What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
What Causes A Flare
Say you are someone who is living with IBD, specifically Ulcerative Colitis. You are bound to experience a flare-up or five every now and then, but what causes a UC flare?
Well first lets answer what ulcerative colitis is. Ulcerative colitis is an inflammatory bowel disease or an IBD that causes inflammation in your digestive tract.
Once inflammation starts to happen, ulcers can develop in your digestive tract as well. It affects the inner lining of your colon and your rectum.
You May Also Like
So what causes inflammation or a flare-up with UC? Well, there are a few things that can cause a flare-up.
Your diet can be a reason for a flare-up. Eating dairy may cause inflammation as well as too much fiber and unhealthy or processed foods.
Stress can also cause inflammation to worsen or trigger it as well.
Perforation Of The Colon
Long-term inflammation and ulcers in the colon can weaken the intestinal wall. Over time, these weaknesses may develop into a perforation.
A perforation can allow bacteria and other intestinal contents to leak out into the abdomen, causing a serious condition called peritonitis.
Peritonitis is the inflammation of the peritoneum, which is the lining of the abdomen. This condition may cause the abdomen to fill with fluid. It can also lead to blood poisoning and sepsis, which is a whole-body inflammatory response to infection.
One in three people who develop sepsis die from the condition.
Symptoms
It is vital to know the symptoms of a perforated colon to help prevent peritonitis and sepsis. According to the , these may include:
- severe stomach pain
A perforated colon is a medical emergency that usually requires surgery to repair the hole in the intestines.
People who experience sepsis also require urgent treatment with antibiotics and fluids.
You May Like: How To Treat Stress Ulcers
What Causes Ulcerative Colitis Flare Ups In The First Place
The experts arent exactly sure what causes UC, but they think its prob an autoimmune condition. Autoimmune conditions are basically what happens when the bodys defense mechanism is a little overzealous and attacks healthy tissue. Your body *means* well, but it causes inflammation.
In the case of UC, scientists think that the immune system might accidentally mistake perfectly harmless bacteria in the colon for serious threats, which causes the whole region to essentially swell up.
Though they dont know exactly what contributes to flare ups, a few possibilities include:
- Stress. According to 2016 research, being stressed out may trigger IBD flare-ups. Even though stress doesnt seem to directly cause UC, it does appear to weaken the intestinal wall and make it more vulnerable to issues. Researchers found that stress increased microbe activity in the colon and hindered the immune response.
- Diet. In a 2020 review, researchers found a correlation between diet and UC flare-ups. However, the research on exactly what triggers them just isnt there yet.
- Certain medications. Abruptly stopping medications like steroids or maintenance therapies, which slow the bods natural cortisol levels, can lead to flares and other negative side effects. Always talk to a doc before halting these drugs.
- Hormonal changes. There seems to be a link between IBD and hormonal changes in women, with some research from 2018 suggesting that UC symptoms worsen during pregnancy in particular.
How Ulcerative Colitis Is Treated

Treatment for ulcerative colitis aims to relieve symptoms during a flare-up and prevent symptoms from returning .
In most people, this is achieved by taking medicine, such as:
- aminosalicylates
- corticosteroids
- immunosuppressants
Mild to moderate flare-ups can usually be treated at home. But more severe flare-ups need to be treated in hospital.
If medicines are not effective at controlling your symptoms or your quality of life is significantly affected by your condition, surgery to remove your colon may be an option.
You May Like: Icd 10 Code Sacral Decubitus Ulcer
What Do Chills Feel Like With Ibd
Many people with IBD experience chills. MyCrohnsAndColitisTeam members describe this symptom in different ways. As one shared, Its like I cannot get warm.
Some people find that chills are accompanied by other symptoms, like fevers: I get flu-like episodes which come on suddenly, wrote one member. Headache, very sore neck and back, big spike in temperature, alternating sweats and chills. Its gone by the next morning. Another shared, The night sweats are horrible! My sheets are soaked every morning.
