Complications Of Ulcerative Colitis And How To Avoid Them
Learn how to identify and avoid potentially life-threatening complications of ulcerative colitis.
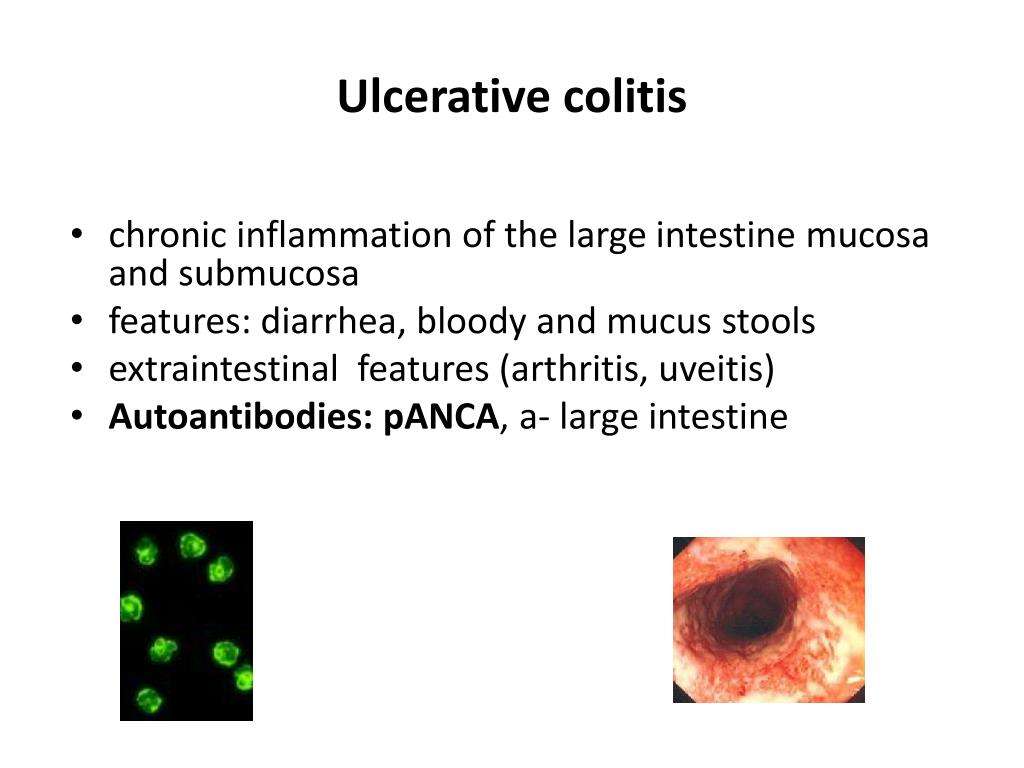
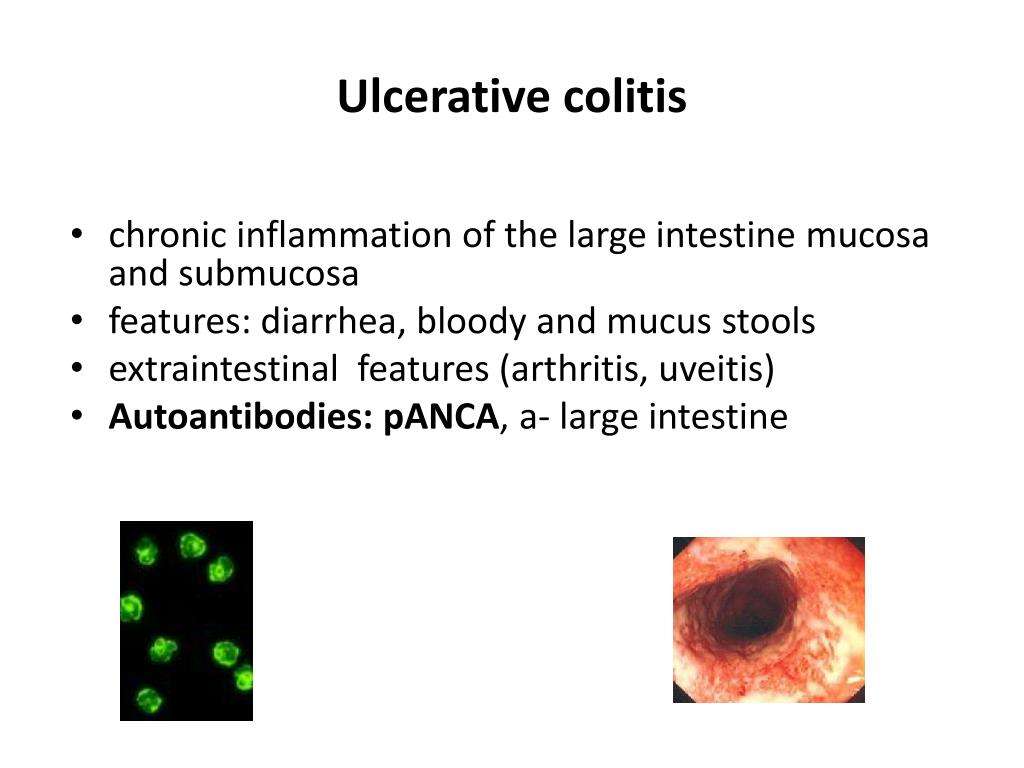
If you have an inflammatory bowel disease like ulcerative colitis , a gastroenterologist can prescribe medication and create a treatment plan for the inflammation and sores, called ulcers, that occur in the lining of the large intestine and rectum. But this autoimmune disorder is often associated with complications in other parts of the body that should be addressed as well.
Extraintestinal complications those that exist outside the intestines can even overshadow symptoms in your bowels, making UC tricky to diagnose. They are also highly prevalent, occurring in nearly half of UC patients and appearing more often in women, according to a review published in May 2019 in Current Gastroenterology Reports. While it remains unclear why UC complications can arise beyond the intestines, the review noted that genetic predisposition, irregular immune response, and changes to the gut microbiome are some common contributing factors.
“It’s easy to forget that ulcerative colitis is not just a disease of the intestines but a systemic or body-wide disorder of the immune system,” says Jessica Philpott, MD, PhD, a gastroenterologist at Cleveland Clinic in Ohio.
Below are five conditions commonly linked to ulcerative colitis, along with some treatment options.
How Do Autoimmune Diseases Affect You If You’re Trying To Get Pregnant
