What Is Toxic Megacolon What Are Its Risk Factors
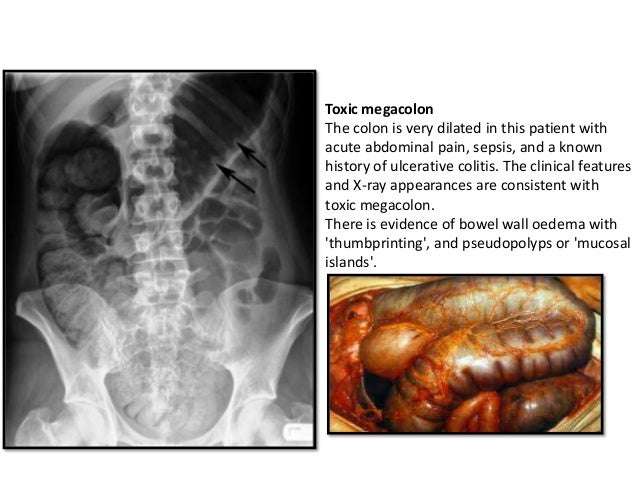
Toxic megacolon is a complication of colitis manifested by acute dilatation of the colon, with associated fever, tachycardia, leukocytosis, anemia, and postural hypotension. Transmural inflammation interferes with colonic motility, leading to colonic dilation and risk for perforation. Severe idiopathic panulcerative colitis carries the highest risk for toxic megacolon, but it may occur with any severe colitis . Performance of barium enema or colonoscopy or the administration of antimotility agents in patients with severe colitis may precipitate toxic megacolon.
James M. Messmer MD, MEd, in, 2008
Toxic Megacolon Complicating Ulcerative Colitis And Crohn’s Disease 1985 Oct
The clinical, laboratory and radiological data of 17 cases of toxic megacolon complicating either ulcerative colitis or Crohn’s disease , referred to the Department of Clinica Chirurgica II of the University of Bologna in a twenty year-period, are reviewed. The surgical strategies and results are compared and discussed, and the mortality and morbidity considered along with the important advances in resuscitative medicine and the employment of total parenteral nutrition .
What Are Warning And Precautions For Loperamide
Contraindications
- Hypersensitivity, bloody diarrhea, high fever, infectious diarrhea, and pseudomembranous colitis
- Patients in whom constipation must be avoided
- Avoid use as primarytherapy with acute dysentery , pseudomembranous colitis associated with antibiotic use)
- Children younger than 2 years
Effects of drug abuse
- See What Are Side Effects Associated with Using Loperamide?
Long-Term Effects
- See What Are Side Effects Associated with Using Loperamide?
Cautions
Also Check: Oral Antibiotics For Leg Ulcers
Toxic Megacolon In Ulcerative Colitis
- Sheldon C. BinderAffiliationsDepartments of Surgery and Medicine, Tufts University, School of Medicine and New England Medical Center Hospital, Boston, Massachusetts
- James F. PattersonCorrespondenceAddress requests for reprints to: Dr. James F. Patterson, New England Medical Center Hospital, 171 Harrison Avenue, Boston, Massachusetts 02111.AffiliationsDepartments of Surgery and Medicine, Tufts University, School of Medicine and New England Medical Center Hospital, Boston, Massachusetts
- b Dr. Glotzer’s present address is: Department of Surgery, Beth Israel Hospital, Boston, Massachusetts.Donald J. Glotzerb Dr. Glotzer’s present address is: Department of Surgery, Beth Israel Hospital, Boston, Massachusetts.AffiliationsDepartments of Surgery and Medicine, Tufts University, School of Medicine and New England Medical Center Hospital, Boston, Massachusetts
What Other Drugs Interact With Loperamide

If your medical doctor is using this medicine to treat your pain, your doctor or pharmacist may already be aware of any possible drug interactions and may be monitoring you for them. Do not start, stop, or change the dosage of any medicine before checking with your doctor, health care provider, or pharmacist first
- Loperamide has severe interactions with no other drugs.
- Loperamide has serious interactions with at least 23 other drugs.
- Loperamide has moderate interactions with at least 66 other drugs.
- Loperamide has minor interactions with the following drugs:
- itraconazole
This information does not contain all possible interactions or adverse effects. Visit the RxList Drug Interaction Checker for any drug interactions. Therefore, before using this drug, tell your doctor or pharmacist of all the drugs you use. Keep a list of all your medications with you, and share the list with your doctor and pharmacist. Check with your physician if you have health questions or concerns.
