What Are The Symptoms Of Leg Ulcers
A lower leg wound that doesnt heal with treatment after two weeks is the first indication of a leg ulcer. The sore may be red, purple, brown or yellow . Nonhealing sores on your legs often have a liquid discharge.
Other signs of a leg ulcer include:
- Dry, scaly or itchy skin.
- Hard bumps on the skin or hardened skin.
- Leg pain, especially after standing for a while.
- Red, blue or purplish skin color .
- Swelling in the lower legs.
How To Prevent Diabetic Sores On Leg
Its critical to keep an eye on your skin if you have diabetes. If you have neuropathy, sores may go unnoticed. When you acquire blisters or get infections in the wounds, there are things you can do to avoid them:
- Each day, carefully inspect your feet.
- Wearing shoes and socks will help you avoid hurting your feet.
- Wear shoes that arent too constricting.
- Take it easy, when trying new shoes as it may cause diabetic sores.
- Wear gloves when pruning or using gardening equipment that might result in blisters.
- Some individuals are sensitive to ultraviolet light, which causes blisters. Apply sunscreen and avoid going outside as much as possible.
How To Treat Leg Ulcers
Treatments for leg ulcers will include wound care, relieving the pressure in your legs, and getting your blood sugar under control. Your healthcare provider will also consider the cause of your leg ulcer before deciding which treatment is best.
Treatments for leg ulcers include the following:
Pressure relief: Wearing compression stockings will help prevent blood from pooling in your legs, lower inflammation, and promote healing. Wear shoes that fit properly and are made of material that allows your feet to breathe .
Wound care: Your healthcare provider will provide instructions for how to care for the ulcer. It should include keeping it clean, moisturized, bandaged, and dry. Your healthcare provider may also prescribe a treatment called debridement, which the removal of dead skin by a podiatrist .
Control blood sugar: High blood sugar causes blood vessel damage. Keeping your blood sugar within the healthy range your healthcare provider has established in your diabetes management plan is essential.
Surgery: If pressure and wound care dont help, you may need surgery or a skin graft to close up the wound.
Surgical correction of venous insufficiency: If venous insufficiency is the cause of the ulceration, correction may accelerate healing.
Also Check: Icd 10 Code For Ulcerative Colitis With Bleeding
Open Sores And Wounds
Having high blood sugar for a long time can lead to poor circulation and nerve damage. You may have developed these if youve had uncontrolled diabetes for a long time.
Poor circulation and nerve damage can make it hard for your body to heal wounds. This is especially true on the feet. These open wounds are called diabetic ulcers.
Diabetes and feet
- Get immediate medical care for an open sore or wound.
- Work with your doctor to better control your diabetes.
What Are Neurotrophic Ulcers
Neurotrophic ulcers occur primarily in people with diabetes, although they can affect anyone who has impaired sensation in their feet. They can be found anywhere on your feet, but they usually develop on the parts of your feet and toes that are most sensitive to weight .
Neurotrophic ulcers dont cause pain. But they can be serious if they arent treated promptly or they dont respond to treatment.
A neurotrophic ulcer might be the following colors:
- Any combination of those colors.
The thin borders of the ulcers are punched out, meaning that theyre taller than the surrounding tissues.
Also Check: What Foods Cause Stomach Ulcers
Where Does An Ulcer Appear
There are many different kinds of ulcers. While peptic ulcers form in the stomach or upper intestine lining, ulcers can also occur almost anywhere on the body.
Ulcers that are found outside the body can include leg and foot ulcers. These ulcers are generally swollen or tender and can cause itchiness or pain. Skin discoloration and changes in texture are also common in ulcers found outside the body.
Whether they are found inside or on the skin’s surface, ulcers are sores that are often slow to heal. Once they have disappeared, ulcers can return if not treated properly. Depending on the cause of the ulcers, they can require different treatment options.
