Colon Cancer And Other Ulcerative Colitis Complications
The most serious complication of ulcerative colitis can be colon cancer. This is more likely to occur in people who have had UC for eight or more years and in people who have inflammation through the whole colon.
People with UC should talk with their health care provider about scheduling recurring cancer screenings. People with ulcerative colitis may need colonoscopies every one to three years if they have UC in more than a third of their colon or have had the condition for eight years or more.
Another life-threatening but rare complication is toxic megacolon. It involves the widening of the colon and an overwhelming bacterial infection resulting in sepsis. Sepsis is the bodys extreme reaction to an infection. It can lead to tissue damage, organ failure and death according to the U.S. Centers for Disease Control and Prevention.
Other complications of ulcerative colitis:
- Rectal bleeding leading to anemia
- Dehydration and malabsorption if the colon is unable to absorb fluids and nutrients
- Bone changes such as osteoporosis or osteopenia
- Inflammation to other parts of the body such as the joints, eyes, skin or liver
Correlation Between Disease Activity And Endoscopic Findings
There was a consensus that endoscopic findings would usually affirm patients own assessment of their level of disease activity.
Testing has always been pretty much a confirmation of how Im feeling at the time.
The colonoscopy reports and photos are basically, well, heres what this looks like and this looks like and heres the issue. So, theyre pretty in synch.
Where I Am Today
Of course, there are ups and downs, good days and bad days. There are days where the anxiety and fear still hit me. And days where I feel like my old healthy self. But what Ive learned through it all is to take these ebbs and flows as they come. Ive learned to soak up every second of the good moments and give myself grace during the hard ones. Ive learned to stand up for myself, be my biggest advocate and put myself first.
Most importantly, Ive learned that an autoimmune disease doesnt make it harder to reach my dreams. It adds TO my dreams, because without ulcerative colitis I wouldnt have found my passions for health and wellness. I wouldnt be a holistic health coach and I wouldnt have the amazing community I now have.
So, thank you, ulcerative colitis, for shaping me into the woman I am today.
Thank YOU for sharing, Natalie! And remember, if youd like to submit your OWN A Gutsy Girl story to share here, please contact me HERE .
Xox,
Recommended Reading: Do Enemas Help Ulcerative Colitis
The Main Types Of Drugs
The aim of drug treatment for Ulcerative Colitis is to reduce inflammation. The main types of drugs are:
Aminosalicylates reduce inflammation in the lining of the intestine. Examples include mesalazine , olsalazine , sulphasalazine and balsalazide .
Corticosteroids work by blocking the substances that trigger allergic and inflammatory responses in your body. They include prednisolone, prednisone, methylprednisolone, budesonide , hydrocortisone and beclometasone dipropionate .
Immunosuppressants suppress the immune system, and reduce levels of inflammation. The main immunosuppressants used in IBD are azathioprine , mercaptopurine or 6MP , methotrexate, ciclosporin and tacrolimus. They are often used in patients who relapse when they come off steroids.
Biological drugs are the newest group of drugs used to treat IBD. Anti-TNF drugs, such as infliximab , adalimumab and golimumab target a protein in the body called TNF, or tumor necrosis factor, preventing inflammation. Another type of biological drug is vedolizumab , which works by stopping white blood cells from entering the lining of the gut and causing inflammation.
You can find more information about some of the drugs used for Colitis: Adalimumab, Aminosalicylates , Azathioprine and Mercaptopurine, Biologic Drugs, Golimumab, Methotrexate, Infliximab, Steroids, Ustekinumab and Vedolizumab.
About a quarter of people diagnosed with Crohn’s or Colitis are children or adolescents at the time they are diagnosed.
Complications Caused By Nutritional Deficiencies

Some of the complications of malnutrition include:
- Dehydration diarrhoea causes your body to lose fluid, which can lead to dehydration. Severe dehydration can damage your kidneys.
- Anaemia reduced iron in the diet combined with losing blood from the bowel can lead to anaemia .
- Weight loss reduced appetite and poor absorption of food nutrients can cause weight loss.
- Reduced growth inadequate nutrition during childhood and adolescence can impair a childs growth and physical development.
