Ulcerative Colitis In Children
According to one study of IBD in the United States, 1 in 1,299 children between ages 2 and 17 years old were affected by the condition in 2016. Crohns disease was twice as common as UC, and boys were more likely to have IBD than girls.
For children with IBD, a diagnosis is more likely after 10 years old.
UC symptoms in children are similar to symptoms in older individuals. Children may experience bloody diarrhea, abdominal pain and cramping, and fatigue.
In addition, they may experience issues compounded by the condition, such as:
- anemia due to blood loss
- malnutrition from poor eating
- unexplained weight loss
UC can have a significant effect on a childs life, especially if the condition isnt treated and managed properly. Treatments for children are more limited because of possible complications. For example, medicated enemas are rarely used as a treatment method in children.
However, children with UC may be prescribed medications that reduce inflammation and prevent immune system attacks on the colon. For some children, surgery may be necessary to manage symptoms.
If your child has been diagnosed with UC, its important that you work closely with their doctor to find treatments and lifestyle changes that can help. Check out these tips for parents and children dealing with UC.
Ileal Pouch For Ulcerative Colitis
There is one surgical technique that can cure ulcerative colitis without the need for a colostomy or ileostomy bag.
The ileal pouch technique is a surgical procedure which removes the entire colon, from the point of its attachment at the small intestine to the point of its attachment at the anus. The anal sphincter muscles and the anus are left intact. The last 10 inches of the small intestine are then used to make a U-shaped sac which is attached to the anus at the anal opening.
This pouch acts as a new rectum. The anal sphincter is left in place so that the patient can still control their bowel movements. Patients generally moves their bowels 4 to 8 times per day following this operation. However, the patient has reasonably good control, and no longer has any symptoms of the colitis.
The ileal pouch procedure requires two operations. During the first operation, the surgeon removes the entire colon, creates the pouch and hooks it to the anus. The surgeon makes an ileostomy, which means that the patient must temporarily wear a bag on the abdomen to collect stool. This prevents bowel contents from entering the pouch until it is healed. After about three months, the surgeon removes the ileostomy. The pouch then begins to function as a rectum, and the patient no longer needs the ileostomy bag.
Reducing The Risk Of Cancer
People with UC are at greater risk of developing colorectal cancer, so it is important to take steps to manage this risk.
People with UC should see their doctor at least once per year for annual checkups and scans. At these appointments, they can discuss their condition and overall state of health.
Doctors may be able to help manage the risk of colorectal cancer in people with UC.
Also Check: Can You Eat Pizza With Ulcerative Colitis
Diet Progression Following Flares For Ulcerative Colitis And Crohns Disease
- Continue to follow a low residue diet and slowly add back a variety of foods.
- Begin with well-tolerated liquids and advance to soft solids, then solids .
- Introduce one or two items every few days and avoid any foods that cause symptoms.
- Add fiber to diet as tolerated. Well-tolerated fiber sources include tender cooked vegetables, canned or cooked fruits, and starches like cooked cereals and whole wheat noodles and tortillas.
- Between flares, eat a wide variety of foods as tolerated. This includes fruits, vegetables, whole grains, lean protein, and low-fat and nonfat dairy products.
- Increase your calorie and protein intake following a flare. Abdominal pain, diarrhea and decreased appetite may have caused poor food intake. Steroids used to treat flares also can increase protein needs.
Suggestions for first foods after a flare include:
- Diluted juices
Soothe The Stomach With Bananas
Bananas can help heal a stomach ulcer by promoting cellular proliferation in the stomach. In addition to this, there are certain antibacterial compounds in bananas that inhibit the growth of ulcer-causing H. pylori. Bananas also help reduce inflammation and strengthen the stomach lining.
A 1986 study published in the Journal of Ethnopharmacology suggests that banana powder treatment not only strengthens mucosal resistance against ulcerogens but also promotes healing by inducing cellular proliferation.
A 2001 study published in the Indian Journal of Experimental Biology suggests that the antioxidant activity of bananas may be involved in its ulcer-protective activity.
