Living With An Ileostomy
You can live a long, active, and productive life with an ileostomy. In many cases, ileostomy patients can participate in the same activities they did before the surgery, including sports, outdoor activities, swimming and other watersports, travel, and work.
Whether your ileostomy is permanent or temporary, it is common for patients to initially feel self-conscious about their ostomy and you may notice a change in how you feel about your body image. Some patients prefer to limit how visible the bag is to others. The ostomy bag typically lays fairly flat under your clothing.
Remember, it is just as important to take care of your mental and emotional health as it is your physical health. Speak with your doctor or a mental health professional if you feel you are experiencing symptoms of depression or anxiety.
-
There are several pouching systems for you to choose from. You will learn how to use your system as well as how to care for the skin surrounding the stoma.
-
Talk to your doctor about any specific dietary restrictions with an ileostomy. It is important for you to drink plenty of fluids to avoid dehydration and loss of electrolytes.
-
Eating foods high in pectin, including applesauce, bananas, and peanut butter, will help thicken your stool output and control diarrhea. Discuss this with your doctor.
The United Ostomy Associations of America has additional resources as you learn to live with your ostomy.
Timing Of Surgical Intervention
Timing of the surgical intervention is the major preoperative concern in UC. Emergency surgery should be avoided if possible, but if it is indicated, most advocate use of a staged procedure. Initially, emergency total colectomy with end ileostomy is performed to alleviate the major symptoms of the disease, including bleeding and pain, and allows the patient to be weaned from steroids.
Later, an IPAA is created, if the patient desires it, with removal of the remaining rectum. Most advocate leaving the rectum in place during the initial emergency operation to prevent disruption of the pelvic tissue planes, with the aim of making the subsequent pelvic dissection safer. If the patient has mild disease or disease in remission, total proctocolectomy with the creation of an IPAA may be performed as the initial definitive procedure.
Refractory Course And Corticosteroid Resistance
A treatment-refractory course, despite the use of immunosuppressive drugs including biologicals, represents an absolute indication for surgery. Similarly, the patient should be operated on if corticoid dependence is obvious, i.e. the corticoid medication cannot be lowered below the Cushing threshold of 7.5 mg of prednisolone equivalent daily. From this course of the disease, which comprises weeks or months, the intractable fulminant flare must be distinguished which cannot be controlled even by high doses of corticosteroids and requires emergency surgery.
Don’t Miss: Foam Boots For Pressure Ulcers
How To Talk To Your Child About Ulcerative Colitis
Its important to help your child feel comfortable to share changes in symptoms, or when theyve missed a medication dose. Here are some ways to help them cope with symptoms and to feel confident about opening up to you:
- Ask them for updates on how they feel both mentally and physically.
- Use language they can understand. Medical terminology can be scary and confusing, so be sure to explain things at their level.
- Dont diminish the severity of their symptoms. Make sure they feel like they can keep you informed of any changes in how theyre feeling. This can be especially true for psychological symptoms like anxiety and depression.
- Make sure children know that their condition isnt their fault and that they arent alone. Online support groups, forums, and even specialized summer camps can be a good way to share other childrens stories.
- Be an advocate for your child with all medical professionals to let them know that you have their back.
- Remember to take care of yourself as a caregiver. Its easy to let your own needs slide when caring for others.
Surgical Management In Ulcerative Colitis
- Surgical Management in Ulcerative Colitis
Embed Size
TRANSCRIPT
- 1.SURGICAL MANAGEMENT IN ULCERATIVE COLITIS
2. UC & CRC 3. INCIDENCE
- CRC in UC appears at younger age than in sporadic CRC .
- 5-10% after 20 years.
- UC complicated by primary sclerosing cholangitis
- Presence of post-inflammatory pseudopolyp
- Mostly located in the rectum and sigmoid
- It arises from areas of dysplasia.
- Dysplastic areas may appear flat or slightly raised areas.