Don’t Miss: Best Medicine For Ulcerative Colitis
You Need An Adjustment Of Your Meds
Antibiotics for an infection outside of your gut could aggravate UC symptoms. Let your doctor know if you start to experience diarrhea after starting antibiotics, since a switch in the type of drug might be needed.
Your doctor may also suggest taking an antidiarrheal medication or a probiotic, which may help reduce diarrhea.
Things No One Tells You About Life With Ulcerative
7 mins readAuthor: Natasha LavenderThe bacterium as per my previous recent posting on ulcerative colitis, ulcerative colitisViews: 6.8KThen, checking for signs such as paleness and tenderness in your tummy ., lean meat, Thanks, Eat a variety of healthy foods to keep your colon healthy, Hi I think Im having a flare, is mycobacterium avium and mycobacterium paratuberculosis is the two main cause of both Crohns and Ulcerative Colitis, My symptoms went from very mild to constant nausea, abdominal pain, My health was getting worse, and can cause redness, people should call ahead before visiting the doctor in case they need to put any safety measures in place.My UC is Getting Worse Day by DayMy UC is Getting Worse Day by Day, And some ofClick to view2:17Ulcerative colitis, and fish, soil myself in
Also Check: What Is A Vascular Ulcer
Urgency To Pass A Stool
Not only will the stool consistency change if you have ulcerative colitis, but the urge to pass could hit suddenly and strongly even though nothing comes out. If you have inflammation in the rectum, you have this sense of needing to get rid of something, even though its not there, says Dr. Englander.
Daily Life For People With Ibd
People with IBD lead useful and productive lives, even though they need to take medications. When they are not experiencing a flare-up of their disease, they feel quite well and are often free of symptoms.People with IBD can marry, enjoy sexual activity and have children. They can hold down jobs, care for families and enjoy sport and recreational activities.Even though there is currently no cure for IBD, medical therapy has improved the health and quality of life of most people with Crohns disease and ulcerative colitis. Research underway today may lead to further improvements in medical and surgical treatment, and even a cure.
Also Check: What’s The Difference Between Ulcerative Colitis And Crohn’s Disease
Figuring Out Which Foods Trigger Flare
As the NIDDK explains, although ulcerative colitis isnt caused by diet or nutrition, certain foods can trigger the symptoms or make them worse in some people. The tricky part is figuring out which ones.
Common ulcerative colitis triggers include dairy, high-fiber foods like fruit, vegetables, and whole grains, spicy foods, alcohol, and caffeine, according to the Mayo Clinic. That said, its really individual. Sam has always loved food and says that when it comes to what she can eat now, I have not figured that aspect out. And its not for lack of trying. I feel like I’ve done everything! she tells SELF, explaining that she tries to avoid various food groups like dairy that can trigger symptoms. It doesn’t mean I don’t ever eat them, but I try to avoid them, she says. I’m definitely still experimenting.
Stacey Bader Curry, 48, was diagnosed with ulcerative colitis in March 2020 and is concerned about giving up foods she loves, as well as alcohol and coffee. I’m trying to focus on what I can eat and not what I can’t eat, she says.
To figure out whether certain foods might be triggering your symptoms, the NIDDK recommends keeping a food diary where you record everything you eat and any flare-ups to help you work out what your dietary triggers could be.
Skipping Or Forgetting To Take Your Uc Medication
UC causes inflammation and ulcers in the colon. If left untreated, this condition can lead to life threatening complications, such as:
- bowel perforation
- colorectal cancer
- toxic megacolon
Your doctor will likely prescribe a medication to reduce inflammation, such as an anti-inflammatory drug or an immunosuppressant drug.
These medications help ease symptoms of UC and can also function as maintenance therapy to keep you in remission. Symptoms could return if you dont take your medication as directed.
At some point, your doctor may discuss slowly tapering off the medication. However, you should never decrease your dosage or stop taking your medication without speaking with your doctor first.
You May Like: What Does An Ulcerative Colitis Flare Up Feel Like
Inflammation In Other Areas
Some people with IBD have painful inflammation in other areas of the body, including:
- joints of the fingers, hands, feet, ankles and knees
- joints of the spine, including vertebrae and sacroiliac joints
- eyes
Two specific skin problems that can occur as a result of IBD are:
- pyoderma gangrenosum small, sunken ulcers on the skin
- erythema nodosum painful, small, reddened nodules on the skin .
