How To Prevent Pressure Ulcers Or Bed Sores
Pressure ulcers are a common problem in palliative care patients. Decreased mobility, increased time spent in bed, and altered nutrition make these patients prime targets for skin breakdown. Pressure ulcers are painful. As a caregiver, one of the most important things you can do to keep your patient comfortable is to prevent one from developing.
Also Check: Foods That Cause Stomach Ulcers
Legal And Policy Material
Patients Rights
Australia and New Zealand recognize patients rights. In Australia, those rights are enshrined in the Australian Charter of Healthcare Rights2 . For aged care, the Charter of Care Recipients Rights and Responsibilities: Residential Care 2014 also outlines recipients rights. A key difference between the Australian Charter and the New Zealand Code of Health and Disability Consumers Rights is enforceability. The New Zealand version provides a codified benchmark against which the health complaints entity assesses complaints for potential breaches . By contrast, the Australian Charter is in effect a guide only, is not specifically enforceable, and is not linked to the powers of the health complaints entities . However, Australian patients may complain to the Health Complaints Commissions in the states and territories and/or the Aged Care Commissioner.
Regulation of Aged Care Facilities
In Australia, RACFs are regulated by state and Commonwealth legislation. The main Commonwealth statute is the Aged Care Act 1997 . This Act concerns funding, allocation, licencing of approved providers, rights, and responsibilities. Importantly, it outlines the responsibilities of providers for the quality of care they provide and residents rights. When assessing the quality of care, the Quality of Care Principles 2014 may also be used as a benchmark.
Torts and Crimes
Coronial Jurisdiction
How Should A Comprehensive Skin Assessment Be Conducted
The first step in our clinical pathway is the performance of a comprehensive skin assessment. Prevention should start with this seemingly easy task. However, as with most aspects of pressure ulcer prevention, the consistent correct performance of this task may prove quite difficult.
3.2.1 What is a comprehensive skin assessment?
Comprehensive skin assessment is a process by which the entire skin of every individual is examined for any abnormalities. It requires looking and touching the skin from head to toe, with a particular emphasis over bony prominences.
As the first step in pressure ulcer prevention, comprehensive skin assessment has a number of important goals and functions. These include:
- Identify any pressure ulcers that may be present.
- Assist in risk stratification any patient with an existing pressure ulcer is at risk for additional ulcers.
- Determine whether there are other lesions and skin-related factors predisposing to pressure ulcer development, such as excessively dry skin or moisture-associated skin damage .
- Identify other important skin conditions.
- Provide the data necessary for calculating pressure ulcer incidence and prevalence.
Additional Information
It is important to differentiate MASD from pressure ulcers. The following articles provide useful insights on how to do this:
3.2.2 How is a comprehensive skin assessment performed?
- Temperature.
- Skin integrity .
Tools
Detailed instructions for assessing each of these areas are found in Tools and Resources .
Don’t Miss: Prevention And Treatment Of Pressure Ulcers
What Causes Pressure Injuries
- Continuous pressure builds when you sit or lie on a bony area for too long. Pressure slows or stops the blood from flowing to the skin. This may hurt the skin and cause tissue damage. Pressure can start to cause damage to your skin and tissue about 2 hours after staying in the same position.
- Shearing or friction happens when delicate skin is dragged across a surface, such as sheets. This may cause your skin to tear or a blister to form. Sliding up or down in bed or moving from the bed to a chair may tear your skin. Muscle spasms may cause your arms or legs to jerk and rub the sheets, causing tears in your skin.
Patient Involvement In Medical Device
Education relating to medical devices, splints, and casts tends to be from staff on the unit. This education is most often utilized if a patient is on maternity and has a knee brace. Often, it is the patient who is likely to be more familiar with the device than the nurse. Asking the patient should not be viewed as a problem and is preferable to patient repositioning of the device afterward. Medical device procurement must include staff involvement with medical device purchasing so that company rhetoric and cost are not placed above patient comfort and safety or staff experience and expertise.
Read Also: Foods To Treat Ulcerative Colitis
What Do The Australian Wound Management Associations Official Guidelines Say
Professor Geoff Sussman, Chairman of Wounds Australia, told HelloCare that the Australian Wound Management Associations Pan Pacific Clinical Practice Guideline for the Prevention and Management of Pressure Injury give the evidence based and the most widely accepted guidelines in the region for preventing pressure sores.
The key recommendations for prevention of pressure injuries for those who have been assessed as being at risk of developing them include:
- Add high protein oral nutritional supplements to a regular diet.
- Use a high specification reactive support foam mattress on beds, or active support mattresses as an alternative.
- Reposition patients to reduce the duration and magnitude of pressure over vulnerable areas, including bony prominences and heels.
- Frequency of repositioning will depend on the patients risk of pressure injury development, skin response, comfort, functional level, medical condition, and the support surface used.
Myth #4 Turning Is Easy
This myth gets under my skin more than any other There are many variables and comorbidities that put a person at risk for pressure injury, but peel back the onion layers of any pressure injury incident and somewhere in there you will always find the problem of pressure itself. The patient is first high risk for some reason, then pressure reduction was complicated for one reason or another. A short list of possible problems include the patient was not turned enough, or he/she was difficult to turn, too unstable to turn, refused to be turned, etc. There are so many reasons why turning can be difficult it makes my head spin but suffice to say is a simple concept that is not always easy to do.
Myths about turning may be ubiquitous, but they do not have be limiting. We have come a long way in the science of pressure injury prevention. Once we are able to integrate the nursing process with science and technology, I believe we can stop pressure injuries. As Dr. Joyce Black says The trick is to get the pressure off
REFERENCES
Recommended Reading: Stomach Ulcer And Chest Pain
Risk Factors For Pressure Sores
A pressure sore is caused by constant pressure applied to the skin over a period of time. The skin of older people tends to be thinner and more delicate, which means an older person has an increased risk of developing a pressure sore during a prolonged stay in bed.