Sometimes, these chills and other flu-like symptoms are what spur a person with IBD to see a doctor in the first place. If a persons gastrointestinal symptoms are not particularly severe, fever and chills might be the first indication that something is wrong. As one member commented, Fevers and chills were part of what led to my Crohns diagnosis.
These symptoms may occur during IBD flares in some cases, even without accompanying gastrointestinal symptoms. Fever and chills are part of the symptoms of a Crohns flare-up I had, shared one member. These were the only symptoms for about a week.
However, some people with IBD experience these symptoms on a regular basis. For the past month or so, I have been getting chills while I have a bowel movement, and they are getting worse each day, one member wrote.
Find New Stress Management Techniques
Stress can trigger a colitis flare-up, so practice stress management techniques to reduce as much external stress on your body as possible.
Why does stress affect irritable bowel diseases so easily? Cortisol can increase inflammation in your body, and learning to manage stress can help you reduce that inflammatory response.
Reduce your stress levels through:
- Practicing deep breathing
- Prioritizing self-care
Self-care includes getting enough sleep each night, following a well-balanced diet, and setting aside time for your favorite activities each day.
Also Check: Whipworm Therapy For Ulcerative Colitis
Youre Not Avoiding Trigger Foods
Theres no food or food group that causes or cures ulcerative colitis, Yun explains. But many people with UC say that certain foods either bring on symptoms or make them worse.
During a flare-up, your doctor may recommend adjustments to your diet. This can mean avoiding foods that trigger symptoms, such as bloating, diarrhea, and cramping. For example, dairy products can be particularly irritating for people who have both UC and lactose intolerance.
Aside from dairy, common trigger foods include beans, whole grains, nuts, seeds, some raw fruits and vegetables, high-fat foods, sugary foods, and sugar alcohols . If youre trying an elimination diet to determine which foods you need to avoid, keep a food diary, and always work with a healthcare practitioner to ensure youre getting all the nutrients you need.
Anxiety And Control Over Activities
Participants acknowledged a large amount of anxiety resulting from a pattern of their symptoms controlling their lives and the resulting effects of their disease on their quality of life.
Ive got a full-blown flareup, and uh, I try and schedule things around when Ive got to go to the bathroom in a half hour, so lets not start this meeting or lets get this meeting over, um, excuse me, Ive gotta go.
if I dont go in the morning, then its in the back of my head, Ok, whens it going to hit? But if I go in the morning, right after I get up, I have no worries the rest of the day.
You end up planning your whole life around what your gut is doing.
I mean, you plan your life around it .
When it started, I just had to stay home because so often I couldnt handle it and it had absolutely no control, and when you teach, you cannot have that in the classroom.
Recommended Reading: Could I Have A Stomach Ulcer
Avoiding Stress Can Ease Flare
Although stress does not cause ulcerative colitis, it will stimulate your symptoms to be worse and trigger your ulcerative colitis flare-up. You must perform exercises, since they assist scale back tension, make sure the bowels square measure operating commonly and relieve you from depression. No matter the exercise being gentle, it will build an enormous distinction. However, you must specialize in activities that you just like doing. Such activities include bike riding, yoga, walking and swimming, as they are smart exercise activities. So as to work out the correct activity for you, it is judicious to consult your doctor.
How Long Do Ulcerative Colitis Flare
People with ulcerative colitis , a type of inflammatory bowel disease that causes inflammation and sores in the rectum and colon, experience bouts of symptoms or flare-ups, which are unpredictable and can last for days, weeks or even months. Having a treatment plan in place including medication, diet changes and flare-up reduction methods could help shorten a flare.
Don’t Miss: What Causes Stomach Ulcers In Humans
Your Uc Flare Management Plan
Your doctor may help you deal with a flare by changing your medications or offering new ones. Treatment of flares can include mesalamine products and usually a steroid, such as prednisone,” says Desi.