Some autoimmune diseases can affect your ability to get pregnant and some have adverse effects on pregnancy. You may need fertility treatments to get pregnant. You might also want to wait until your disease is in the remission stage to try to conceive.
There is a higher risk for stillbirth or preterm birth if you have lupus. If you have myasthenia gravis, you may experience trouble breathing.
Does Uc Compromise The Immune System
If a person does not manage their condition correctly, UC may lower their immune systems overall function. Excessive immune activity in the gut could mean less immune activity in the rest of the body.
The following table shows a list of immunosuppressive drugs that can treat IBD, as well as drugs that do not suppress the immune system:
| Immunosuppressant treatment for IBD |
|---|
| 5-aminosalicylates:Mesalamine, balsalazide, olsalazine, sulfasalazine |
| Immunomodulators: Azathioprine, 6-mercaptopurine, methotrexate |
, the current evidence suggests people with inflammatory bowel disease , which includes UC and Crohns disease, are not at higher risk of COVID-19 than the general population.
Immunomodulators and biologics are all unlikely to raise a persons risk of infection.
The American College of Gastroenterology adds that most people taking standard IBD therapies do not have a higher risk of getting COVID-19. They listed the following statements that a person with IBD may find useful regarding COVID-19:
2021 review found that treatments for IBD did not increase the risks of COVID-19 complications, except for people taking aminosalicylates and steroids.
In people with IBD who tested positive for COVID-19, 27% of people required treatment in a hospital, and mortality rates were less than 5%.
Researchers also found that taking biologics reduced negative outcomes.
