Key Points To Remember About Pressure Ulcers
- Staging refers to the amount of tissue that was damaged. In the case of a Stage 4 pressure ulcer, there is damage to the underlying structures that will never regenerate with the type of tissue that was damaged. Scar tissue is not as strong as healthy tissue and is more likely to break down again.
- If there is scarring on a patients body, it has to have come from a Stage 3 or 4 pressure ulcer!
- If documentation stated that the wound is a Stage 3 and muscle is documented as assessed in the wound bed, it is not a correct assessment. That description is indicative of a Stage 4 pressure ulcer.
- If the documentation stated that Stage 4 is healing and now presents as a Stage 2, that is inappropriate staging. A full thickness wound never becomes a partial thickness wound.
- Slough and eschar will only form in full thickness wounds, not partial thickness wounds. If the wound was a Stage 2 and had slough or eschar present, it was inappropriately assessed as a Stage 2. It should have been staged as a Stage 3 or 4.
- Unstageable pressure ulcers and Deep Tissue Injury pressure ulcers have been considered as additional pressure ulcer stages by the NPUAP since 2007.
Has anyone found that the documentation is the key to a successful case or the downfall of the case?
Med League provides with expertise in evaluating pressure ulcer cases. for assistance.
How Do We Measure Our Pressure Ulcer Rates And Practices
A basic principle of quality measurement is: If you can’t measure it, you can’t improve it. Therefore, pressure ulcer performance must be counted and tracked as one component of a quality improvement program. By tracking performance, you will know whether care is improving, staying the same, or worsening in response to efforts to change practice. Moreover, continued monitoring will be key to understanding where you are starting and to sustaining your improvement gains.
During the course of your pressure ulcer prevention improvement effort and on an ongoing basis, you should regularly assess your pressure ulcer rates and practices. We recommend that you regularly monitor:
The questions in the rest of this section will help you develop measures and processes for assessing pressure ulcer rates and practices.
Treatment Of Stage 3 And Stage 4 Pressure Ulcers
The goal of treatment for stage 3 and 4 pressure ulcers, is to properly debride and dress the wound cavity, create or maintain moisture for optimal healing, and protect the wound from infection. The goal of properly unloading pressure from the area still applies. At these pressure ulcer stages, more emphasis should be placed on proper nutrition and hydration to support wound healing. If the extent of the pressure ulcer or other factors prohibit it from healing properly, surgery may be necessary to close the wound.
The following precautions can help minimize the risk of developing pressure ulcers in at-risk patients and to minimize complications in patients already exhibiting symptoms:
- Patient should be repositioned with consideration to the individualâs level of activity, mobility and ability to independently reposition. Q2 hour turning is the standard in many facilities, but some patients may require more or less frequent repositioning, depending on the previous list.
- Keep the skin clean and dry.
- Avoid massaging bony prominences.
- Provide adequate intake of protein and calories.
- Maintain current levels of activity, mobility and range of motion.
- Use positioning devices to prevent prolonged pressure bony prominences.
- Keep the head of the bed as low as possible to reduce risk of shearing.
- Keep sheets dry and wrinkle free.
Read Also: What Is A Good Diet For Ulcerative Colitis
Checklist For Measuring Progress
5. Checklist for measuring pressure ulcer rates and practices
| Measuring pressure ulcer rates | |
|
___ |
| Measuring key processes of care | |
|
___ |
Scoring With The Braden Scale

Each category is rated on a scale of 1 to 4, excluding the ‘friction and shear’ category which is rated on a 1-3 scale. This combines for a possible total of 23 points, with a higher score meaning a lower risk of developing a pressure ulcer and vice versa. A score of 23 means there is no risk for developing a pressure ulcer while the lowest possible score of 6 points represents the severest risk for developing a pressure ulcer.The Braden Scale assessment score scale:
- Very High Risk: Total Score 9 or less
- High Risk: Total Score 10-12
- Moderate Risk: Total Score 13-14
- Mild Risk: Total Score 15-18
- No Risk: Total Score 19-23
Read Also: How Does One Get Ulcerative Colitis
Audit Of Monitoring Systems
Based on the work of Fletcher and the outcomes of debate within the East of England Tissue Viability Group, the Tissue Viability Society called a consensus meeting to attempt to solve some of the issues a report followed, but little changed as a result.
