How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
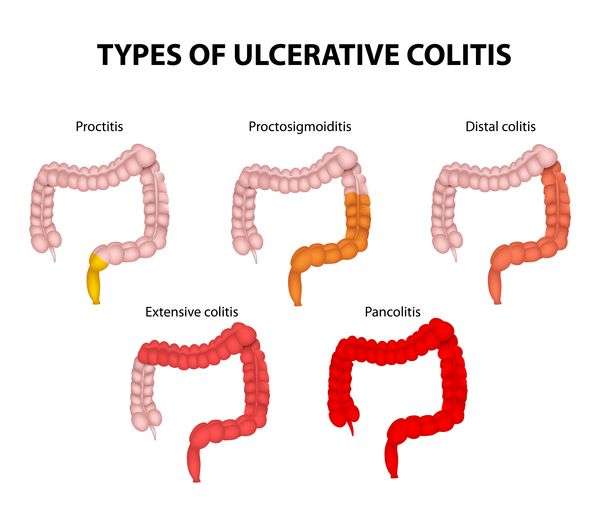
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
Oral Signs Of Crohn Disease
The oral mucosa is commonly affected in Crohn disease with up to one third of patients reported to have oral changes, and even higher in children. In some studies, the oral changes preceded the diagnosis of Crohn disease in 60%. There may be a male predominance.
1. Specific oral mucosal changes: orofacial Crohn disease
In children with Crohn disease, orofacial Crohn disease can be an important presentation preceding the bowel diagnosis.
2. Nonspecific changes in the mouth and surrounding facial skin associated with Crohn disease:
Involvement Of Body Sites Other Than The Bowel In Inflammatory Bowel Disease
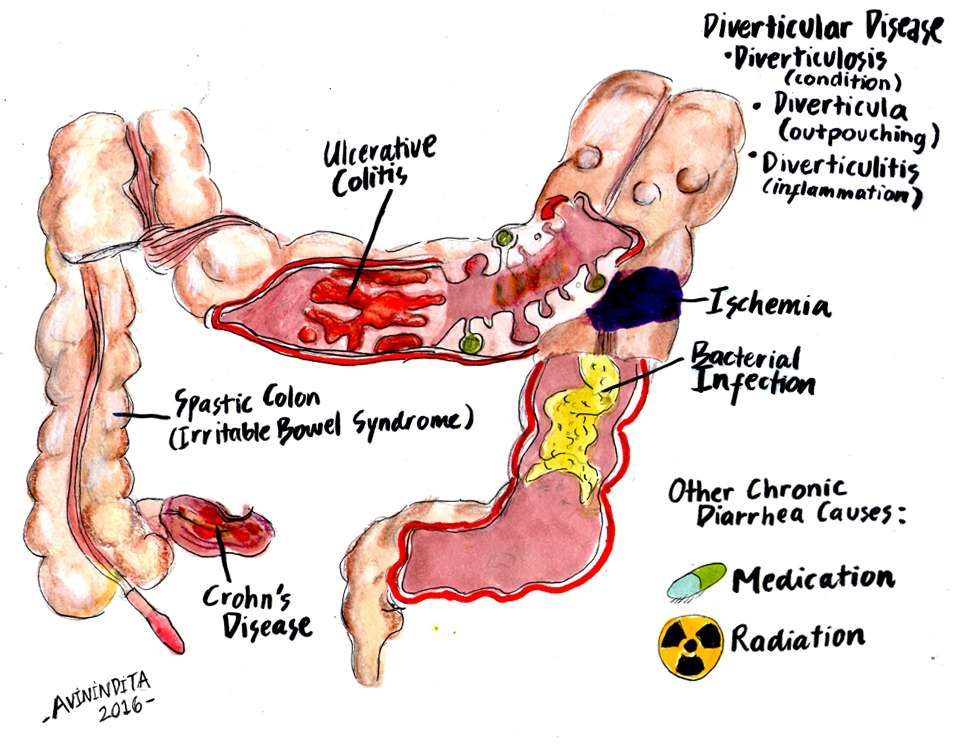
Both forms of inflammatory bowel disease can develop symptoms and signs in addition to the bowel disease. Changes in the skin and oral mucosa can develop with both, but are more commonly seen with Crohn disease. Sometimes these develop before the diagnosis of inflammatory bowel disease, leading the doctor to investigate for bowel problems. In some patients they may appear with flares of the bowel inflammation. Where the association is specific with diagnostic histology, it can be valuable in making the diagnosis.
