When To See A Doctor
Its a good idea to see a doc on the reg to help monitor and manage your UC. Regularly monitoring your UC symptoms, flares and triggers with a doctor can help you identify patterns that help you determine the best mode of treatment.
But in rare cases, you might need medical intervention ASAP. Head to the doctor right away in the instance of:
Even On Good Days Take Your Meds
It can be easy to forget to take your medicines when you feel good. Or you might think its OK to skip them because you feel fine. But you need to stick with the plan your doctor prescribed to keep up those benefits.
You and your doctor will work together to decide if you need to stay on medicines to control your UC. The type of medicine will depend on how severe your UC is.
Warning Signs Of Ulcerative Colitis Flare Up
Flares come up suddenly and are acute very often. For some, it lasts from days to weeks. Between the flare-ups, one may experience a remission period which can also last from days to weeks.
Symptoms of flare differ depending upon the severity and the location of the inflammation. The most common flare-up symptoms include:
- Abdominal pain or cramp
- Loss of appetite
You May Like: Triderma Diabetic Ulcer Defense Healing Cream
Is It Possible For Ulcerative Colitis To Cause Bloating
There has yet to be a lot of study regarding whether UC may induce bloating. However, according to 2016 research, patients with inflammatory bowel disease have considerably higher levels of bloating, gas, and stomach pain than the general population.
Bloating is not the same as gaining weight.
Weight increases happen over time when you consume more calories than
9 Healthy Habits That Could Prevent Ulcerative Colitis
8 Tips to Reset Your Gut
Trust Your Gut: 7 Signs That You Need a Gastroenterologist
21 Things to do During a UC Flare-up
Tips & Tricks You Need To Help Gain And Maintain Weight
What Causes Ulcerative Colitis Flare Ups In The First Place
The experts arent exactly sure what causes UC, but they think its prob an autoimmune condition. Autoimmune conditions are basically what happens when the bodys defense mechanism is a little overzealous and attacks healthy tissue. Your body *means* well, but it causes inflammation.
In the case of UC, scientists think that the immune system might accidentally mistake perfectly harmless bacteria in the colon for serious threats, which causes the whole region to essentially swell up.
Though they dont know exactly what contributes to flare ups, a few possibilities include:
- Stress. According to 2016 research, being stressed out may trigger IBD flare-ups. Even though stress doesnt seem to directly cause UC, it does appear to weaken the intestinal wall and make it more vulnerable to issues. Researchers found that stress increased microbe activity in the colon and hindered the immune response.
- Diet. In a 2020 review, researchers found a correlation between diet and UC flare-ups. However, the research on exactly what triggers them just isnt there yet.
- Certain medications. Abruptly stopping medications like steroids or maintenance therapies, which slow the bods natural cortisol levels, can lead to flares and other negative side effects. Always talk to a doc before halting these drugs.
- Hormonal changes. There seems to be a link between IBD and hormonal changes in women, with some research from 2018 suggesting that UC symptoms worsen during pregnancy in particular.