- Dysplastic areas may occurwithinornearnodules, masses, polyps or plaque like lesion.
- N.B.: Diagnosis of dysplasia in Pre Op colonoscopy has a:
- 81%sensitivity
7. Surgical management in UC 8. Indications for surgery in UC:
- SURGICAL EMERGENCIES
- Toxic megacolon with impending perforation
- Fulminant colitis unresponsive to IV corticosteroids
- Colonic perforation
- Dysplasia-associated lesion or mass
- Intolerable side effects of medications
- Patient with significant risk to develop CRC
- Stricture formation without obstruction
- Growth retardation, primarily in children and adolescents
- Subtotal colectomy with end ileostomy
- Proctocolectomy with end ileostomy
- Blow-hole colostomy with end ileostomy
- Subtotal colectomy with end ileostomy
- Advantages : Allows option for IPAA low risk
- Disadvantages :
- may develop rectal recurrence of disease
- Contraindication :Massive hemorrhage from colon and rectum
- moderate risk for perineal nerve damage
- Contraindication :Severely toxic or unstable patient
- Blow-hole colostomy with end ileostomy
Also Check: Can You Drink Coffee With Ulcerative Colitis
Surgical Management Of Ulcerative Colitis
- Surgical Management of Ulcerative Colitis
Embed Size
TRANSCRIPT
Colon And Rectal Carcinomas
The finding of a colon or rectal cancer in a patient with UC is unfortunate. Colon cancers of relative early stage can be treated by proctocolectomy and IPAA, Kock pouch or Brooke ileostomy . Metastatic colon tumors to the liver should be treated with proctocolectomy with Brooke ileostomy or abdominal colectomy and ileorectal anastomosis. The treatment of patients who are lymph node positive is best by proctocolectomy and Brooke ileostomy. If the patient is very adverse to a stoma, IPAA could be carried out.
Rectal carcinoma in the middle and lower rectum is a contraindication for IPAA. A standard proctectomy is advisable and a permanent Brooke ileostomy. These patients are prone to local recurrence, and thus radiation therapy may be required in the future. Patients with upper rectal tumors may safely undergo IPAA, but in the case of a large, advanced tumor, proctocolectomy with Brooke ileostomy is advisable .
Don’t Miss: How Do I Know If I Have A Peptic Ulcer
Allergic Colitis In Infants
Allergic colitis is a condition that can occur in infants, usually within the first months after birth. The condition can cause symptoms in infants including:
- reflux
- fussiness
- possible flecks of blood in a babys stool
Doctors dont know exactly what causes allergic colitis. One of the most popular theories is that infants with allergic colitis have an allergic or hypersensitive reaction to certain components in breast milk. A 2020 review of studies indicated that a protein allergy, either through breast milk, cows milk, or formula, could contribute.
Eosinophilic colitis is a type of allergic colitis that can also show up in infants with these symptoms. Its causes are similarly unknown , but its likely also related to a protein allergy.
Doctors will often recommend an elimination diet for the birthing parent, which involves slowly cutting out certain foods known to contribute to allergic colitis. Examples include cows milk, eggs, and wheat. If the baby stops having symptoms of allergic colitis, these foods were likely causing the problem.
In severe cases, monoclonal antibodies, such as those used to inflammatory bowel disease , may also be another treatment option.
Risk Of Cancer And Dysplasia
Compared to the general population, the risk of colorectal cancer is increased in patients with UC . Accordingly, a surveillance colonoscopy should be performed annually in patients with pancolitis and a disease duration 8 years. Patients with a left-sided or distal colitis should be submitted to surveillance colonoscopy every 1 or 2 year after a disease duration of 15 years .
In case of a histologically proven colitis-associated high-grade intraepithelial neoplasia /dysplasia a proctocolectomy is indicated after the diagnosis has been confirmed by an external pathologist. For resection of manifest colitis-associated cancer, the same principles apply as for the oncological resection of sporadic colorectal cancer.