Don’t Miss: Snack Ideas For Ulcerative Colitis
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.
Difference Between Colitis And Diverticulitis
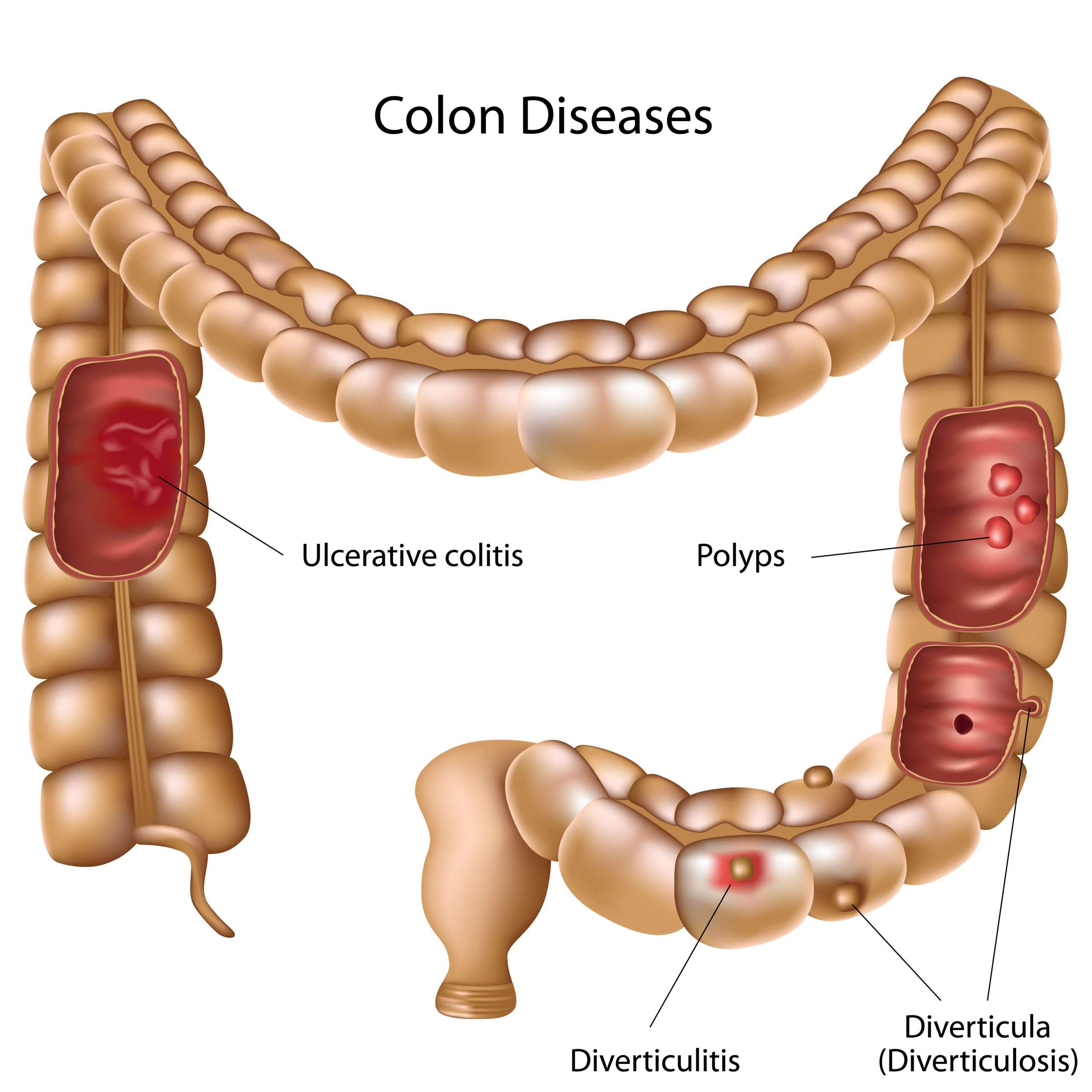
The difference between colitis and diverticulitis can be hard to distinguish as both cause similar abdominal pain. Colitis and diverticulitis are inflammatory diseases that can affect the colon and rectum in our large intestine. Though both the diseases show some similar symptoms, colitis causes inflammation of the colon whereas diverticulitis causes inflammation of the diverticula.