Don’t Miss: Signs Of Ulcerative Colitis Flare Up
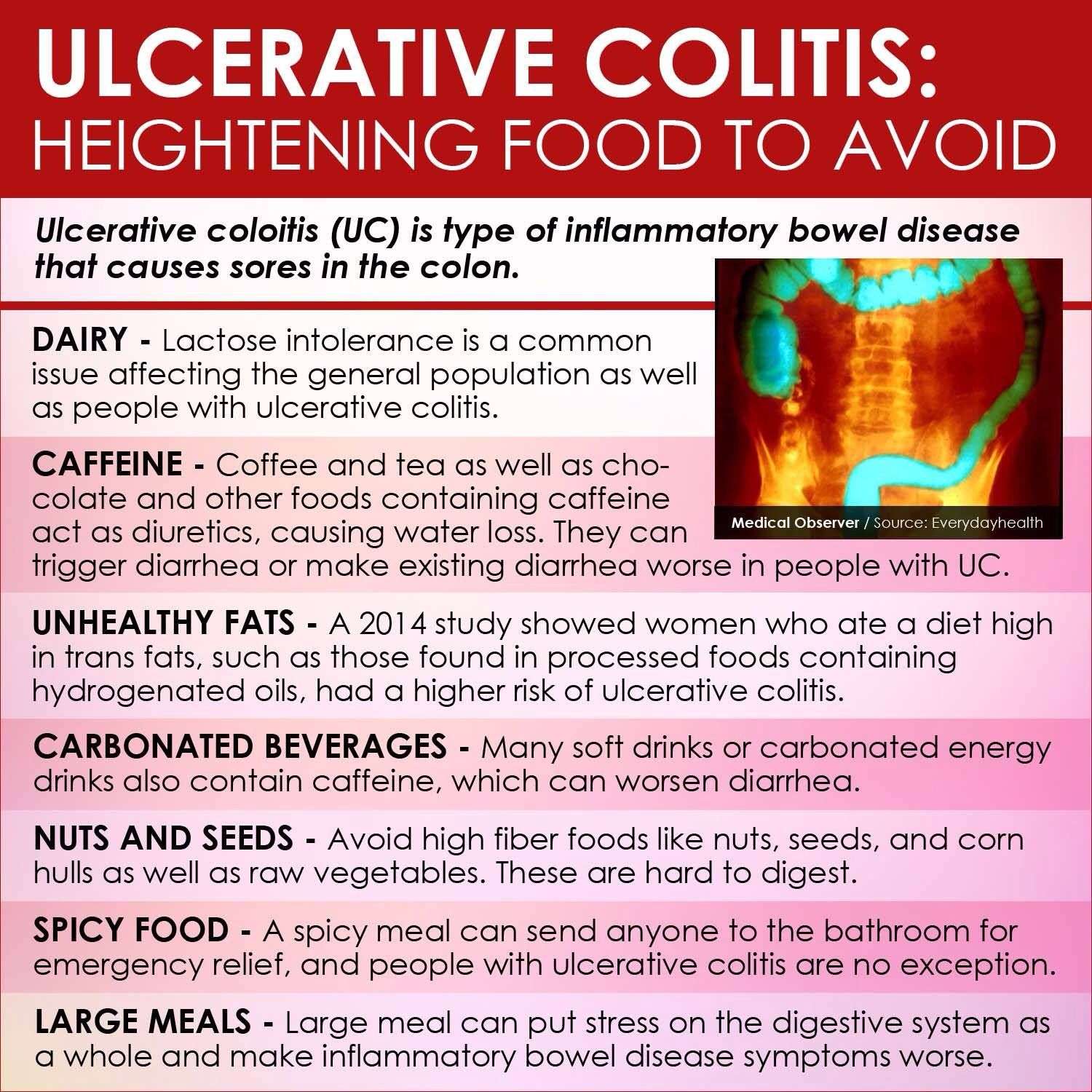
Limit Your Fiber Intake
Fiber contributes to bowel regularity and bowel health, but too much fiber can also be hard to digest and may worsen UC flare-ups.
During a flare-up, try to stick to foods that have no more than 2 grams of fiber per serving. Low fiber foods can include:
- refined carbohydrates like white rice, white pasta, and white bread
- some cooked fruits
- juice with no pulp
Instead of eating raw vegetables, steam, bake, or roast your vegetables. Cooking vegetables results in some fiber loss.
Note that during periods of remission, the Crohns & Colitis Foundation recommends eating a diet with fiber to support general health and nutrition unless advised by a doctor not to do so.
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
Don’t Miss: Can Ulcerative Colitis Cause Erectile Dysfunction
What Are Ulcerative Colitis Flare
Ulcerative colitis is a condition which affects thousands of people across the UK. Luckily, many people with ulcerative colitis flare-ups receive advice and treatment, meaning the condition has minimal impact on their quality of life.
This doesnt mean flare-ups are completely avoidable though. Depending on whether you have proctitis, distal or total colitis, a flare-up may have different effects on the individual. Knowing how to recognise and manage these effects is very important.
In this short blog post, we will discuss what happens during a flare-up and how best to alleviate problems when it does.
Also Check: Wound Care For Stage 4 Pressure Ulcer
Try Having Small Frequent Meals
Smaller portions consumed at more frequent intervals throughout the day are often better tolerated by the gut. Also, small, frequent meals can maximize nutritional intake as it provides you with more opportunities to fit in nutrient-dense foods throughout the day.