In the presence of a low-grade IEN/dysplasia in flat mucosa – also confirmed by an external pathologist – either proctocolectomy or an endoscopic biopsy control within 3 months should be offered to the patient . The patient has to be informed of the risk of malignancy. In this situation, other centers and we advise the patient to undergo surgery because a sampling error’ represents a significant risk of missing a high-grade dysplasia or carcinoma in repeated colonoscopies.
Read Also: Can Diverticulitis Cause Ulcerative Colitis
Elective Colorectal Cancer Surgery
Patients with Crohns disease and ulcerative colitis have a higher risk for colorectal cancer than the general population, so elective surgery may be recommended to eliminate that risk.
Colorectal cancer risk factors
-
The risk of CRC increases after living with IBD for 8 to 10 years
-
The risk increases the longer a person lives with IBD
-
The greatest risk is for people with IBD affecting their colon
-
Patients who have a family history of primary sclerosing cholangitis are also at higher risk of developing colorectal cancer
In most cases, colorectal cancer starts as a polyp, or a small lump growing from the wall of the intestine. Polyps typically start out benign but become cancerous over time. But in patients with IBD, abnormal and potentially precancerous tissue, called dysplasia, may lay flat against the wall of the intestine and can even be found in areas of the intestinal wall that appear normal during a colonoscopy.
Choice Of Ileal Pouch Size And Type
The creation of an IPAA involves total proctocolectomy, with folding of the distal ileum into a J, S, or W formation to create a fecal reservoir. The anastomosis to the anus preserves continence function involving the internal and external anal sphincters. The S and W configurations have been associated with a failure rate as high as 66% and a need for revision however, the J configuration is associated with a need for revision in only 1-2% of cases.
Reasons for failure with S and W pouches include dilation of the reservoir, leading to stasis, and elongation of the spout at the anal anastomosis, leading to stenosis. These technical points are all but alleviated with the current technique of J pouch construction. Transanal defecation is restored in 88% of children with J pouches, whereas 32% of those with S pouches and 32% of those undergoing straight ileoanal pull-through procedures require revision.
Although most surgeons do not use the S pouch as the first option , the spout created in its construction provides an additional 3-5 cm in length to the entire ileal reservoir, as compared with the length of a J pouch.
However, others have noted a need for revision of the straight pull-through configuration in 70% of cases. Construction of the ileal J pouchanal anastomosis is described below. One should keep in mind that the straight ileoanal pull-through is performed in essentially the same manner and uses less total length of small bowel.
Also Check: What Foods Should I Avoid With A Stomach Ulcer
Ulcerative Colitis Surgical Procedures
The standard surgical procedure to treat ulcerative colitis is a proctocolectomy. This surgery removes both your colon and your rectum .
There are two types of proctocolectomy procedures used to treat ulcerative colitis.
-
Proctocolectomy with ileal pouch-anal anastomosis: Removal of the colon and rectum, and creation of an internal pouch that eliminates the need for a permanent external ostomy.
-
Proctocolectomy with end ileostomy: Removal of the colon, recturm, and anus and creation of an external ostomy.
It can feel overwhelming when you are recommended for one of these surgeries. We can help you understand whats involved with each surgery, and be prepared for life after your proctocolectomy.