Read Also: Can I Eat Oatmeal With Ulcerative Colitis
How Is Ulcerative Colitis Diagnosed
To diagnose ulcerative colitis in children, teenagers and adults, your healthcare provider has to rule out other illnesses. After a physical exam, your provider may order:
- Blood tests: Your blood can show signs of infection or anemia. Anemia is a low level of iron in your blood. It can mean you have bleeding in the colon or rectum.
- Stool samples: Signs of infection, parasites , and inflammation can show up in your poop.
- Imaging tests: Your healthcare provider may need a picture of your colon and rectum. You may have tests including a magnetic resonance imaging scan or computed tomography scan.
- Endoscopic tests: An endoscope is a thin, flexible tube with a tiny camera. Specialized doctors can slide the endoscope in through the anus to check the health of the rectum and colon. Common endoscopic tests include colonoscopy and sigmoidoscopy.
What Should I Ask My Doctor On Behalf Of My Child Or Teenager
Ask your healthcare provider the following questions in addition to the ones listed above:
- What vitamins should my child take?
- Will my other children have pediatric ulcerative colitis?
- Is my child at risk for other conditions?
- Can you recommend a psychiatrist or therapist to help my child with emotional issues related to pediatric ulcerative colitis?
- Is my child growing at a normal rate?
- What can I do to help my child cope at school?
A note from Cleveland Clinic
When you have ulcerative colitis, its essential to work closely with your healthcare team.
Take your medications as prescribed, even when you dont have symptoms. Skipping medications youre supposed to take can lead to flareups and make the disease harder to control. Your best shot at managing ulcerative colitis is to follow your treatment plan and talk to your healthcare provider regularly.
Read Also: Wound Vac For Pressure Ulcers
Difference Between Ulcerative Colitis And Diverticulitis Causes
As mentioned, the immune system is suspected to play a role in ulcerative colitis, along with genetics and environmental factors. Certain genes seem to be involved in the development of ulcerative colitis, and having more than four family members with this condition increases your risk of developing it, too. Environmental factors include place of residence, especially because there are higher rates of ulcerative colitis in urban areas, North America, and Western Europe. Air pollution, medications, and certain diets have also been found to be associated with a higher risk of ulcerative colitis.
Weak spots along the bottom of the large intestine can prompt the formation of diverticula. When pressure is added, bulges form. These bulges, or pouches, may protrude through the colon wall. When they burst or get infected, this marks the diagnosis of diverticulitis. It is worth noting that diverticula themselves do not necessarily create symptoms.
Comparing Ulcerative Colitis And Diverticulitis Signs And Symptoms
Ulcerative colitis symptoms include abdominal pain, increased abdominal sounds, blood stools, diarrhea, fever, rectal pain, weight loss, malnutrition, joint pain and swelling, mouth sores, nausea, vomiting, and skin ulcers.
Signs and symptoms of diverticulitis include severe pain that may last for days and takes place in the lower left side of the abdomen, nausea and vomiting, fever, abdominal tenderness, constipation, and in some cases diarrhea .
Recommended Reading: Ulcerative Colitis Surgery Pros And Cons
Where To Find Help With All 3
Should you find yourself experiencing any of the symptoms laid out above, its imperative that you speak with a gastrointestinal specialist as soon as you can. At the Colorectal Clinic of Tampa Bay, your physician will do a deep dive with you on all of your symptoms, your daily habits, and your overall lifestyle to best understand which condition is truly to blame. We are well versed in treating Ulcerative Colitis, Crohns Disease, and Celiac Disease, having helped many patients throughout the Bay Area find relief. Schedule your first appointment with us now!
Crohns Disease Vs Diverticulitis: Us Prevalence
Prevalence of Crohns disease in the U.S. is 26 to 199 per 100,000 persons, and the incidence rate of Crohns disease is 3.1 to 14.6 cases per 100,000 person-years.
Roughly two million people in the U.S. suffer from diverticular disease. Prevalence rate is one in 136, or 0.74 percent. Annually, 300,000 new cases of diverticulitis are diagnosed.