In 2015, following petitioning from the East of England Tissue Viability Group, the NHS England safety team commissioned the TVS to undertake a project to further measure the extent of disparities and inaccuracies in pressure ulcer reporting. Monitoring systems were audited in 24 organisations in two audits .
Smith et al found:
- Significant under-reporting via the Safety Thermometer their audit identified 160 patients with a pressure ulcer, compared with 105 reported
- Significant under-reporting via an IRS their audit identified 189 patients with a pressure ulcer, compared with 135 according to the IRS approximately half the patients identified by the audit had also been identified by the IRS however, 34 of those identified in the IRS were not in the audit, which found that 11 had wounds with different aetiologies and 23 had healed pressure ulcers or other types of wounds.
From both audits, it was clear that it was not possible to compare pressure ulcer prevalence and incidence rates between organisations.
Braden Scale For Predicting Pressure Ulcer Risk
| Braden Scale for Predicting Pressure Ulcer Risk | |
|---|---|
| Purpose | assess risk of pressure ulcer |
The Braden Scale for Predicting Pressure Ulcer Risk, is a tool that was developed in 1987 by Barbara Braden and Nancy Bergstrom. The purpose of the scale is to help health professionals, especially nurses, assess a patient’s risk of developing a pressure ulcer.
Read Also: Best Treatment For Diabetic Ulcers
Analysis Of Existing Evidence
The effect of pressure ulcers on patients, nurses, and hospitals is outlined in academic literature. Qaseem et al. find that the prevention of bedsores is much more beneficial than their treatment. First of all, pressure ulcers are dangerous to the health of patients as it is described above. Skin damage and the following infections increase morbidity and mortality, putting patients at increased risk of complications and prolonged length of stay at the hospital .
Second, clinicians also encounter challenges in dealing with bedsores as the latter require adequate assessment and difficult treatment. Prevention, on the other hand, can be performed in steps that have been tested and documented. Finally, the rate of ulcers affects hospitals and units as it is one of the factors of healthcare organizations ratings. The high incidence of bedsores implies the poor quality of service, low rating of the unit, and decreased financial support.
In order to adequately address the issue, it is necessary to understand how pressure ulcers can be measured. According to Fletcher and Hall , nurses may face many challenges due to hospitals having different records of patients with pressure ulcers. Some of the wounds may be called bedsores, while others may have names such as moisture-associated dermatitis or sacral and gluteal lesions .
Review Question: What Are The Most Reliable Techniques/tools To Measure The Dimensions Of A Pressure Ulcer
One systematic review looked at the performance of instruments designed for measuring the dimensions of pressure ulcers. This systematic review was included in the current evidence review and it was subsequently updated to include 1 other study . Overall 13 studies were included in the evidence review.,,,,,,,,,,,, Evidence from these is summarised in the clinical GRADE evidence profile below. The quality of these studies is outlined in .
The O’Meara review looked at studies of any design which reported an evaluation of a pressure ulcer measurement instrument as the main focus of the investigation. The authors did not include assessment checklists where the focus was the performance of the tool overall rather than the measurement of pressure ulcer dimensions.
Recommended Reading: Are Eggs Bad For Ulcerative Colitis
Procedure And Data Analysis
Demographic and clinical data to describe the population were collected. This included the American Spinal Injury Association Impairment Scale and neurological level of injury according to the International Standards for Neurological Classification of Spinal Cord Injury. In addition, each pressure ulcer was scored on the Pressure Ulcer Scale for Healing version 3.0. The PUSH tool version 3.0 rates pressure ulcers according to the surface area of the pressure ulcer, amount of exudate and type of tissue damage. The total scores range from 0 to 17 points, with higher scores indicating a severe pressure ulcer and a score of zero representing no pressure ulcer. The original plan was to correlate the undermining scores with the PUSH to provide some evidence about the validity of the undermining measurements. However, this aspect of the study was subsequently abandoned when it became clear that the PUSH was not a reasonable gold standard for undermining. We, however, report the PUSH data and its correlation with the undermining scores.
Symptoms Of Stage 3 And Stage 4 Pressure Ulcers
Stages 3 and 4 pressure ulcers have deeper involvement of underlying tissue with more extensive destruction. Stage 3 involves the full thickness of the skin and may extend into the subcutaneous tissue layer granulation tissue and epibole are often present. At this stage, there may be undermining and/or tunneling that makes the wound much larger than it may seem on the surface. Stage 4 pressure ulcers are the deepest, extending into the muscle, tendon, ligament, cartilage or even bone.