You May Like: What Foods Should Be Avoided With Stomach Ulcers
Antiperistaltic Agents Infectious Diarrhea
Major Potential Hazard, High plausibility. Applicable conditions: Infectious Diarrhea/Enterocolitis/Gastroenteritis
The use of drugs with antiperistaltic activity is contraindicated in patients with diarrhea due to pseudomembranous enterocolitis or enterotoxin-producing bacteria. These drugs may prolong and/or worsen diarrhea associated with organisms that invade the intestinal mucosa, such as toxigenic E. coli, Salmonella and Shigella, and pseudomembranous colitis due to broad-spectrum antibiotics. Other symptoms and complications such as fever, shedding of organisms and extraintestinal illness may also be increased or prolonged. In general, because antiperistaltic agents decrease gastrointestinal motility, they may delay the excretion of infective gastroenteric organisms or toxins and should be used cautiously in patients with any infectious diarrhea, particularly if accompanied by high fever or pus or blood in the stool. Some cough and cold and other combination products may occasionally include antimuscarinic agents for their drying effects and may, therefore, require careful selection when necessary.
References
Pathophysiology Of Ulcerative Colitis
Ulcerative colitis usually begins in the rectum. It may remain localized to the rectum or extend proximally, sometimes involving the entire colon. Rarely, it involves most of the large bowel at once.
The inflammation caused by ulcerative colitis affects the mucosa and submucosa, and there is a sharp border between normal and affected tissue. Only in severe disease is the muscularis involved. Early in the disease, the mucous membrane is erythematous, finely granular, and friable, with loss of the normal vascular pattern and often with scattered hemorrhagic areas. Large mucosal ulcers with copious purulent exudate characterize severe disease. Islands of relatively normal or hyperplastic inflammatory mucosa project above areas of ulcerated mucosa. Fistulas and abscesses do not occur.
Recommended Reading: How To Test For Ulcerative Colitis
What Are Dosages Of Loperamide
Adult and pediatric dosage
Acute Diarrhea
Adult dosage
- 4 mg initially, then 2 mg after each loose stool not to exceed 16 mg/day discontinue if no improvement seen within 48 hours
Pediatric dosage
- 2-6 years : 1 mg every 8 hours orally
- 6-8 years : 2 mg every 12 hours orally
- 8-12 years : 2 mg every 8 hours orally
Second & Subsequent Doses
- 0.1 mg/kg orally after each loose stool not to exceed the dose recommended for first 24 hours
Chronic Diarrhea
Adult dosage
- 4 mg initially, then 2 mg after each loose stool until controlled, and then 4-8 mg/day in divided doses
Pediatric dosage
- 0.08-0.24 mg/kg/day orally divided every 12 hours
Travelers Diarrhea
Adult dosage
- 4 mg after first loose stool, then 2 mg after each subsequent stool not to exceed 8 mg/day
Pediatric dosage
- Children younger than 6 years of age: Safety and efficacy not established
- Children 6-8 years: 2 mg after first loose stool, then 1 mg after each subsequent stool not to exceed 4 mg/day
- Children 8-12 years: 2 mg after first loose stool, then 1 mg after each subsequent stool not to exceed 6 mg/day
- Children 12 years or older: 4 mg after first loose stool, then 2 mg after each subsequent stool not to exceed 8 mg/day
Dosage Considerations Should be Given as Follows:
- See Dosages.
Managing Ulcerative Colitis Flares: The Most Important Step
The key to managing an ulcerative colitis flare is to get a confirmed diagnosis and begin treatment as soon as possible. But doing so can be tricky, because people with the condition may attribute their symptoms to other GI problems, says Oriana Mazorra Damas, MD, an assistant professor of gastroenterology at the University of Miami Miller School of Medicine in Miami.
The goal for remission is to feel well enough that you forget that you have the condition for most of the day in other words, you experience few, if any, symptoms, Dr. Damas explains.
Don’t Miss: Natural Supplements For Ulcerative Colitis
Strategies For The Care Of Adults Hospitalized For Active Ulcerative Colitis
- Suresh PolaAffiliationsInflammatory Bowel Disease Center, Division of Gastroenterology, University of California San Diego Health System, La Jolla, California
- Derek PatelCorrespondenceReprint requests Address requests for reprints to: Derek R. Patel, MD, Division of Gastroenterology, University of California San Diego Health System, 200 W Arbor Drive, MC 8413, San Diego, California 92103-8413. fax: 543-7731AffiliationsInflammatory Bowel Disease Center, Division of Gastroenterology, University of California San Diego Health System, La Jolla, California
- Jesus RiveraNievesAffiliationsInflammatory Bowel Disease Center, Division of Gastroenterology, University of California San Diego Health System, La Jolla, CaliforniaVA San Diego Healthcare System, San Diego, California
- John T. ChangAffiliationsInflammatory Bowel Disease Center, Division of Gastroenterology, University of California San Diego Health System, La Jolla, CaliforniaVA San Diego Healthcare System, San Diego, California
- Elisabeth EvansAffiliationsInflammatory Bowel Disease Center, Division of Gastroenterology, University of California San Diego Health System, La Jolla, California
- Michael DochertyAffiliationsInflammatory Bowel Disease Center, Division of Gastroenterology, University of California San Diego Health System, La Jolla, California
- William J. SandbornAffiliationsInflammatory Bowel Disease Center, Division of Gastroenterology, University of California San Diego Health System, La Jolla, California
Which Factors Increase The Risk For Toxic Megacolon
Often, triggering or predisposing factors can be identified. Signs and symptoms of acute colitis may be present for as long as 1 week before dilatation develops. Although the risk of toxic megacolon increases with the severity of the colitis, rapid tapering or abrupt discontinuation of medications such as steroids, sulfasalazine, and 5-aminosalicylic acid may precipitate toxemia and dilatation.