In a 2013 study published in Pharmacognosy Research, researchers suggest that the anti-ulcer effect of banana may be due to its antisecretory and cytoprotective activity. The healing of the ulcer base might be connected to the basic fibroblast growth factors responsible for epithelial regeneration in the case of acid-induced ulcers.
Both ripe and unripe bananas are very effective in treating a stomach ulcer.
- Simply eat at least 3 ripe bananas a day.
- Alternatively, peel 2 or 3 bananas and cut them into thin slices. Put the banana slices in the sun until they dry. Now, grind the dry pieces into a fine powder. Mix together 2 tablespoons of this powder and 1 tablespoon of honey. Take this mixture 3 times a day for 1 week.
Read Also: How To Prevent Sacral Pressure Ulcers
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
Have Just Had A Colonoscopy And They Found Some Aphthous Ulcers In My Bowel What Are They
Ask U.S. doctors your own question and get educational, text answers â it’s anonymous and free!
Ask U.S. doctors your own question and get educational, text answers â it’s anonymous and free!
HealthTap doctors are based in the U.S., board certified, and available by text or video.
You May Like: Can Ulcers Give You Headaches
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.
What Are Rectal Ulcers
A rectal ulcer is a painful sore that develops inside the rectum. The rectum is a tube connecting the colon to the anal opening . Stool passes through the rectum and anus when it leaves the body.
These ulcers are related to several different conditions. People who have a condition called solitary rectal ulcer syndrome can develop rectal ulcers. Inflammatory bowel disease , including ulcerative colitis and Crohns disease, may also cause ulcers to form in the rectum and intestines. Constipation and straining during a bowel movement can cause rectal ulcers to develop as well.
Signs of a rectal ulcer may include:
- Blood in the stool.
- Painful Bowel movements.
Also Check: Do Ulcers Make You Vomit
How Are Rectal Ulcers Diagnosed
Your doctor will examine you and ask about habits that may have caused your symptoms . To check for rectal ulcers, doctors use physical examination, tests and imaging studies. These tests include:
- Anoscopy: Your doctor may use a tool called an anoscope to examine you. An anoscope is a short tube that your doctor inserts into your anus. Your doctor uses a light to see through the tube and check for ulcers or lesions inside your rectum.
- Sigmoidoscopy: Doctors insert a flexible instrument into your rectum during a sigmoidoscopy. The thin device has a camera on the end. With it, your doctor can see inside your rectum and the lower part of the colon.
- Colonoscopy: To look at the entire colon, doctors insert a long scope with a camera. Like a sigmoidoscopy, a colonoscopy is an outpatient procedure . It is a more invasive test than a sigmoidoscopy.
- Rectal ultrasound: During this test, doctors insert a small probe in your rectum. The probe uses sound waves to show images of the inside of the rectum so your doctor can see ulcers and other growths.
- Biopsy: Your doctor may take a biopsy of the tissue surrounding the ulcer and send it to a lab. The lab tests the tissue for other conditions, such as cancer.
How To Reduce Your Risk
Here are a few other things you can do to lower your chances of developing colorectal cancer and improve your odds of finding it early if you develop it:
- Ask your doctor about taking medications such as sulfasalazine , vedolizumab , or mesalamine . These drugs help manage UC, and they may help lower your risk for colorectal cancer.
- Take your medications as your doctor prescribed to keep your UC inflammation well managed.
- See your gastroenterologist for check-ups at least once a year.
- Let your doctor know if any of your family members had colorectal cancer or have recently been diagnosed.
- Eat more fruits, vegetables, and whole grains such as brown rice or wheat bread.
- Limit red meat, such as burgers, steaks, and pork. Also limit processed meats, such as hot dogs, bacon, and sausage. Theyve been linked to colorectal cancer risk.
- Avoid alcohol or limit yourself to no more than one drink a day.
- Try to walk, ride a bike, or do other exercises on most days of the week.
Along with getting regular screenings, look for these symptoms of colorectal cancer and report them to your doctor right away:
- a change in your bowel movements
- blood in your stool
Recommended Reading: Imodium Ulcerative Colitis Toxic Megacolon
Living With Ulcerative Colitis
With careful management, most people with UC are able to enjoy life, including work, travel, recreation, sex and having children.