Other Types Of Leg Ulcer
Other common types of leg ulcer include:
- arterial leg ulcers caused by poor blood circulation in the arteries
- diabetic leg ulcers caused by the high blood sugar associated with diabetes
- vasculitic leg ulcers associated with chronic inflammatory disorders such as rheumatoid arthritis and lupus
- traumatic leg ulcers caused by injury to the leg
- malignant leg ulcers caused by a tumour of the skin of the leg
Most ulcers caused by artery disease or diabetes occur on the foot rather than the leg.
Page last reviewed: 16 November 2022 Next review due: 16 November 2025
Don’t Miss: Photos Of Venous Leg Ulcers
How Does This Insight About The Skin
As physicians who treat chronic wounds, we generally don’t assess the mental status of our patients. We often just focus on healing the wound. We can be more aware of the patients mental health and recommend intervention if they show depression or cognitive disability.
Ideally, we should have mental health specialists in our clinics to address the mental health needs of patients. Patients need additional education on how their mental health can affect their healing, and conversely, how the non-healing wound may be affecting their mental health. These interventions could help the overall healing process and result in better outcomes for our patients with chronic wounds.
To learn more about Isseroffs study on skin-brain connection, read her article in Brain, Behavior, and Immunity- Health.
Nonsurgical Treatment For Diabetic Foot Ulcers
To help a diabetic foot ulcer heal, doctors at NYU Langone clean and disinfect the area. If the ulcer is infected, your doctor prescribes antibiotics to clear it up and prevent it from traveling to a bone in the foot.
Your doctor can refer you to an NYU Langone vascular specialist for additional medication if you have lower extremity arterial disease, a condition that impairs blood flow to the legs and feet and can cause an ulcer to heal more slowly.
NYU Langone doctors recommend regular wound care for foot ulcers, as well as other therapies.
You May Like: Can You Have Colitis Without Ulcers
What Are The Risk Factors For Diabetes Foot Ulcers
The following can increase the likelihood of developing a foot ulcer:
- Wearing poor fitting footwear
- Walking barefoot
People who have diabetes for a longer period or manage their diabetes less effectively are more likely to develop foot ulcers. Smoking, not taking exercise, being overweight, having high cholesterol or blood pressure can all increase diabetes foot ulcer risk.
Heart And Blood Circulation Problems
Cardiovascular autonomic neuropathy is a potentially serious heart and blood circulation problem that’s common in people with diabetic polyneuropathy.
CAN happens when damage to the peripheral nerves disrupts the automatic functions that control your blood circulation and heartbeat.
The 2 main noticeable symptoms of CAN are:
- an inability to exercise for more than a very short period of time
- low blood pressure that can make you feel dizzy or faint when you stand up
Recommended Reading: Can Stomach Ulcers Cause Headaches And Dizziness
Yellowish Scaly Patches On And Around Your Eyelids
These develop when you have high fat levels in your blood. It can also be a sign that your diabetes is poorly controlled.The medical name for this condition is xanthelasma.
Take action
- Tell your doctor about the yellowish scaly patches around your eyes.
- Talk with your doctor about how to better control your diabetes. Controlling diabetes can clear the scaly patches.
Causes Of Diabetic Foot Ulcers

An ulcer is an open sore or wound on the skin. Ulcers on the feet are particularly common in those who have diabetes. Complications from the disease such as poor circulation and loss of feeling in the feet due to diabetes-related nerve damage make it more likely for a wound to develop, and also harder to heal.
People with diabetes who use insulin, have diabetes-related kidney, eye or heart disease, or who are overweight, use alcohol or tobacco have an even higher risk of developing foot ulcers.
You May Like: Is Honey Good For Ulcerative Colitis
Tips To Prevent Ulcers
Thereâs a lot you can do to lower your chance of having ulcers in the first place:
Keep your blood sugar in check. Good blood sugar control is the single best way to prevent small cuts and sores from becoming ulcers. If you have trouble managing your blood sugar, tell your doctor. They can work with you to make changes to your medication and lifestyle that will keep your blood sugar from getting too high. Even if your blood sugar level is fairly steady, itâs still important to see your doctor regularly. Thatâs especially key if you have neuropathy, because you may not feel damage to your skin and tissue.