Medications that negatively impact bowel motility are also implicated in the development of toxic megacolon. These include, but are not limited to, anticholinergics, antidepressants, loperamide, atropine, and opioids. Procedures such as barium enema or colonoscopy may cause distention, impair blood supply, or exacerbate a microperforation and cause subsequent toxemia.
A retrospective study by Tschudin-Sutter et al indicated that the incidence of toxic megacolon is higher in pediatric patients with communityassociated, rather than healthcare facilityassociated, C difficile infection. The study involved 202 pediatric patients with C difficile infection, including 38 with communityassociated infection, 144 with healthcare facilityassociated infection, and 20 with an indeterminate source of infection. Compared with the healthcare facilityassociated group, children with a communityassociated infection had a higher rate not only of toxic megacolon but also of toxic shock and recurrence.
Read Also: How To Check A Horse For Ulcers
Prognosis For Ulcerative Colitis
Usually, ulcerative colitis is chronic with repeated exacerbations and remissions. In about 10% of patients, an initial attack becomes fulminant with massive hemorrhage, perforation, or sepsis and toxemia. Complete recovery after a single attack occurs in another 10%.
Patients with localized ulcerative proctitis have the best prognosis. Severe systemic manifestations, toxic complications, and malignant degeneration are unlikely, and late extension of the disease occurs in only about 20 to 30%. Surgery is rarely required, and life expectancy is normal. The symptoms, however, may prove stubborn and refractory. Moreover, because extensive ulcerative colitis may begin in the rectum and spread proximally, proctitis should not be considered localized until it has been observed for ⥠6 months. Localized disease that later extends is often more severe and more refractory to therapy.
Imodium Classic 2 Mg Capsules
Summary of Product Characteristics Updated 24-Jan-2020 | McNeil Products Ltd
Imodium Classic 2 mg Capsules.
Each capsule contains 2 mg Loperamide hydrochloride.
Excipient with known effect: lactose
For a full list of excipients, see section 6.1
Capsule, hard.
Opaque green cap and grey body, hard gelatin capsule imprinted with ‘Imodium’ on cap and ‘Janssen’ on body containing white powder.
For the symptomatic treatment of acute diarrhoea in adults and children aged 12 years and over.
For the symptomatic treatment of acute episodes of diarrhoea associated with Irritable Bowel Syndrome in adults aged 18 years and over following initial diagnosis by a doctor.
Posology:
ACUTE DIARRHOEA
Adults and children over 12:
Two capsules initially, followed by one capsule after each loose stool. The usual dose is 3-4 capsules a day. The total daily dose should not exceed 6 capsules .
SYMPTOMATIC TREATMENT OF ACUTE EPISODES OF DIARRHOEA ASSOCIATED WITH IRRITABLE BOWEL SYNDROME IN ADULTS AGED 18 YEARS AND OVER
Two capsules to be taken initially, followed by 1 capsule after every loose stool, or as previously advised by your doctor. The maximum daily dose should not exceed 6 capsules .
Paediatric population
Imodium is contraindicated in children less than 12 years of age.
Elderly
No dose adjustment is required for the elderly.
Renal impairment
No dose adjustment is required for patients with renal impairment.
Hepatic impairment
Method of administration
in children less than 12 years of age.
Recommended Reading: List Of Foods Good For Ulcers
What Are Side Effects Associated With Using Loperamide
Common side effects of Loperamide include:
- red or purple skin rash that spreads and causes blistering and peeling,
- diarrhea that is watery or bloody,
Rare side effects of Loperamide include:
- none
This is not a complete list of side effects and other serious side effects or health problems may occur as a result of the use of this drug. Call your doctor for medical advice about serious side effects or adverse reactions. You may report side effects or health problems to FDA at 1-800-FDA-1088.