To keep healthy, consider:
- eating a nutritious diet to help with healing and reduce fatigue
- keeping a food diary to check if there are any foods that make your symptoms worse during a flare-up
- asking your doctor about supplements if you think you may be malnourished
- exercising regularly to lift your mood and help relieve stress
- learning some relaxation techniques to help manage stress
What Are The Signs And Symptoms Of Colorectal Cancer
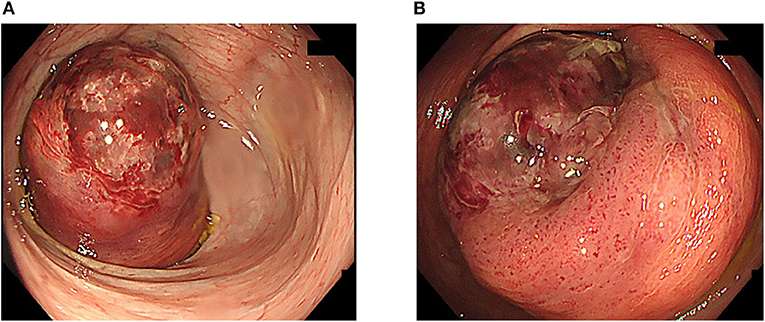
Unfortunately, some colorectal cancers might be present without any signs or symptoms. For this reason, it is very important to have regular colorectal screenings to detect problems early. The best screening evaluation is a colonoscopy. Other screening options include fecal occult blood tests, fecal DNA tests, flexible sigmoidoscopy, barium enema, and CT colonography . The age at which such screening tests begin depends upon your risk factors, especially a family history of colon and rectal cancers.
Even if you do not have a family history of colorectal cancer or polyps, tell your doctor if you have any of the signs that could indicate a colorectal cancer, no matter what your age. Common signs of colorectal cancer include the following:
If you experience any of these signs or symptoms, it is important to see your doctor for evaluation. For a patient with colorectal cancer, early diagnosis and treatment can be life-saving.
You May Like: How To Stop Ulcers From Hurting
Talk With Others Who Understand
MyCrohnsAndColitisTeam is the social network for people with Crohns disease and ulcerative colitis and their loved ones. On MyCrohnsAndColitisTeam, more than 159,000 members come together to ask questions, give advice, and share their stories with others who understand life with Crohns disease and ulcerative colitis.
Have you had a colonoscopy for ulcerative colitis? Share your experience in the comments below, or start a conversation by posting on MyCrohnsAndColitisTeam.
What Will You Learn
Much is written about “the prep” for colonoscopy and the procedure itself, but less is written about what the results may mean. As a screening test, it’s usually done to find colon cancer or precancerous polyps. But, often neither is found instead, other, potentially confusing or surprising findings may be discovered.
Here’s a primer on what your colonoscopy may reveal:
While small polyps can often be removed during colonoscopy, larger ones may require surgery. Risk factors for colon polyps are similar to those for colon cancer, including advanced age, family history of polyps or cancer, a diet high in red meat, or a history of inflammatory bowel disease.
