What To Drink With Ulcerative Colitis
What If Proctitis Is Not Treated
Proctitis that is not treated or does not respond to treatment may lead to complications, including
- Severe bleeding and anemiaa condition in which red blood cells are fewer or smaller than normal, which means less oxygen is carried to the bodys cells
- Abscessespainful, swollen, pus-filled areas caused by infection
- Ulcers on the intestinal lining
- Fistulasabnormal connections between two parts inside the body
People with proctitis symptoms need medical attention. If diagnosed with proctitis, patients should take all medications as prescribed and see their doctor for a followup appointment to be sure the cause of the inflammation has been treated successfully.
Dietary And Lifestyle Modifications

As most nutrients are absorbed higher up in the digestive tract, persons with ulcerative proctitis generally do not have nutrient deficiencies however, other factors may influence an individuals nutritional state. Disease symptoms may cause food avoidance, leading to food choices that might not provide a balanced diet. If bleeding is excessive, then modifications to the diet will be necessary to compensate for this.
Better overall nutrition provides the body with the means to heal itself. It is important to follow Canadas FoodGuide, but some foods may irritate the rectum and increase symptoms, even though they do not affect the disease course. The customized recommendations of a registered dietitian can address your sensitive digestive tract.
Donât Miss: How To Heal Mouth Ulcers Fast
You May Like: How To Treat Ulcers In The Colon
What Is The Prognosis Of Ulcerative Colitis
Ulcerative colitis is characterized by periods of remission and relapse.
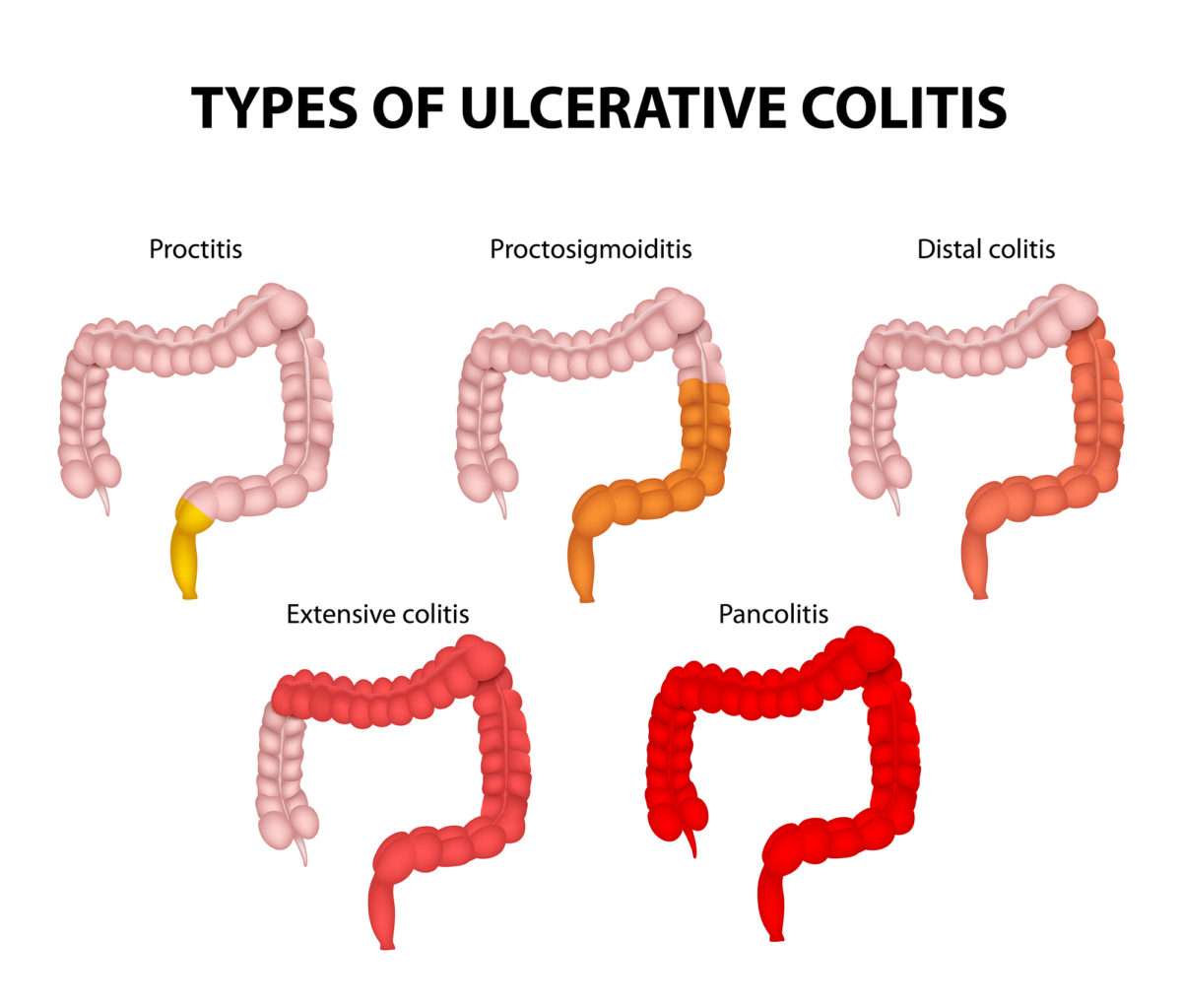
Patients with long-standing ulcerative colitis are at an increased risk for developing colorectal cancer. The risk of developing colorectal cancer depends on:
- Disease duration: The risk increases 8-10 years after onset of symptoms.
- Extent of the disease: The risk is higher in patients with pancolitis , lower in those with only left-side colitis and not increased in those with ulcerative proctitis .
It is recommended a follow-up with a sampling of multiple biopsies repeated every 1â3 years.
Are Inflammatory Bowel Diseases Different From Irritable Bowel Syndrome
Yes! IBD and IBS are very different, even though the symptoms can be similar. Most importantly, the treatments are not the same. Working with your provider to figure out what condition you have is important so that you can find the best treatment.
IBS is much more common than IBD. About 11% of people have IBS. That makes it about 10 times more common than IBD.
Fortunately, its also less serious. IBD is caused by inflammation and damage to the GI tract. With IBS, this isnt the case. IBS is a collection of gut symptoms caused by unusual functioning of the bowel.
Also Check: What Causes Ulcers On Your Feet