Read Also: Different Types Of Ulcerative Colitis
Key Difference Colitis Vs Diverticulitis
Colitis and diverticulitis are two inflammatory diseases of the colon that are difficult to be diagnosed solely based on the clinical features. The inflammation of the colon is known as colitis. Diverticulitis is the inflammation of the diverticula in the colon. As seen from the definitions, colitis is a condition that occurs in the colon whereas diverticulitis is a condition that takes place in the diverticula. This is the main difference between colitis and diverticulitis.
When To See A Doctor
Schedule a doctor’s visit, Mayo Clinic suggests, if you have these symptoms of colitis:
- Abdominal pain
- Diarrhea that continues even after you treat it with over-the-counter drugs
- Diarrhea that wakes you up
- A fever that lasts for more than a day or two without explanation
Schedule a doctor’s visit if you have these symptoms of diverticulitis: Continuous abdominal tenderness or pain without an obvious reason, especially if you also have a fever and constipation or diarrhea.
Keep in mind that any unusual signs should prompt a visit to your doctor. Don’t try to diagnose these conditions on your own, warns Dr. Stollman.
Don’t Miss: How To Check A Horse For Ulcers
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
- Alcohol.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Salt.
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
Differentiating Crohns Disease And Diverticulitis Treatment
Crohns disease has a long list of treatment methods, because there is no exact cause to target. Treatment for Crohns disease may include corticosteroids, anti-inflammatory drugs, immunosuppressant agents, antibiotics, biologic agents, nutritional and dietary counseling, stress management, and, in severe Crohns disease cases, surgery to remove heavily affected areas of the intestines and colon.
Medical treatments for diverticulitis include antibiotics to treat infection, liquid diet to allow bowels to heal, and over-the-counter pain relievers. In complicated cases of diverticulitis, surgery may be required, such as primary bowel resection, where the affected part of the intestine is removed and the rest of it is reconnected. Another option is bowel resection with colostomy if it is impossible to reconnect the colon to the rectum due to inflammation.
If diverticulitis is causing pain, there are home remedies you can try for relief. To reduce muscle cramping caused by diverticulitis, you can apply heat to the abdomen. Meditation, too, may be beneficial in managing the associated pain. Lastly, if you need to opt for a pain reliever, stay away from ibuprofen and instead reach for acetaminophen .
There are also some preventative measures you can try to lower your risk of developing diverticulitis.
Don’t Miss: Side Effects Of Ulcerative Colitis
Symptoms Of Diverticular Disease And Diverticulitis
Symptoms of diverticular disease include:
- tummy pain, usually in your lower left side, that tends to come and go and gets worse during or shortly after eating
- occasionally, blood in your poo
If your diverticula become infected and inflamed , you may suddenly:
- get constant, more severe tummy pain
- have a high temperature
- get mucus or blood in your poo, or bleeding from your bottom
Role Of Inflammation In The Pathogenesis Of Diverticular Disease
Antonio Tursi
1Gastroenterology Service, ASL BAT, Andria, Italy
2Gastroenterology Unit, ASL Roma 6, Albano Laziale, Roma, Italy
Abstract
Diverticulosis of the colon is the most common condition in Western societies and it is the most common anatomic alteration of the human colon. Recurrent abdominal pain is experienced by about 20% of patients with diverticulosis, but the pathophysiologic mechanisms of its occurrence are not completely understood. In the last years, several fine papers have showed clearly the role of low-grade inflammation both in the occurrence of symptoms in people having diverticulosis, both in symptom persistence following acute diverticulitis, even if the evidence available is not so strong. We do not know yet what the trigger of this low-grade inflammation occurrence is. However, some preliminary evidence found colonic dysbiosis linked to low-grade inflammation and therefore to symptom occurrence in those patients. The aim of this paper is to summarize current evidences about the role of inflammation in symptom occurrence in symptomatic uncomplicated diverticular disease and in symptom persistence after an episode of acute diverticulitis.
1. Introduction
Most people with colonic diverticulosis remain asymptomatic. Just about one-fourth to one-fifth of those people will develop symptoms without complications, experiencing the so-called Symptomatic Uncomplicated Diverticular Disease , and about 20-25% of them will ultimately develop diverticulitis .