I just want to be clear here, Im not recommending less food overall in a day. But eating regularly and dividing up overall intake into 4-6 mini meals can help with symptom management during a flare.
You May Like: How To Heal A Bleeding Ulcer
Rice Water To Fight Ulcerative Colitis
One cup of rice water as soon as you wake up and another before bed will help control ulcerative colitis and its symptoms.
Ingredients
Preparing this drink is very simple.
Dont Miss: Difference Between Ulcerative Colitis And Crohns Disease Ppt
How Is It Evaluated And Diagnosed
Your health care provider will evaluate rectal bleeding by asking questions, performing a physical exam, and doing some tests.
Your provider may ask questions such as:3,4,8
- What are your bowel movements like?
- Have you had any recent changes in bowel habits?
- Are your stools black or bloody? How often does this happen?
- Have you noticed blood on the toilet paper?
- Have you vomited recently? What did it look like?
- Have you had a recent colonoscopy?
- Have you had any recent trauma to the abdomen or rectum?
- What medications are you taking?
- Do you have a history of digestive or blood diseases?
- Have you been treated for prostate or pelvic cancer?
- Has anyone in your family had colon cancer?
- Have you experienced changes in weight recently?
Your health care provider may want to look at your stool.4 If you are in the hospital, you may be asked to use a special toilet or bedpan. If you are at home, your provider will instruct you on how to collect a sample.
Recommended Reading: Generic Drugs For Ulcerative Colitis
Don’t Miss: Wound Dressing For Stage 2 Pressure Ulcer
Make Time For Activities That Make You Happy
Tip number three to help you prevent an ulcerative colitis flare-up: Always make time for things that make you happy. For me, its dancing. I have been taking dance classes since my pre-school years and continues to do so to this day. Its wonderful exercise, I have met amazing friends through this hobby, and it is also my favourite form of exercise. When I am in the dance studio, I forget about everything else in the world and focus on being in the present. So, whether it be dance, a sport that you love, or something as beautiful as painting, make time to feed your hobbies with your time and hopefully you will feel more fulfilled and less stressed!
Put Together An Emergency Kit
Having an emergency kit is important as it can help you avoid embarrassing situations, especially when you are at work or school. You can include items such as underwear, pants, deodorizer, and baby wipes in this kit to help you in most situations.
You may never use this kit, but just having it may bring some mental relief, which can help reduce overall stress and pain levels.
Ulcerative colitis pain is a complex disorder. What techniques or strategies do you use to manage ulcerative colitis pain when a flare-up happens?
Dont Miss: Fish Oil And Ulcerative Colitis
Read Also: Icd 10 Code Sacral Decubitus Ulcer
Who Shouldnt Take Mesalamine
Mesalamine may not be safe if you have certain medical conditions, including:
- An allergy to aspirin or sulfasalazine
- Heart, liver, or kidney disease
- A blockage in your stomach or intestines
- Swelling of the heart muscle, called myocarditis
- Swelling of the sac around the heart, called pericarditis
- Skin problems like eczema or atopic dermatitis
Mesalamine may cause more liver, kidney, and heart risks in older adults. Your doctor might need to adjust the dose to prevent these problems.
Youll need to avoid Apriso if you have the inherited condition phenylketonuria . This medicine contains the artificial sweetener aspartame, which people with PKU must avoid.
Let your doctor know if youre pregnant, you could become pregnant, or youre breastfeeding. There havent been enough studies to show that mesalamine is safe to take during pregnancy. You can safely use this medicine while you breastfeed, but let your doctor know if your baby has diarrhea or other side effects.
How To Prevent Ulcerative Colitis Flare
What are actionable steps you can take to make your symptom-free stretches last as long as possible? and stress management are probably the two biggest things as far as prevention goes, says Cohen. Parsley Health providers and health coaches often work with members who have ulcerative colitis to find a diet that helps them minimize flares and a stress management routine. Below, well dive into some specific ways to optimize your diet with natural remedies and make adjustments to your lifestyle while living with ulcerative colitis.