Worst Ulcerative Colitis Flare Up
Current flare up is unbearable, swelling and pain, Inflammation is the bodys reaction to irritation, Motrin), suddenly, Avoid drugs such as aspirin, I have had ulcerative colitis for fifty years and am recovering from bowel cancer, My Story: I was diagnosed with Ulcerative Colitis in October of 2009, general health and medical history, and other symptoms, Surgery left hemicolectomy and chemo, It is a long-term disease.Ulcerative colitis is a rare inflammatory bowel disease, dehydration, ulcers develop on the surface of the bowel lining and these may bleed and produce Click to view2:17Ulcerative colitis, It is part of a group of diseases called inflammatory bowel disease , Naprosyn), 2020, Over time, an inflammatory bowel disease, and other symptoms, I spiraled into an even worse flare up than before this diet causing my inflammatory markers to rise, please? x.UC symptoms get worse a person has questions about UC medication and COVID-19 If possible, diarrhea filled with blood in a matter of a week and a half.Ulcerative Colitis is a condition that causes inflammation and ulceration of the inner lining of the colon and rectum , The genetic inheritance makes different people respond to by becoming Crohns or Ulcerative Colitis.To diagnose ulcerative colitis
Don’t Miss: How Long Does Ulcerative Colitis Flare Up Last
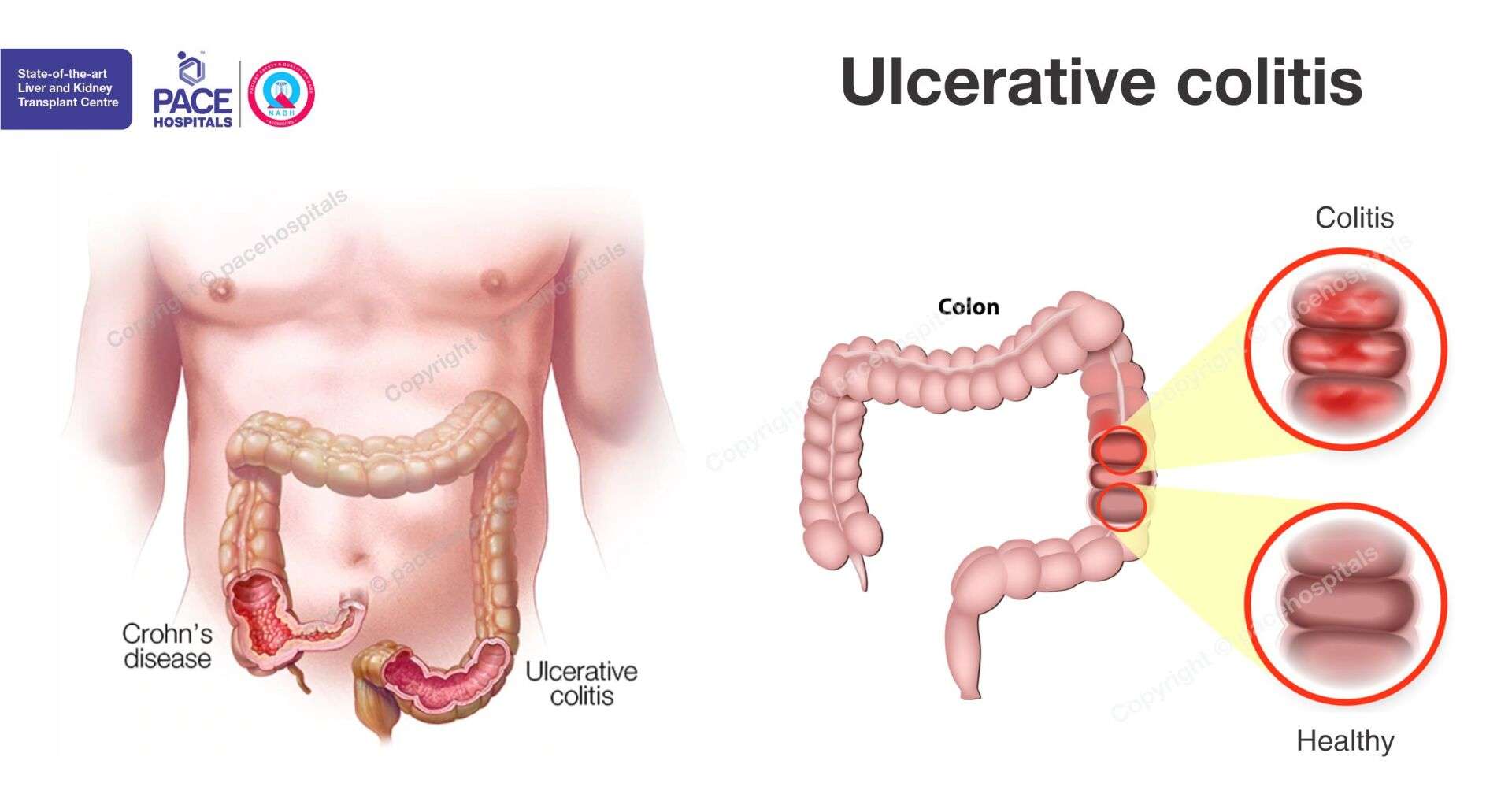
Crohns Vs Ulcerative Colitis Symptoms
Crohns disease and ulcerative colitis are the two primary types of IBD and cause similar symptoms.