In a position statement on COVID-19 vaccines, the Crohns and Colitis Foundation states:
Don’t Miss: Are Eggs Bad For Ulcerative Colitis
Coexistence Of Lupus Nephritis Ulcerative Colitis And Communicating Hydrocephalus: A Report Of A 21
Nida Saleem
1Shifa International Hospital, H-8/4, Pitras Bukhari Road, Islamabad, Pakistan
Abstract
Systemic lupus erythematosus and ulcerative colitis are multisystem autoimmune disorders that rarely coexist. We report a case history of a 21-year-old male, presenting with bloody diarrhea and, later, diagnosed to have ulcerative colitis on colonic biopsy. There was clinically silent renal impairment leading to end-stage kidney disease requiring hemodialysis possibly secondary to ongoing lupus nephritis as suggested by positive lupus-specific antibodies detection. Besides this, the diagnosis of lupus associated with early communicating hydrocephalus was made on CT brain findings which clinically responded well to the initiation of immunosuppressive therapy. It is imperative to keep in mind the remote possibility of ulcerative colitis in an SLE patient with gastrointestinal manifestations. Communicating hydrocephalus is a rare neurological manifestation of SLE leading to seizures and can respond well to the initiation of steroids and immunosuppressants. Therefore, a trial of immunosuppressant medications must be given even in a patient with end-stage renal disease to halter extra renal rare lupus manifestations.
1. Introduction
2. Case
| Hemoglobin | ||
| Protein: +, blood: +++, RBCs: 2025/HPF, WBCs: 1-2/HPF | ||
| Stool R/E | No cyst, ovum, or worm | Spot urine protein-to-creatinine ratio |
| Serum chloride | 97 |
| ANA | |
| Anti-Golgi apparatus antibodies | Positive |
3. Discussion
4. Conclusion
Diagnosing Inflammatory Bowel Disease In Adults
In inflammatory bowel disease, or IBD, there is persistent inflammation in the gastrointestinal tract. The condition causes symptoms such as abdominal pain, diarrhea, bloody stool, constipation, and an urgent need to have a bowel movement. The most common types of IBD are Crohns disease and ulcerative colitis.
Gastroenterologists at NYU Langone’s Inflammatory Bowel Disease Center are experts in the gastrointestinal tract and can recommend the appropriate diagnostic tests to determine the cause of your symptoms. There is no single definitive test to confirm the presence of IBD, so the condition is diagnosed based on a combination of tests, including endoscopy, biopsy, and imaging tests.
Read Also: Can Eliquis Cause Stomach Ulcers
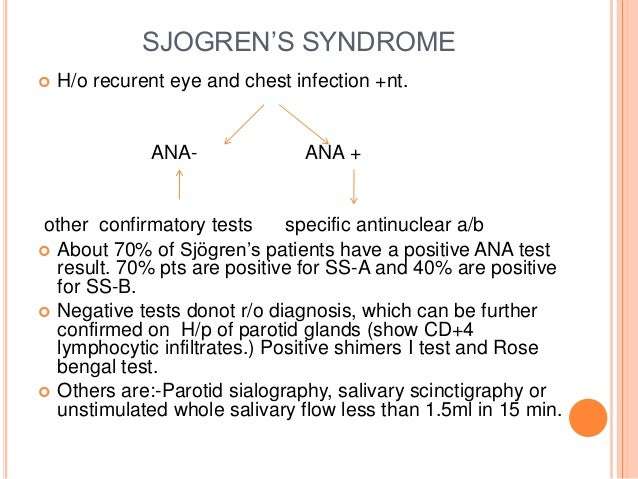
How Are Autoimmune Diseases Diagnosed
Diagnosing an autoimmune disease usually takes healthcare providers longer than it does to diagnose other diseases. This is because many autoimmune diseases have similar symptoms with each other and with other diseases. You can help your healthcare provider with the diagnosing process by bringing the following to your appointment:
- A detailed list of any symptoms and how long youve had them.
- A record of your familys health history. Note if anyone in your family has an autoimmune disease.
In addition to interviewing you about your symptoms, your healthcare provider may do some blood tests to check for autoimmune diseases, including:
- Antinuclear antibody test .