There are also some things you can do at home to temper a flare. These include:
During an ulcerative colitis flare, its recommended that you schedule regular visits to see your doctor, at least once every three months until the symptoms go away. After the flare has subsided, physicians recommend one or two checkups a year to manage the disease.
When an ulcerative colitis flare strikes, you have options for getting your life back on track. Its important to learn what you can about maintaining your health and work with your doctor to find the best ways to safely control UC. And remember to always let your doctor know when new or persistent symptoms arise.
Get Support For Your Ibd Today

MyCrohnsAndColitisTeam is the social network for people diagnosed with IBD and the people who love, support, and care for them. More than 142,000 members come together to ask questions, give advice, and share their experiences of life with IBD.
Have you experienced chills with Crohns disease or ulcerative colitis? Share your experience in the comments below or by posting on MyCrohnsAndColitisTeam.
Recommended Reading: What Is An Infusion For Ulcerative Colitis
What Can Affect Ulcerative Colitis Flare
The concrete reasons causing the UC flare-up are still unknown. For some people, the effects might be visible in only a small section, but for a few, it might spread through the entire colon. However, certain factors that might trigger the flare-ups are:
- Smoking Cigarettes are not only one of the major factors that cause UC, but also can cause flare-ups.
- Food that irritates the GI tract There is evidence that food can cause UC or flare. Consuming certain foods during a flare-up can aggravate the symptoms.
- Unnecessary Medication Flare-up can be a result of intake of unprescribed over-the-counter drugs. Nonsteroidal anti-inflammatory drugs like Aspirin, Naproxen, Ibuprofen, and others can worsen the flare-up symptoms.
- Stress Emotional or physical stress doesnt cause ulcerative colitis directly, but it does affect the digestive process and hence contributes to the worsening of flare-ups.
Read Also: What Should You Eat With Ulcerative Colitis
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
Recommended Reading: What Are Signs Of A Peptic Ulcer
What Should I Ask My Doctor On Behalf Of My Child Or Teenager
Ask your healthcare provider the following questions in addition to the ones listed above:
- What vitamins should my child take?
- Will my other children have pediatric ulcerative colitis?
- Is my child at risk for other conditions?
- Can you recommend a psychiatrist or therapist to help my child with emotional issues related to pediatric ulcerative colitis?
- Is my child growing at a normal rate?
- What can I do to help my child cope at school?
A note from Cleveland Clinic
When you have ulcerative colitis, its essential to work closely with your healthcare team.
Take your medications as prescribed, even when you dont have symptoms. Skipping medications youre supposed to take can lead to flareups and make the disease harder to control. Your best shot at managing ulcerative colitis is to follow your treatment plan and talk to your healthcare provider regularly.
Read Also: How To Heal Ulcerative Colitis With Food
Get Enough Relaxation And Rest To Ease Flare
In order to ease and combat ulcerative colitis flare-up, ensure you get enough time to relax as it is vital. Relaxation ensures your body is calm and digestion of food is much easier. In addition, you can take breathing and stretching practices, in order to improve your blood circulation, to keep your body out of flight mode and to make sure you regulate your digestive system.
You May Like: What To Eat With An Ulcerative Colitis Flare Up
What Are Ulcerative Colitis Flare
Ulcerative colitis is a condition which affects thousands of people across the UK. Luckily, many people with ulcerative colitis flare-ups receive advice and treatment, meaning the condition has minimal impact on their quality of life.