Check your skin every day, and pay special attention to your feet. Look for blisters, cuts, cracks, sores, redness, white spots or areas, thick , discoloration, or other changes. Donât rely on pain even feeling more warmth or cold than usual can be a sign that you have an open wound on your skin, and itâs possible that you may feel nothing at all.
Ulcers are most likely to form on the ball of your foot or the bottom of your big toe, so be sure to check your feet every night. If you notice a problem, or you arenât sure if somethingâs normal, call your doctor.
Donât smoke.Smoking damages your blood vessels, decreases blood flow, and slows healing. Those things raise your risk of ulcers and amputation.
Show Sources
How Do I Take Care Of My Foot And Toe Ulcers
Your healthcare provider might teach you how to care for your ulcers at home. You might be instructed to:
- Wash the affected area with mild soap.
- Keep the wound clean and dry.
- Change the bandages as directed.
- Take prescribed medications as directed.
- Drink plenty of fluids. Ask your healthcare provider how much water you should drink every day.
- Follow a healthy diet, as recommended by your healthcare provider.
- Exercise regularly, under your healthcare providers care.
- Wear appropriate shoes.
- Wear compression wraps as directed.
Read Also: How To Treat Venous Stasis Ulcers
What Are Diabetic Ulcers
Ulcers are wounds that heal slowly. Slow healing injuries are prevalent in those with diabetes. The condition decreases the bodys resistance to infection and trauma and compromises its ability to heal or recover. Without proper care, diabetic ulcers can turn into festers and weep or ooze liquid, blood, or pus.
Symptoms of diabetic ulcers include:
- Pain in the legs or feet that occurs with or without cause or movement
- Slow healing or non-healing injuries or sores
- Cracked, peeling, or inflamed skin
- Discolored skin that may seem tender to the touch
- Bleeding, burning, or irritation to the skin, especially on the feet, ankles, or bottom of the feet
- A bluish tint to the toenails or the skin on the legs or feet
- Leg hair that no longer grows
Advanced stage diabetic ulcers can lead to gangrene, a condition that destroys skin and tissue, omits an unpleasant smell, causes prominent skin discoloration, and requires antibiotics and surgery to remove the affected limb to prevent the infection from spreading.
As foot and leg injuries and deformities become more likely with age, many ulcers develop from a combination of issues, not just elevated blood sugar. Also, when blood sugar levels remain unchecked, the risk of diabetic ulcers increases significantly.
What Are Foot And Toe Ulcers
An ulcer is an open wound or sore that will not heal or keeps returning. When you have ulcers on your feet and toes, it can be related to diabetes specifically, a complication called neuropathy that causes you to lose feeling in your feet. A scrape, cut or puncture in your skin can turn into an ulcer, but you might not know its there if you have neuropathy.
Ulcers can lead to infections. Sometimes, the infection wont go away and you may need to have part of your foot or toe surgically removed . About 15% of people with diabetes will get a foot or toe ulcer. Around 14% to 24% of people with diabetes in the U.S. need an amputation after they get an ulcer.
You May Like: Best Food For Ulcer Pain
How Can I Prevent Leg Ulcers
Leg ulcers commonly open up again after healing. These steps can lower the risk of getting a leg ulcer or a wound recurrence:
- Elevate your legs above your heart when youre sitting or sleeping.
- Maintain a healthy weight and stay physically active.
- Manage health conditions that affect blood circulation, including diabetes, high blood pressure, high cholesterol and Raynauds syndrome.
- Quit smoking and using tobacco products. Talk with your healthcare provider about ways to stop smoking.
- Use gentle cleansers, and apply moisturizing lotion to prevent dry skin.
- Wear compression stockings or bandages for an hour each day to improve blood flow to the legs.