Surgical Treatment Of Ulcerative Colitis
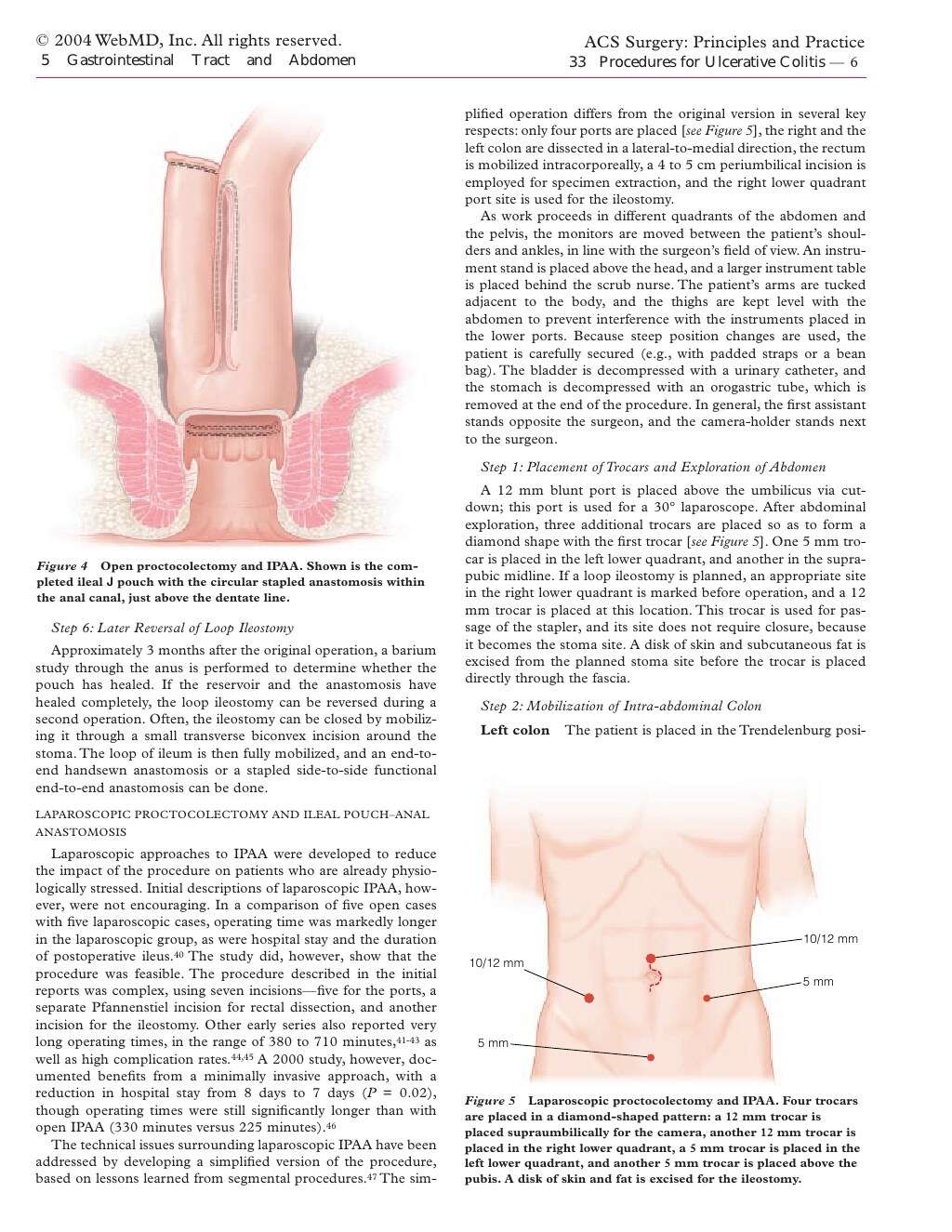
Restorative proctocolectomy with IPAA is the operation of choice for patients with UC it represents the only technique by which the substrate of the disease is completely removed and gastrointestinal continuity is reestablished. It is important to include the rectal mucosa down to the dentate line since residual tissue in this location may give rise to intractable pouchitis later on. Patients after IPAA can discontinue colitis-related medications, particularly immunosuppressants and immunomodulators, thereby avoiding associated adverse effects. In addition, the procedure substantially reduces the risk for dysplasia or cancer to the pouch itself in the rare cases where severe chronic pouchitis cannot be controlled.
Fig. 1
Regular pouchography before closure of ileostomy.