Also Check: Best Treatment For Diabetic Foot Ulcer
Whats New In Treating Ulcerative Colitis And Diverticulitis
New paradigms and new management in treating these diseases
OUR UNDERSTANDING of ulcerative colitis and diverticulitis is changing, according to Jonathan Terdiman, MD, who directs the gastroenterology department at University of California, San Francisco. Dr. Terdiman, who spoke at UCSFs management of the hospitalized patient conference last fall, pointed out new developments in treating those conditions, as well as common mistakes clinicians make.
Physicians often dont recognize soon enough, for instance, when ulcerative colitis patients are failing steroids. Doctors also need to change how they dose infliximab in those patients.
Even more far-reaching: Experts are now developing a new way of thinking about diverticular disease, seeing it as more of an immune disorder than an infection. That new paradigm, Dr. Terdiman explained, could broadly affect treatment and management.
An ulcerative colitis diagnosisUlcerative colitis, which ranges from mild to fulminant, comes with many predictors of bad outcome. By bad outcome, we mean people who end up leaving the hospital without their colons, Dr. Terdiman said.
Infliximab is not just an induction drug but a maintenance drug.
~ Jonathan Terdiman, MDUniversity of California, San Francisco
Those predictors include stool frequency , percentage of bloody stools, a fever of more than 37.5 degrees, a heart rate over 90 beats per minute, and a CRP greater than 25.
Key Difference Diverticulitis Vs Ulcerative Colitis
In the medical jargon, the suffix itis is almost always used to describe something to do with inflammation. According to that preamble, you can understand that diverticulitis is the inflammation of the diverticula that arise from the colon. Ulcerative colitis, on the other hand, is the inflammation of the colon with the formation of associated ulcers. In ulcerative colitis, the overlying mucosa of the colon is inflamed, but in diverticulitis, it is the diverticulum arising from the colon that gets inflamed. This is the key difference between diverticulitis and ulcerative colitis.
Also Check: How Long Does An Ulcerative Colitis Flare Up Last
Diagnosis For Crohns Disease And Diverticulitis
Crohns disease is diagnosed through a detailed examination of ones medical and family history, as well as additional testing as needed.
Because Crohns disease can mimic other conditions like infections, diverticulitis, and cancer, its important to rule them out. Blood tests are ineffective in diagnosing Crohns disease, so an ultrasound, CT scan, MRI, colonoscopy, and internal biopsy may be conducted.
To properly diagnose diverticulitis, your doctor will conduct a physical examination, checking your abdomen and pelvic region. Other tests include blood tests, pregnancy test for women, liver function tests, stool tests, and CT scans, which can help gauge severity of diverticulitis.
Tests For Diverticular Disease And Diverticulitis
After taking your medical history and listening to your symptoms, the GP may first want to rule out other conditions, such as irritable bowel syndrome , coeliac disease or bowel cancer.
These often have very similar symptoms to diverticular disease.
This may involve blood tests. If necessary, you’ll be referred for a colonoscopy, a CT scan, or sometimes both.
Recommended Reading: Does Smoking Cause Ulcers After Gastric Bypass
Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
Ulcerative Colitis Vs Diverticulitis: Us Prevalence
The CDC estimated that one to 1.3 million Americans are affected by IBD. Generally, ulcerative colitis is more prevalent in males than females.
Roughly two million people in the U.S. suffer from diverticular disease. Prevalence rate is one in 136, or 0.74 percent. Annually, 300,000 new cases of diverticular disease are diagnosed.
Recommended Reading: L Glutamine Ulcerative Colitis Dosage
My Experience With The Covid
With the vaccine behind me, I feel hopeful for the future for the first time in over a year.
Having an autoimmune disease is tough physically, mentally, and emotionally. Having an autoimmune disease during a pandemic? That is a completely new experience that I wasnt prepared for.
I have ulcerative colitis , a type of inflammatory bowel disease , and have been fighting a flare-up off and on throughout all of 2020. I like to say that I was quarantining before quarantining was cool.
I finally felt a glimmer of hope mixed with a twinge of uncertainty when the Centers for Disease Control and Prevention announced that a COVID-19 vaccine was finally available.
Was it going to work? Was it going to make my disease worse? So many questions were living rent-free in my brain.
I did so much research about the effects of the vaccine on people with IBD and initially found very little. I want to share my experience in the hope that it will help you make an educated decision on COVID-19 vaccination for yourself.