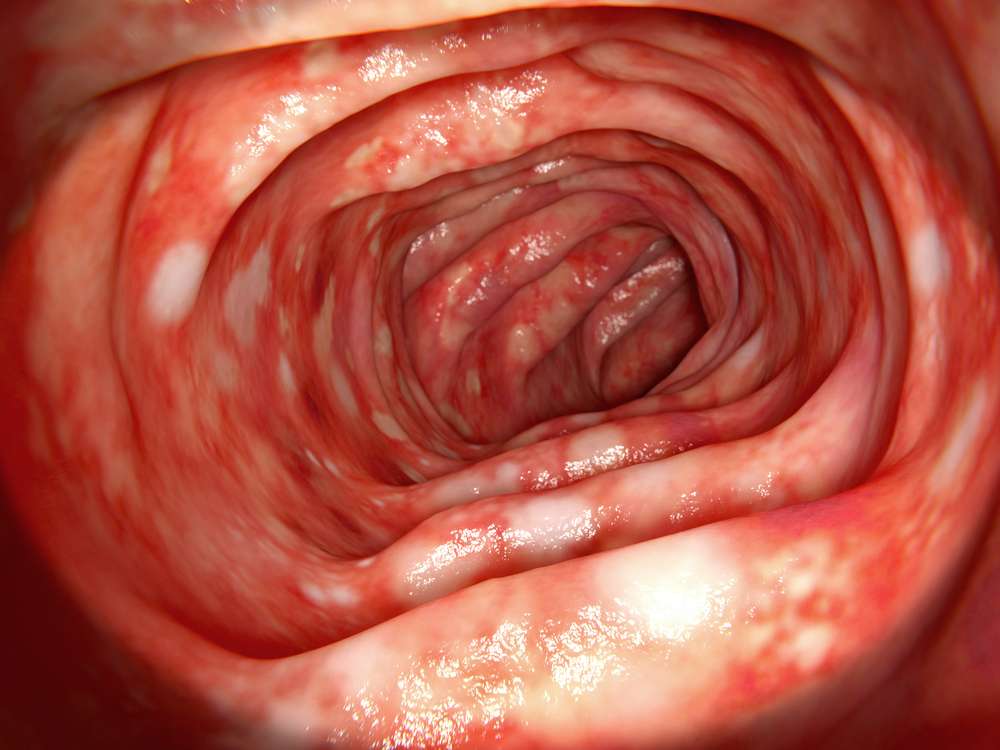
- Inflammation and ulceration The lining of the colon can be irritated, inflamed and ulcerated for many reasons, including infection, medications , inflammatory bowel disease and cancer.
- Bleeding Sometimes there is blood in seen in the colon a search for source may identify a tumor, an ulcer or an abnormal collection of blood vessels but often a source cannot be identified during a colonoscopy and additional tests may be necessary.
Other, less common findings include a “foreign body” or a fistula .
Read Also: Ulcerative Colitis And Hip Pain
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
Why Do You Need A Colonoscopy For Ulcerative Colitis
In addition to its routine use to screen for colon cancer, colonoscopy is an important part of diagnosing and treating ulcerative colitis and other inflammatory bowel disease . UC can occur in any part of the colon , from the rectum to the end of the small intestine. It cannot be properly diagnosed or monitored without tissue biopsies or visualization of the colon.
A colonoscopy provides your doctor with information they need to manage your chronic disease. Colonoscopy is used to determine the extent and severity of UC or to help rule out other conditions that have the same symptoms. Additional colonoscopies may also be needed to monitor how well your UC treatments are working. Because people with IBD have a higher risk of colorectal cancer, regular colonoscopies are also needed for colorectal cancer screening.
| Read: The importance of colonoscopies in measuring UC treatment effectiveness |
Read Also: Offloading The Diabetic Foot For Ulcer Prevention And Healing
Does Ulcerative Colitis Affect Your Cancer Risk
Having ulcerative colitis doesnt mean you will get colorectal cancer, but it does increase your risk.
Ulcerative colitis is a chronic inflammatory bowel disease that affects the lining of the rectum and colon. It can be limited to the rectum or extend throughout the colon. Ulcerative colitis that affects the entire colon is called pancolitis.
The most common symptoms of ulcerative colitis are diarrhea and blood in your stool. Some patients may have abdominal pain. In severe cases, it can cause fever. Experts arent sure what causes the disease.
We talked to Yinghong Wang, M.D., about the link between ulcerative colitis, cancer and cancer treatment.
How does ulcerative colitis affect cancer risk?
If you have ulcerative colitis, your immune system recognizes the lining of your colon as a foreign body and attacks it. Over time, this damages the colon. As your body tries to repair the damage, the inflammation and constant cell replacement can result in a mutation that leads to cancer.
The more extensive your colitis and the longer you have it, the greater your risk of colorectal cancer. Males are at higher risk. And if you have both primary sclerosing cholangitis, which is inflammation of the bile duct, that puts you at even greater risk for colorectal cancer.
What should I do to reduce my cancer risk if I have ulcerative colitis?
Surgery is a cure. Because your colon is gone, the disease is gone, too.
What should cancer patients with ulcerative colitis know?