Specific symptoms combined with specific blood markers may prove that you have an autoimmune disease.
Radiologic Assessment Of Ulcerative Colitis
Imaging has an important role in the workup of patients with suspected inflammatory bowel disease and in the differentiation of ulcerative colitis and Crohn disease.
Plain abdominal radiographs are a useful adjunct to imaging in cases of ulcerative colitis of acute onset. Because of its ability to depict fine mucosal detail, double-contrast barium enema examination also is a valuable technique for diagnosing ulcerative colitis and Crohn disease, even in patients with early disease.
Cross-sectional imaging studies are useful for showing the effects of these conditions on the bowel wall.
Radionuclide studies are useful in cases of acute fulminant colitis when colonoscopy or barium enema examination is contraindicated.
Angiography may be helpful because evidence suggests microcirculatory disturbances may play an important role in the pathophysiology of ulcerative colitis.
See Ulcerative Colitis Imaging for more detailed information.
References
Murata I, Satoh K, Yoshikawa I, Masumoto A, Sasaki E, Otsuki M. Recurrent subcutaneous abscess of the sternal region in ulcerative colitis. Am J Gastroenterol. 1999 Mar. 94:844-5. .
Kimura K, Hunter SF, Thollander MS, et al. Concurrence of inflammatory bowel disease and multiple sclerosis. Mayo Clin Proc. 2000 Aug. 75:802-6. .
Egan CA, Meadows KP, Zone JJ. Ulcerative colitis and immunobullous disease cured by colectomy. Arch Dermatol. 1999 Feb. 135:214-5. .
Wiesner W, Steinbrich W. . Ther Umsch. 2003 Mar. 60:137-44. .
Don’t Miss: Can You Cure Ulcerative Colitis Naturally
How Are Autoimmune Diseases Treated
There are no cures for autoimmune diseases, but symptoms can be managed. Everyones immune system, genetics and environment are different. That means that your treatment must be unique.
Some examples of medications used to treat autoimmune diseases include:
- Painkillers.
- Limiting processed foods from your diet.
Double Contrast Barium Enema X
This is a specialized X-ray, using a contrast material to highlight the affected area. During the X-ray, your doctor can clearly see the right colon and the ileum , the two areas most often involved in Crohn’s disease.
Before the procedure, you will need to clear your colon of any stool. Preparations may include a liquid diet, enema or laxative. During a barium enema:
A barium preparation is inserted through a rectal tube.
The barium outlines the colon, highlighting any abnormalities.
An X-ray is taken.
Your doctor can look for evidence of Crohn’s disease.
You May Like: Ulcer Signs Symptoms And Treatment
Who Created The Ana Test How Do Health Care Professionals Perform The Procedure
The ANA test was designed by Dr. George Friou in 1957. The ANA test is performed using a blood sample. An ANA test is performed by testing the blood in the laboratory. The antibodies in the serum of the blood are exposed in the laboratory to cells. It is then determined whether or not antibodies are present that react to various parts of the nucleus of cells. Thus, the term anti-“nuclear” antibody. Fluorescence techniques are frequently used to actually detect the antibodies in the cells, thus ANA testing is sometimes referred to as fluorescent antinuclear antibody test .
Ways To Reduce Complications
Early intervention and frequent surveillance of ailments is key to reducing complications and improving outcomes. It’s important to maintain proper nutrition and avoid emotional stress, though neither stress nor sensitivity to certain foods causes the disease. Avoiding steroids can also be helpful if you and your doctor have an alternative way of treating UC flares.
While the cure for UC has yet to be found, when the disease is treated properly, some complications may disappear altogether. Work with your doctor and other members of your healthcare team to get optimal control of the disease as soon as possible.
Additional reporting by Jordan M. Davidson.