Figure 1: Stage 4 sacral pressure ulcerFigure 2: Stage 3 pressure ulcer on hip
Read Also: What To Eat During An Ulcerative Colitis Flare
Measuring Quality Of Life
Dr. Simon Palfreyman examines the impact of pressure ulcer interventions
Simon Palfreyman and Brendan Mulhern – 28 January 2016
Pressure ulcers are wounds that result when people are immobile or have reduced mobility. They tend to occur over bony prominences. Pressure ulcers can range from superficial skin damage to deep, extensive wounds that extend through to the bone. The prevention and treatment of pressure ulcers have been identified as major costs for health-care providers.
In order to compare interventions to prevent or treat pressure ulcers it is necessary to be able to examine their impact on quality of life. This can be done through the use of preference-based patient reported outcome measures , which are questionnaires that ask about the participant’s state of health. PROMs are grouped into those that are designed for only those with a specific condition and generic ones that can be completed by a wide range of people with many different health problems. It is currently unclear which of these are best for people with pressure ulcers.
The purpose of the study was to explore the feasibility of using generic PROMs in patients with pressure ulcers or at risk of developing pressure ulcers.
Approach
Highlights of the findings
The presence of an ulcer had a negative impact on quality of life and also led to a perceived lower level of dignity. The PROM questionnaires were able to measure the difference between those who had an ulcer and those who did not have an ulcer.
Pressure Ulcer Stages 1 2 3 And 4
- A stage I pressure ulcer has redness on the surface of the skin that does not disappear when pressure is relieved.
- A stage 2 ulcer is a partial thickness wound. This means there is damage to the epidermis and the dermis . Both of these are superficial or shallow wounds. As they heal there is no scar tissue formation and the tissues damaged will regenerate as healing takes place. This is one of the reasons it is so important for the healthcare team to correctly treat pressure ulcers to reduce the risk of them progressing to more involved wounds.
- Stages 3 and 4 are full thickness wounds, which are much worse.
- Stage 3 is injury into the subcutaneous tissue but not through to the underlying structures, i.e. the muscle, bone and/or tendon.
- Stage 4 is an injury that is very deep and muscle, bone and/or tendon will be exposed in the wound bed. Full thickness pressure ulcers are deeper and heal by scar tissue formation. There is no regeneration of the underlying tissues. The development of these ulcers gets the most attention from attorneys and their experts. The damages are significant.
You May Like: How To Treat Mouth Ulcers
Measuring Key Processes Of Care
5.2.1 Why measure key processes of care?
While measuring pressure ulcer rates is the ultimate test of how your facility or unit is performing, pressure ulcer rates are limited in that they do not tell you how to improve care. If your pressure ulcer rate is high, on what specific areas should you focus? To know where to focus improvement efforts, it is important to measure key processes of care. Many important processes of care could be measured in assessing pressure ulcer prevention. We recommend initially looking at no more than three:
- Performance of comprehensive skin assessment within 24 hours of admission.
- Performance of standardized risk assessment within 24 hours of admission.
- Performance of care planning that addresses each deficit on standardized risk assessment.
5.2.2 What data sources should be used in measuring key processes of care?
Much pressure ulcer preventive care may not be documented. Nonetheless, we recommend medical record reviews as the source of data on the performance of key processes of care. While rates may initially be low because of poor documentation, this finding will encourage improved documentation of the care actually being provided.
Tools
Use this tool developed by the Quality Improvement Organization program for abstracting medical record data .
5.2.3 How do we ensure performance of comprehensive skin assessment within 24 hours of admission?
Tools
A sample protocol for checking skin assessments is available in Tools and Resources .