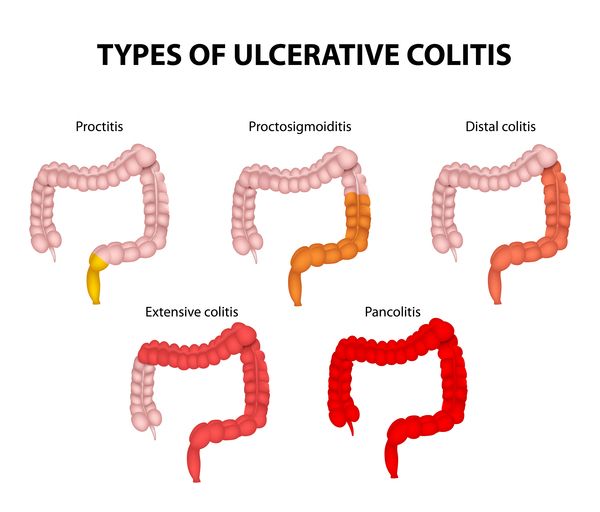
This doesnt mean flare-ups are completely avoidable though. Depending on whether you have proctitis, distal or total colitis, a flare-up may have different effects on the individual. Knowing how to recognise and manage these effects is very important.
In this short blog post, we will discuss what happens during a flare-up and how best to alleviate problems when it does.
Donât Miss: Is Soy Milk Good For Ulcerative Colitis
Ulcerative Colitis Questions To Ask Your Doctor
Whether youâre worried your symptoms are UC, or you already have the condition and want more information, here are questions to ask your doctor:
- Are my symptoms a sign of ulcerative colitis or another condition?
- Are there different kinds of UC? Do they have different symptoms?
- What tests will I need?
- If I have ulcerative colitis, what will my treatment plan be?
- Will changing my diet or lifestyle help ease my symptoms?
- How serious is my ulcerative colitis?
- If I take medication for ulcerative colitis, will there be side effects?
- Should I take nutritional supplements like probiotics?
- How often will I need to come in for checkups?
- What should I do if my symptoms suddenly get worse?
- How do I know if my ulcerative colitis is getting worse?
- How do I know if I should change my ulcerative colitis medication?
- Should I consider surgery? What does surgery involve?
- What is my risk of getting colon cancer?
Recommended Reading: What Should You Not Eat If You Have An Ulcer
Recommended Reading: Off Loading Shoe For Heel Ulcer
Medications For Other Conditions
A medication you take for another condition can also trigger a flare-up.
This might happen if you take an antibiotic to treat a bacterial infection. Antibiotics can sometimes disrupt the balance of intestinal bacteria in the gut and cause diarrhea.
Certain over-the-counter nonsteroidal anti-inflammatory drugs , such as aspirin and ibuprofen , may also irritate the colon and cause a flare-up.
This doesnt mean you should stop taking antibiotics or pain medications, but you should speak with your doctor before taking these drugs.
If you take an antibiotic, you may also need a temporary antidiarrheal medication to combat possible side effects.
If you experience stomach pain after taking an NSAID, your doctor may suggest acetaminophen to reduce pain instead.
What Else Should I Know
People with ulcerative colitis are at risk for colon cancer, which is related to chronic inflammation. So they should get a colonoscopy every 1-2 years, starting about 10 years after diagnosis.
Kids and teens with ulcerative colitis may feel different and not be able to do the things their friends can do, especially during flare-ups. Some struggle with a poor self-image, depression, or anxiety. They may not take their medicine or follow their diet. It’s important to talk to the doctor or a mental health provider if you’re concerned about your child’s mood, behavior, or school performance.
Parents can help teens take on more responsibility for their health as they get older. Encourage teens to take their medicine, take care of themselves, and manage stress in positive ways. Yoga, meditation, breathing and relaxation techniques, music, art, dance, writing, or talking to a friend can help.
You also can find more information and support online at:
Don’t Miss: Is Ashwagandha Safe For Ulcerative Colitis
General Causes Of Ulcerative Colitis
The exact cause for ulcerative colitis continues to be not acknowledged. However, researchers link the sickness to:
- A combination of environmental factors.
- A system that is awry.
- Genetic predisposition.
- A microorganism or microorganism infection within the colon, that initiates uncontrolled inflammation that is closely joined to colitis.
The condition may additionally be aggravated by the sort of diet and stress. For example consumption of Trans fats in masses will increase the danger of the condition. These fats square measure chiefly in processed foods. On the opposite hand, the intake of Omega -3 fatty acids in massive quantities lowers the danger of developing the condition.