Recommended Reading: How To Repair An Ulcer
Prediction Of Response To Treatment
It would be of great clinical and economic significance if clinicians could utilize serological antibody measurements to predict the response to treatment and to implement individualized treatment plans based on this information. This goal is particularly important because recent biologics are costly and can be associated with serious adverse events. Infliximab, an anti-tumor necrosis factor- agent, has been reported to have little efficacy in pANCA-positive CD patients, and a subsequent study demonstrated a similar result in pANCA-positive/ASCA-negative CD patients. Infliximab also has little efficacy in pANCA-positive/ASCA-negative UC patients. Also, CD patients who responded to antibiotics were positive for anti-I2 or anti-OmpC, which are antibodies against intestinal bacteria. Furthermore, pANCA-positive UC has been reported to be resistant to medical treatments.
What Questions Might A Healthcare Provider Ask To Help Diagnose An Autoimmune Disease
When your healthcare provider interviews you, they might ask you one or more of the following questions:
- What medications are you taking?
- What are your symptoms?
- How severe are your symptoms?
- Have you had to go to the emergency department because of your symptoms?
- How long have you had these symptoms?
- In what ways are your symptoms affecting your quality of life?
- Is there anything that triggers your symptoms? Anything that makes them worse?
- Is there a history of autoimmune diseases in your family?
- Which autoimmune diseases run in your family?
- What over-the-counter or alternative medicines have you tried, if any?
You May Like: Stage 2 Pressure Ulcer Characteristics
What Is The Interpretation Of The Ana Screen Result
The ANA test is a sensitive screening test used to detect autoimmune diseases. Autoimmune diseases feature a misdirected immune system, and each of them has characteristic clinical manifestations that are used to make the precise diagnosis. The interpretation or identification of a positive ANA test does not make a diagnosis. It simply suggests to the doctor to consider the possibility that an autoimmune disease is present.
Ct Scans And Ct Enterography
CT scans involve taking a series of X-rays to create detailed two- and three-dimensional images of the body. CT scans of the gastrointestinal tract can reveal a narrowing of the small or large intestine, called a stricture, or an obstruction. The test may also indicate inflammation in the small intestine, which suggests that Crohns disease may be causing your symptoms.
Occasionally, doctors may recommend an enhanced CT scan, known as a CT enterography. Prior to the scan, you drink a contrast agent. As the liquid passes through the digestive tract, the CT scanner takes pictures of the small intestine and may reveal anatomical problems. For example, if an obstruction is present, the contrast liquid is visibly blocked.
Recommended Reading: Hind Gut Ulcers In Horses Symptoms
Are Anas Always Associated With Illness What Is The Normal Range
No. ANAs can be found in approximately 5% of the normal population, usually in low titers . These people usually have no disease. Titers of 1:80 or lower are less likely to be significant. Even higher titers are often insignificant in patients over 60 years of age. Ultimately, the ANA result must be interpreted in the specific context of an individual patient’s symptoms, underlying medical conditions, and other test results. It may or may not be significant, even if positive, in a given individual.
Systemic Lupus Erythematosus And Gastrointestinal Involvement
Gastrointestinal symptoms are common in systemic lupus erythematosus patients, and more than half of them are caused by adverse reactions to medications and viral or bacterial infections. Gastrointestinal manifestations may overshadow other aspects of the disease and mimic any type of abdominal condition. Lupus mesenteric vasculitis is the most common cause, followed by protein-losing enteropathy, acute pancreatitis, serositis intestinal pseudo-obstruction and other rare comorbidities such as celiac disease and inflammatory bowel disease . In an extensive review of the gastrointestinal and hepatic manifestations of systemic lupus erythematosus only about 10% of patients with autoimmune hepatitis had lupus and up to 4.7% of patients with SLE had chronic active hepatitis.
Imaging studies are helpful in diagnosing SLE-related gastroenteropathies. Early nondiagnostic radiographic findings include thumbprinting, pseudoobstruction and segmental bowel dilatation. Abdominal CT and arteriography may be more helpful with diagnosis but a negative arteriogram does not exclude disease because vasculitis generally involves small arteries.
Abdominal CT scan may show thickened small bowel loops with contrast enhancement consistent with small bowel ischemia. However, small bowel thickening is not a specific finding for intestinal vasculitis and may be also associated with hypoalbuminemia, IBD and gastroenteritis.