In recent years, there has been a trend towards performing a three-step procedure . The reason for this seems to be an intensified conservative therapy with increasing use of biologics. This entails the risk of surgical complications due to an often significantly reduced general condition of the patient. The three-stage procedure offers a better control in these cases. In contrast, a one-stage operation should be reserved only for young patients with good sphincter function, low activity of inflammation, good general condition, low-dose immunosuppressive therapy, and a totally tension-free IPAA. In our series this ideal condition is met in less than 10% of all patients.
Fig. 2
Recommended Reading: Support Surfaces For Pressure Ulcer Prevention
Perioperative Care Of Patients With Ibd
Good perioperative care always ensures better surgical results. Patients undergoing surgery for IBD must be prepared psychologically and medically.
Psychological preparation should start by explaining the patient the need for surgery. In this approach the surgeon must be aided by the gastroenterologist that has managed the patient for a long time in most of the cases. After acceptance of surgery, the patient must be explained the objectives, the advantages and disadvantages of each surgical intervention and the decision must be taken in common. People that will be submitted to stomas should also get a consultation from stomatherapist.
Medical preparation of the patients includes correction of hemoglobin, volemia, electrolytes and acid-base levels, coagulopathy, liver function. Total parenteral nutrition may be necessary in patients with nutritional deficits. Coexisting diseases should also be addressed. Any corticosteroid and immunosuppressive therapy should be discontinued before surgery, but corticosteroids need to be tapered immediately after surgery.
Perforation Of The Colon
Chronic inflammation caused by ulcerative colitis can weaken the wall of the colon until a hole, or perforation, develops. Once the colon has been perforated, the contents of the intestine can spill into the abdomen and cause a serious infection called peritonitis.
This is a potentially life-threatening condition that needs immediate medical treatment.
You May Like: Black Tarry Stools Ulcerative Colitis
When To Speak With Your Childs Doctor
Children can be especially challenging to diagnose. Reach out to your childs doctor if you notice continued abdominal pain, diarrhea, unexplained weight loss, unexplained rashes, or notice any blood in their stool.
Early detection is key to preventing complications, so keep an open dialogue with your child about symptoms and speak with their doctor to rule out other conditions.
Sudden Severe Ulcerative Colitis
This complication is the main cause of emergency surgery in patients with ulcerative colitis. With sudden, severe ulcerative colitis, medications and intravenous steroids, are unable to control the symptoms.
-
Uncontrolled bleeding can occur from deep ulcerations in the colon, though that is rare.
-
Severe, sudden ulcerative colitis can lead to toxic megacolon, a potentially life-threatening complication caused by severe inflammation.
-
Toxic megacolon leads to rapid enlargement of the colon. Symptoms include pain, distension or swelling of the abdomen, fever, rapid heart rate, constipation, and dehydration.
-
Toxic megacolon requires immediate treatment and surgery.
Read Also: Snack Ideas For Ulcerative Colitis
Proctocolectomy With Brooke Ileostomy
Description of procedure
This procedure involves the surgical removal of colon, rectum, and anus with creation of a permanent Brooke ileostomy.
Indications
Most patients are suitable candidates for this operation irrespective of age. The choice of this operation is often appropriate for patients who wish to avoid the problems associated with ileoanal pouch procedure or those who are not suitable candidates for a resortative procedure, especially in elderly patients and those with poor sphincter function.
Contraindications
IPAA is now the surgical procedure of choice in most patients with UC .
Contraindications
Patients less than 60 years of age are preferred . Exceptions have been made in extremely physiological fit individuals with acceptable results. Short obese patients are advised to lose weight prior to operation as the ability of the ileal pouch to reach the anus for anastomosis is compromised by the limited mobility of a short thick small bowel mesentery. Tall patients can also be a challenge to get the pouch to reach the anus for anastomosis.
Operative factors
Complications
Bowel obstruction is common following all types of surgery for UC. The annual risk for patients following IAPP is 1 in 25, 1 in 49 for a Kock pouch, 1 in 66 for a proctocolectomy and Brooke ileostomy, and 1 in 71 for colectomy and ileorectal .
Outcome