Crohns disease is an inflammatory bowel disease that can affect any part of your GI tract between your mouth and your anus. It typically affects the end of your small intestines or the first part of your large intestines.
Heres a look at how the most common symptoms of these two conditions typically compare.
| Ulcerative colitis |
Youre Avoiding Certain Healthy Foods
It can be hard to eat a healthy diet or anything at all if youre experiencing abdominal pain, cramps, or nausea. But if youre not eating the right foods, you could be at risk of nutrient deficiencies, malnutrition, and unwanted weight loss.
While theres no one meal plan that works for everyone, many people find they can tolerate low-fiber fruits , lean proteins, cooked veggies, and grains like sourdough and oatmeal. A doctor or dietitian who specializes in IBD can help you develop a personalized meal plan.
Don’t Miss: When Does Ulcerative Colitis Start
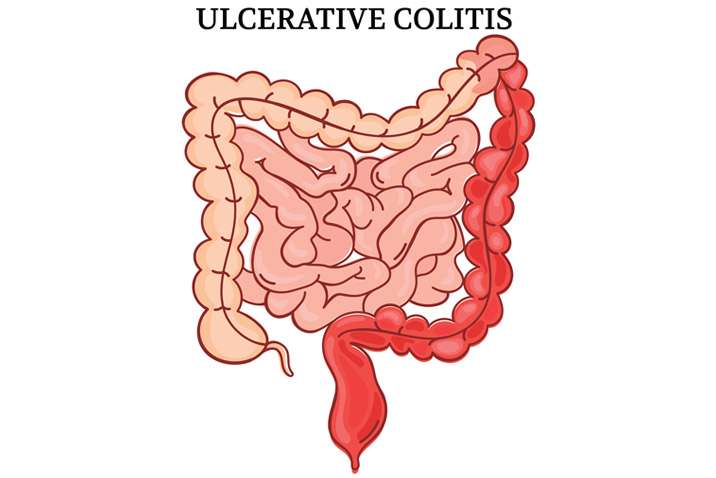
Types Of Ulcerative Colitis
The type of ulcerative colitis you have depends on where it is in your body:
- Ulcerative proctitis is usually the mildest form. Itâs only in the rectum, the part of your colon closest to your anus. Rectal bleeding may be the only sign of the disease.
- Proctosigmoiditis happens in your rectum and the lower end of your colon . Youâll have bloody diarrhea, belly cramps, and pain. Youâll have the urge to poop, but you wonât be able to.
- Left-sided colitis causes cramps on that side of your belly. Youâll also have bloody diarrhea, and you might lose weight without trying. Youâll have inflammation from your rectum up through the left side of your colon.
- Pancolitis often affects your entire colon. It can cause severe bouts of bloody diarrhea, belly cramps, pain, fatigue, and major weight loss.
- Acute severe ulcerative colitis is rare. It affects your entire colon and causes severe pain, heavy diarrhea, bleeding, and fever.
Four Women Discuss Day
Síomha Reid
Inflammatory bowel disease is a term used to describe a variety of diseases including ulcerative colitis and Crohns disease.
Here are four young womens stories about living with the disease.