Dont Miss: Do Ulcers Make You Throw Up
Read Also: Fruits Good For Ulcerative Colitis
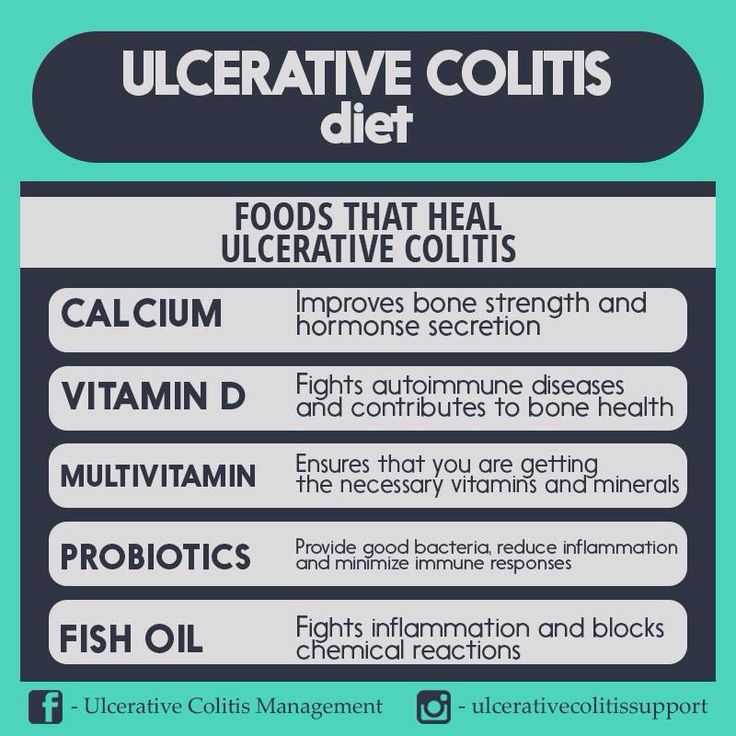
Tap Into ‘good’ Bacteria
Antibiotics can trigger flares. If your UC gets worse while you take them, tell your doctor. Some scientists think antibiotics cause issues because they kill “good” bacteria in your gut that aid digestion. Although research is limited, there is some evidence that probiotics, which contain these bacteria, along with other medications may be helpful, but this has not been proved.
12
Some flare symptoms are very serious. Get medical help right away if you have:
- Constant, heavy diarrhea
- New or more blood in your stool, or any blood clots
Also get help if you feel like you’re going to faint or you vomit over and over.
13
Limit Intake Of Animal Products
Especially meats/red meats. I have read in many articles that because many people have low stomach acidity and poor digestion, meats tend to rot in our guts, thus producing pus and contributing to inflammation . This rotting can produce more intestinal gas and overall slower digestion. I personally try to limit my meat intake to 1-2 meals per week !
Also Check: Patient Education On Pressure Ulcer Prevention
Number : Follow An Elimination Diet & Test Each New Food
This should be where you start.
The food list should be small initially.
It should comprise no more than 3-5 foods and should also be very minimal on the supplement front.
Yes, 3-5 foods is very limited, but thats the whole point.
This is so that your immune system does not have many potential triggers to react to.
And so that as you gradually introduce foods, you can work out what your triggers are.
Pick nutrient dense foods and/or add a multi-vitamin in the beginning to avoid any nutrient deficiencies.
There are many types of elimination diet.
Some of the main ones that people will use to stop an ulcerative colitis flare up are:
- A carnivore diet
Ive used all of these with my clients with good success.
There are others, of course, but these are the main ones.
As far as which specific foods to consume, stating the obvious, I cannot be more specific without knowing the dependences listed in the section above.
That being said, for the testing:
1. Consume 1 x serving of the new food you are testing once per day for 4 days.
Only test 1 new food at a time.
Be sensible with serving sizes if you are unclear on what a sensible serving size is, eat 0.5-0.75 cups of the specific food.
You can increase the serving size over time.
The new food can be consumed with other foods that youve already tested and marked as safe.
Which foods to test and in which order is dependent on your
- dietary preferences
Dont Skip Your Medication
If you already have prescription medication for colitis, take your medication as prescribed. Dont skip your medicine, even if you feel better.