Does Gabapentin Cause Weight Gain Learn More About The Side Effects
Gabapentin is a prescription drug that is used to treat various medical conditions such as seizures, restless legs syndrome, and nerve pain and it belongs to a class of anticonvulsant medication. Gabapentin works by decreasing the number of seizures you have, relieving pain, and improving your sleep among several other benefits. If you take gabapentin you also may experience weight gain as a side effect. In this article, we will discuss how gabapentin causes weight gain, how to stop it, and other potential risks associated with taking this medication.
You May Like: Combination Therapy For Ulcerative Colitis
Tip #: Get The Right Nutrients
Eating a well-balanced diet, high in lean protein, fiber and legumes, and low in saturated fats, can be very beneficial for diabetic patients. Many minerals and vitamins, for instance, zinc, iron, copper and protein, are necessary for the body to grow tissue. If youre deficient in those products, you can imagine that healing is going to be a lot slower, she explains.
Assessment Of Diabetic Foot Ulcers

A task force of the Foot Care Interest Group of the American Diabetes Association released a 2008 report that specifies recommended components of foot examinations for patients with diabetes. Providers should take a history that takes into consideration previous ulceration or amputation. The history should also include any neuropathic symptoms or symptoms that are suggestive of peripheral vascular disease. Further, providers should inquire about other complications of diabetes, including vision impairment suggestive of retinopathy and nephropathy, especially dialysis or renal transplantation. Finally, patients should be questioned regarding smoking because smoking is linked to the development of neuropathic and vascular disease. A complete history will aid in assessing the risk for foot ulceration.
In examining the foot, visual inspection of the bare foot should be performed in a well-lit room. The examination should include an assessment of the shoes inappropriate footwear can be a contributing factor to the development of foot ulceration. In the visual inspection of the foot, the evaluator should check between the toes for the presence of ulceration or signs of infection. The presence of callus or nail abnormalities should be noted. Additionally, a temperature difference between feet is suggestive of vascular disease.
Don’t Miss: Paleo Diet For Ulcerative Colitis
Fructosamine To A1c: How Are They Related
Diabetes, also called diabetes mellitus, is a condition that affects millions of people all over the world. It can be difficult to manage, but with the right tools and information, it is possible to live a healthy life with diabetes. One of the most important tools for managing diabetes is understanding fructosamine levels and hemoglobin A1C levels. In this article, we will explain what fructosamine and hemoglobin A1C are, and discuss the relationship between these two measures. We will also provide tips on how to test your fructosamine and hemoglobin A1C levels correctly.
How To Treat And Prevent Diabetic Ulcers On The Feet And Legs
Home – Disease – How to Treat and Prevent Diabetic Ulcers on the Feet and Legs
If you have diabetes, also called diabetes mellitus, it is important to be aware of diabetic ulcers on your feet, ankles, and legs.
These sores can easily become infected if not treated properly and can eventually lead to severe infection and even limb amputation.
In this article, we will discuss what diabetic ulcers are, how to treat them, and how to prevent them from occurring in the first place.
We will also touch on other causes of ulcers for those who do not have diabetes in case diabetes is not the cause of your foot or leg ulcer.