Recommended Reading: Ulcerative Colitis And Blood In Urine
Mri Scans And Mr Enterography
An MRI scan uses a magnetic field and radio waves to create two- and three-dimensional images of the body. MRI scans are especially helpful when doctors need to visualize soft tissues, such as the lining of the intestines. They may reveal small tears or ulcers, as well as irritation or bleeding.
To get a better look at the gastrointestinal tract, the doctor may ask you to drink a contrast agent just before the MRI. This is called MR enterography.
Serum Levels Of Anca Asca And The Positive Rates Among The Three Comparison Groups
Our data suggested that: The ANCA-IgG level and positive rate in UC group were significantly higher than those of disease control group and healthy control group,the differences were statistically significant There were no significant differences in ANCA-IgG level and positive rate between disease control group and healthy control group There were no significant differences in ASCA-IgA, ASCA-IgG levels and positive rate among UC group, disease control group and healthy control group. Results were shown in Table .
Read Also: How To Reduce Ulcerative Colitis
Association With Clinical Phenotypes And Prognostic Indicators
In UC, very few studies have assessed acute phase markers in predicting outcome of disease or association with clinical phenotypes. In severe UC, after three days of intensive treatment patients with frequent stools , or 3-8 stools/d and CRP > 45 mg/L should be identified, as most of them will need to undergo colectomy. It is commonly accepted that the presence of ANCA in UC is not related to the duration and age of onset. Previous studies agree that in patients affected with CD, the presence of atypical pANCAs in serum characterizes an UC-like clinical phenotype.
What Causes Autoimmune Diseases
The precise cause of autoimmune diseases is unknown. However, there are risk factors that may increase your chances of getting an autoimmune disease. Risk factors include:
- Some medications. Talk to your healthcare provider about the side effects of medications for blood pressure, statins and antibiotics.
- Having relatives with autoimmune diseases. Some diseases are genetic they run in families.
- Smoking.
- Temperature sensitivity.
Don’t Miss: Remicade Infusion For Ulcerative Colitis
Diagnostic And Differential Diagnostic Value
Previous studies have valued the usefulness of routine laboratory testing in UC. CRP is a helpful index of UC activity, but its utility, as a screening test has not been totally evaluated.
CRP is the most sensitive compared to other serologic markers of inflammation in adult population for detecting IBD. The sensitivity of CRP ranges from 70%-100% in the differential diagnosis between CD versus irritable bowel syndrome and from 50%-60% in UC. In high percentage of paediatric patients, the sensitivity of routine testing , varies from 62%-91% when evaluating the combination of 2 routine laboratory tests, whereas specificity ranged from 75%-94%.
Levels of CRP are higher in active CD than in UC and this difference might be used to differentiate between CD and UC. The measurements of circulating levels of CRP, ESR, platelets count are not useful at all for differentiation between both types of IBD.
Orosomucoid is not useful test for screening healthy populations or differentiating patients with inflammatory vs functional disorders.
The clinical usefulness of pANCA or ASCA testing in patients with non-specific gastrointestinal symptoms is limited, because of the low sensitivity. Assaying all the serum markers available for CD, the sensitivity for the diagnosis of CD is greater than 80% and the positive predictive value is over 90% but only when the prevalence of CD is > 38%.
Why Does Ulcerative Colitis Cause Joint Pain
As you can probably guess, the joint pain that occurs as a symptom of some type of Enteropathic Arthritis develops because of the inflammation caused by Ulcerative Colitis.
And no, the cause for this is yet to be found out. In normal circumstances, for some unknown reasons, inflammation occurs and affects some or more than one joint, what is later diagnosed as some type of Arthritis.
So it is not a different story this time it is still the inflammation that has first occurred because of the Ulcerative Colitis that has later only spread and affected some joints in the body, causing the common Arthritis symptoms to develop as well.
But the good news is that there are some promising suggestions for a colectomy to make the Arthritis symptoms, as well as the Ulcerative colitis symptoms, to go away.
You May Like: Can I Eat Oatmeal With Ulcerative Colitis