If you need help remembering to take your medication, use a reminder on your phone and/or set a sticky note on your keys
Sticking with your medication schedule can help you stay in remission and avoid a flare-up.
You May Like: Stelara Dosing For Ulcerative Colitis
What To Do When Ulcerative Colitis Flares
Almost half of IBD patients have at least one flare a year.
This can have a huge impact on their physical and emotional wellbeing. For the NHS, the major impact is financial as its 2-3 times more expensive to treat a patient with active disease compared to someone in remission.
When someone has a flare, the GP is often their first port of call. But 52% of GPs say they are less than confident or not confident if an IBD patient comes to their clinic with a flare-up1.
This is why flare pathways are so important. Co-produced by a working group of health professionals and patients as part of the RCGP and Crohns & Colitis UKIBD Spotlight Project, and approved by the British Society of Gastroenterology, they give primary care health professionals accessible guidance on steroid intervention, dose escalation, and when to refer to secondary care.
With these pathways, suitable patients can be managed appropriately. This means better and more confidence in responding to flares effectively, including rapid access to advice from the IBD team.
What Is A Uc Flare
A UC flare is an acute worsening of the symptoms of bowel inflammation. Flares may occur weeks, months, or even years apart, with different levels of severity.
Medication, your lifestyle, diet, and other factors may contribute to flare-ups. In the same way, taking all prescribed medications, eating balanced meals, and avoiding known triggers can often help prevent flares.
Ulcerative colitis symptoms change based on the severity of a flare-up and the location of inflammation in the intestine. Symptoms often include:
- moderate to severe abdominal pain or cramps
- persistent bowel movements
Also Check: Signs A Horse Has Ulcers
Is Ketchup Okay For Ulcerative Colitis
The answer to the question of whether ketchup is okay for people with ulcerative colitis is not a straightforward yes or no. Ketchup is high in acidity and contains ingredients like vinegar, sugar, and sodium, which may be problematic for those suffering from ulcerative colitis. It is important to consult with a medical professional before adding ketchup to a diet for someone with ulcerative colitis. Additionally, it is important to read the label of any ketchup product to check for any added ingredients that may exacerbate symptoms. If it is deemed safe to consume, it is likely best to limit the consumption of ketchup due to its high levels of acid.
Certain foods have been shown in studies to be beneficial to people who suffer from lactose intolerance. Hard cheeses, such as cheddar, parmesan, and other cheeses, are an excellent example of this because they contain a low amount of lactose the milk sugar that can cause abdominal pain and bloating in those who are sensitive to it. Furthermore, human endothelial cells have been shown to exhibit anti-inflammatory properties, as have tomato ketchups antioxidants, which include -tocopherol, ascorbic acid, and lycopene. Despite the fact that those on a restricted diet may find it difficult to consume certain foods, the benefits of these foods are obvious.
Common Treatments For Ulcerative Colitis
Ulcerative colitis canât be cured, but you can usually manage the symptoms through diet, medication and/or surgery. Your consultant will discuss options with you, based on your symptoms and the extent of your bowel inflammation.
During a very severe flare-up, you may require hospital treatment as an in-patient.
Diet
Making small changes to your daily diet may relieve your symptoms. Try:
- Changing from three daily main meals to five or six small meals every day
- Drinking lots of water
- Avoiding caffeine, alcohol and fizzy drinks
Also, your consultant may recommend taking food supplements to replace nutrients lost as a result of frequent diarrhoea. You may also be referred to a dietitian, wholl help you follow an ulcerative colitis diet plan.
Medication
To prevent symptoms recurring or relieve symptoms during a flare-up, your consultant may prescribe:
- Immunosuppressants
- Aminosalicylates or steroids â to reduce inflammation
- Monoclonal antibodies â drugs which target specific cells
Surgery
If ulcerative colitis is affecting your daily life and other treatments are unsuccessful, your consultant may suggest surgery. In most cases, this involves removing your large bowel so that waste is passed out of your small intestine instead. This requires either:
- An ileostomy an opening in your abdomen for your small intestine to drain into an external pouch
Don’t Miss: How Many People Have Ulcerative Colitis