Don’t Miss: Do Ulcers Cause Burning In The Stomach
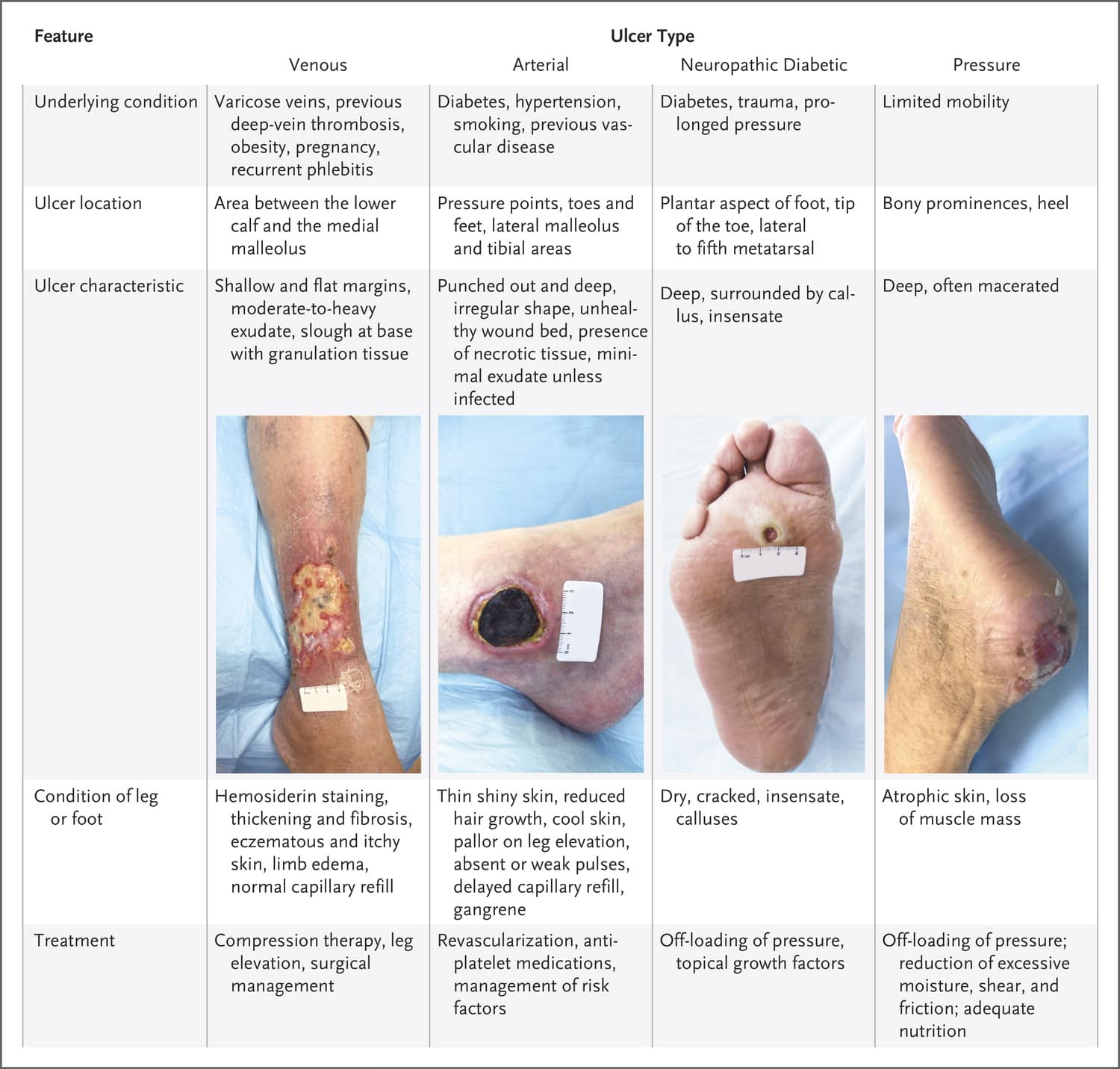
How Are Foot And Toe Ulcers Diagnosed
Your healthcare provider can tell what type of ulcer you have based on four observations:
- The appearance of the ulcer.
- Location of the ulcer.
- The appearance of the borders.
- The appearance of the surrounding skin.
Your primary healthcare provider can diagnose an ulcer, but they might send you to a specialist for treatment. You might see a podiatrist, a provider who works with feet, or a wound specialist. For more complicated cases that require surgery, you might also see a plastic surgeon, anesthesiologist, orthopedic surgeon and/or vascular surgeon.
Diabetic Nerve Pain In Ankle Feet And Legs
Diabetic neuropathy is a condition that results from damage to the nerves due to high blood sugar levels and nerve damage can cause a wide range of symptoms including pain, numbness, tingling, burning sensations, and weakness. In some cases, diabetic neuropathy can lead to serious complications such as diabetic foot ulcers.
Also Check: Liquid Diet For Ulcerative Colitis