Treatment Of Ulcerative Colitis
If fulminant or toxic colitis is suspected, the patient should
-
Stop all antidiarrheal drugs
-
Take nothing by mouth and have inserted a long intestinal tube attached to intermittent suction
-
Receive aggressive IV fluid and electrolyte therapy with 0.9% sodium chloride, and potassium chloride and blood as needed
-
Receive high-dose IV corticosteroids or cyclosporine
-
Receive antibiotics
-
Perhaps receive infliximab
Having the patient roll over in bed from the supine to prone position every 2 to 3 hours may help redistribute colonic gas and prevent progressive distention. Insertion of a soft rectal tube may also be helpful but must be done with extreme caution to avoid bowel perforation. Even if decompression of a dilated colon is achieved, the patient is not out of danger unless the underlying inflammatory process is controlled otherwise, colectomy will still be necessary.
If intensive medical measures do not produce definite improvement within 24 to 48 hours, immediate surgery is required or the patient may die of sepsis caused by bacterial translocation or even perforation.
Don’t Miss: Foods That Irritate Stomach Ulcers
Symptoms And Signs Of Ulcerative Colitis
Patients typically have
-
Attacks of bloody diarrhea of varied intensity and duration interspersed with asymptomatic intervals
Usually an attack begins insidiously, with increased urgency to defecate, mild lower abdominal cramps, and blood and mucus in the stools. Some cases develop after an infection .
When ulceration is confined to the rectosigmoid, the stool may be normal or hard and dry, but rectal discharges of mucus loaded with red and white blood cells accompany or occur between bowel movements. Systemic symptoms are absent or mild.
If ulceration extends proximally, stools become looser and the patient may have > 10 bowel movements per day, often with severe cramps and distressing rectal tenesmus, without respite at night. The stools may be watery or contain mucus and frequently consist almost entirely of blood and pus.
Toxic or fulminant colitis manifests initially with sudden violent diarrhea, fever to 40° C , abdominal pain, signs of peritonitis , and profound toxemia.
Are Your Ulcerative Colitis Symptoms Under Control
She emphasizes that your doctor will likely be just as focused on ensuring your treatment also leads to endoscopic remission and histologic/deep remission .
Studies show that those who are in endoscopic and deep remission do best long term, as far as lower chances of hospitalizations for flare-ups and lower chances of complications, including surgery, she says.
Still, your doctor will also recommend that when you do feel your digestion is off that you recognize it and react as quickly as possible.
Pay extra attention if you are exposed to any potential ulcerative colitis triggers. For example, some common medications may prompt flares. The two biggest culprits are antibiotics and nonsteroidal anti-inflammatory drugs , such as ibuprofen, aspirin, and naproxen. Other triggers may include stress and foods that aggravated your symptoms in the past.
Don’t Miss: Causes Of Ulcers In Horses
Pregnancy And Breast Feeding
Loperamide is not recommended in the United Kingdom for use during pregnancy or by nursing mothers. In the U.S., loperamide is classified by the U.S. Food and Drug Administration as pregnancy category C. Studies in rat models have shown no teratogenicity, but sufficient studies in humans have not been conducted. One controlled, prospective study of 89 women exposed to loperamide during their first trimester of pregnancy showed no increased risk of malformations. This, however, was only one study with a small sample size. Loperamide can be present in breast milk, and is not recommended for breast-feeding mothers.
Antiperistaltic Agents Toxic Megacolon
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Inflammatory Bowel Disease
References
Also Check: Signs Of Having An Ulcer
More Tips To Ease Ulcerative Colitis Symptoms
The best way to shorten a flare, of course, is to get treated by your doctor. But there are steps you can take at home too.
When you have a flare, try to follow a low-residue diet for several weeks, Damas says. The goal is to let the colon rest by avoiding fiber. That means staying away from seeds, nuts, fresh fruit, dried fruit, raw vegetables, whole grain bread and cereal, and tough meat.
Were learning more now about the influence that diet can have on control of inflammation, Damas notes. When patients are having an acute flare, its important in the short term to have a low-fiber diet. Many times, for a short period of time, until the flare-up is controlled, we recommend whats called a low FODMAP diet. However, this diet is not recommended long term, because it has no impact on inflammation itself and only on control of symptoms.
Indeed, once youre in remission, Damas says your doctor will likely recommend reintroducing fruits and vegetables as tolerated. Its better to cook vegetables without the skin and consume no more than 2 cups of milk a day.
If youre lactose intolerant, be sure you choose lactose-free dairy products. Its also a good idea to cut down on fat during this time to prevent bulky stools. Avoid other potential triggers, too, such as spicy foods.
Additionally, we recommend patients avoid eating processed foods, as well as those high in fat and animal protein, as these have been associated with inflammation in some studies, Damas says.