Tools
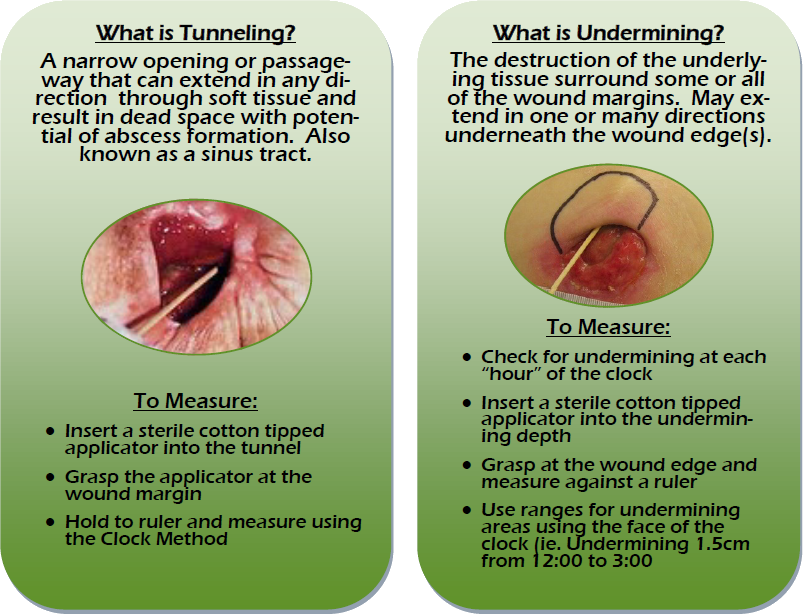
How To Assess Wounds For Tunneling And Undermining
As part of a thorough wound assessment, in addition to noting location and measuring size, the entire wound bed should be probed for the presence of tunneling and/or undermining. If you are unsure what tunneling and undermining are and how to recognize these phenomena, here’s an explanation of these terms and how to assess wounds for their presence.
Recommended Reading: Nutritionist Specializing In Ulcerative Colitis
How Do You Measure Pressure Ulcers
5/5Assessulcer
Pressure ulcer areas were measured using 3 techniques: measurement with a ruler , wound tracing using graduated acetate paper, and digital planimetry.
Additionally, how often should pressure ulcers be assessed? The Institute for Healthcare Improvement has recently recommended that in hospitalized patients, pressure ulcer risk assessment be done every 24 hours44 rather than the previous suggestion of every 48 hours.
Correspondingly, how do you measure the size of a wound?
Direct measurement Direct measurement involves measuring the wound at its longest length and its widest width. Width should be measured perpendicular to the length. By multiplying the length times the width , you will obtain the surface area of the wound. To measure wound depth, you will need a probe.
How do you assess pressure ulcer risk?
A number of tools have been developed for the formal assessment of risk for pressure ulcers. The three most widely used scales are the Braden Scale, the Norton Scale, and the Waterlow Scale.
Information Sources And Searches
Guidelines, systematic reviews, reports, online documents, and books were searched as long as they met the inclusion criteria. A combined search of the Embase and Medline databases was conducted via OVID . Available systematic reviews22, 23 were used to search for the original publications. In addition, numerous databases and websites were searched, including:
Also Check: What Are Diabetic Leg Ulcers
Pressure Ulcers: Prevention Evaluation And Management
DANIEL BLUESTEIN, MD, MS, Eastern Virginia Medical School, Norfolk, Virginia
ASHKAN JAVAHERI, MD, Stanford University School of Medicine, Stanford, California, and Veterans Affairs Palo, Alto Health Care System, Palo Alto, California
Am Fam Physician. 2008 Nov 15 78:1186-1194.
Pressure ulcers, also called decubitus ulcers, bedsores, or pressure sores, range in severity from reddening of the skin to severe, deep craters with exposed muscle or bone. Pressure ulcers significantly threaten the well-being of patients with limited mobility. Although 70 percent of ulcers occur in persons older than 65 years,1 younger patients with neurologic impairment or severe illness are also susceptible. Prevalence rates range from 4.7 to 32.1 percent in hospital settings2 and from 8.5 to 22 percent in nursing homes.3
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Compared with standard hospital mattresses, pressure-reducing devices decrease the incidence of pressure ulcers.
| Clinical recommendation | |
|---|---|
|
There is no evidence to support the routine use of nutritional supplementation and a high-protein diet to promote the healing of pressure ulcers. |
|
|
Heel ulcers with stable, dry eschar do not need debridement if there is no edema, erythema, fluctuance, or drainage. |
|
|
Ulcer wounds should not be cleaned with skin cleansers or antiseptic agents because they destroy granulation tissue. |
SORT: KEY RECOMMENDATIONS FOR PRACTICE