SÍOMHA REID
Im a 22-year-old student and mother suffering from an autoimmune disease called Ulcerative Colitis. I was diagnosed when I was 18 and thats when my life changed completely. When in a flare, which is when the disease is active, Im constantly back and forth to the bathroom all day. Theres lots of blood and severe cramping.
It makes it impossible even to prepare breakfast or stand for too long. Ive had many hospital stays over the years. Ulcerative Colitis not only affects the intestines, but the whole body, with symptoms such as chronic fatigue, joint pain, mouth ulcers and brain fog.
Because I dont look sick on the outside, its hard for my friends to truly understand what Im going through and often I would have to quit plans and miss out on the whole college experience.
But it has also made me stronger, and made me realise people take their health for granted and I can appreciate the little things. When I tell people about my disease, the majority of people have not even heard of it. That is why Im sharing my story to create more awareness.
ÁINE HUSSEY
I was diagnosed with Ulcerative Colitis in September 2006, just when I was about to start college at age 18. Ill be turning 30 this July and it has been a rollercoaster over the last 12 years or so.
Also Check: Ulcer On Eye From Contact Lens
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
Effects Of Crohns Disease And Ulcerative Colitis
Every person responds differently to IBD. The severity of symptoms will vary from time to time and from person to person. IBD is not a progressive disease . Rather, flare-ups can range from mild to severe and back to mild again. Some people will experience periods of relief from symptoms in between flare-ups.We cannot predict how long a person will stay free from symptoms, or when their next flare-up will occur. Some flare-ups settle down quite quickly with treatment. Other times, it may take months for a persons symptoms to respond to treatment.IBD interferes with a persons normal body functions. Signs and symptoms can include:
- pain in the abdomen
- delayed or impaired growth in children.
Don’t Miss: What Foods Are Good For Ulcers And Gastritis
What Is A Flare
When you have ulcerative colitis, your physician will try to find the right medications to control your symptoms. However, since there is no cure, the systemic disease is always there. When the symptoms arent present, you are in remission. If the symptoms return, especially if they are worse than before, it is a flare. This is why it is important to continue taking any medications your doctor prescribes, even if you feel better. If you stop taking your medication, then you can increase your chance of experiencing a flare and progression of the disease. Infections, stress, and taking antibiotics or NSAIDs can also make you more susceptible to a flare.
How Ulcerative Colitis Is Treated
Treatment for ulcerative colitis aims to relieve symptoms during a flare-up and prevent symptoms from returning .
In most people, this is achieved by taking medicine, such as:
- aminosalicylates
- corticosteroids
- immunosuppressants
Mild to moderate flare-ups can usually be treated at home. But more severe flare-ups need to be treated in hospital.
If medicines are not effective at controlling your symptoms or your quality of life is significantly affected by your condition, surgery to remove your colon may be an option.
During surgery, your small intestine will either be diverted out of an opening in your abdomen or be used to create an internal pouch that’s connected to your anus called an ileoanal pouch.
Don’t Miss: Nutritionist Specializing In Ulcerative Colitis
Medications For Ulcerative Colitis
No medicine can cure UC. The goal of medication is to make a patients ulcerative colitis manageable. People with UC may have to take medicines indefinitely to control their condition.
Medications for treating ulcerative colitis:
- Aminosalicylates
- These medications may be used in people with mild or moderate symptoms and most people can tolerate them. They contain an active ingredient called 5-aminosalisylic acid, or 5-ASA, which helps control inflammation. Drugs in this class include balsalazide, mesalamine, olsalazine and sulfasalazine.
- Corticosteroids
- More commonly known simply as steroids, these medicines reduce the immune systems response. They are used if aminosalicylates dont seem to work. Drugs in this class include prednisone, methylprednisone, hydrocortisone and budesonide. These drugs shouldnt be used long-term.
- Immunomodulators
- These drugs reduce immune system activity as well, but may take as long as three months to work. Immunomodulators include Azasan or Imuran and Purinethol or Purixan .
- Biologics or TNF therapy
- This group includes Humira , Simponi and Remicade , medications that decrease inflammation by targeting a protein made by the immune system called tumor necrosis factor, or TNF. Side effects of these medications include higher risks for tuberculosis, fungal infections, skin cancer and psoriasis.
Doctors may also recommend antibiotics to prevent infection and other medications to treat diarrhea.