Other risk factors for pressure sores include:
- immobility and paralysis for example due to a stroke or a severe head injury
- being restricted to either sitting or lying down
- impaired sensation or impaired ability to respond to pain or discomfort. For example, people with diabetes who experience nerve damage are at increased risk of pressure sores
- urinary and faecal incontinence skin exposed to urine or faeces is more susceptible to irritation and damage
- malnutrition can lead to skin thinning and poor blood supply, meaning that skin is more fragile
- obesity being overweight in combination with, for example, immobility or being restricted to sitting or lying down can place extra pressure on capillaries. This then reduces blood flow to the skin
- circulation disorders leading to reduced blood flow to the skin in some areas
- smoking reduces blood flow to the skin and, in combination with reduced mobility, can lead to pressure sores. The healing of pressure sores is also a slower process for people who smoke.
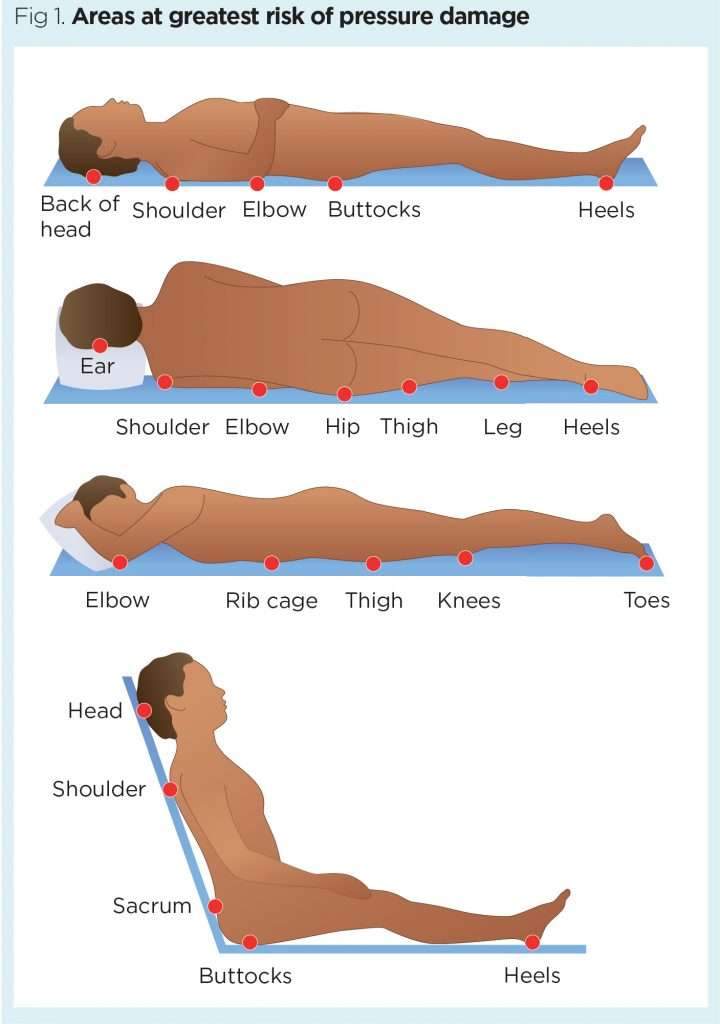
If youre bedridden, pressure sores can occur in a number of areas, including:
- back or sides of the head
- rims of the ears
- backs or sides of the knees
- heels, ankles and toes.
What To Ask To Ensure Compliance While Repositioning Patients At
Pressure injury prevention needs to start before admission and needs to be stressed to the patient at risk on admission when they are positioned appropriately and a preliminary repositioning schedule is set.If there is a delay in getting the correct surface or equipment this can be interpreted as the issue not being important.
Statements to avoid:
- Can I make you comfortable?
- Is it alright to reposition you?
- May I turn you now?
Statements likely to elicit more positive participation from patients regarding repositioning:
At each stage, ask the patient why they do not want to be repositioned to address each issue . Turn their bed a different way, position a blind, move a bedside stand. If you are not getting anywhere, seek advice from the charge nurse or a colleague. Be flexible, but firm and consistent. Remember: patients have choices and can refuse care, but their choices need to be informed choices and their choices must be documented. Part of educating them is their acceptance that what you are saying is believable. The term “pressure injury” is more meaningful than “pressure ulcer” as, to many people, an ulcer is a serious stomach condition. How can they get that from a red patch on their butt? The word “injury” indicates damage that can happen fast and is likely to be understood better. A picture paints a thousand words so plan with their team to show them a photograph of a stage 4 pressure injury. And remember to always DOCUMENT.
You May Like: What To Eat To Cure Ulcer
How Can Pressure Injuries Be Prevented
Ways to prevent pressure injuries include:
Where To Get Help
- Hospital staff
- Domiciliary care staff
- NURSE-ON-CALL Tel. for expert health information and advice
- Ricci JA, Bayer LR, Orgill DP. Evidence-Based Medicine: The Evaluation and Treatment of Pressure Injuries, Plast Reconstr Surg. 2017 Jan 139:275e-286e
- Walia GS, Wong AL, Lo AY, Mackert GA, Carl HM, Pedreira RA, et al. Efficacy of Monitoring Devices in Support of Prevention of Pressure Injuries: Systematic Review and Meta-analysis. Adv Skin Wound Care, 2016 Dec 29:567-574
- Wound, Ostomy and Continence Nurses Society-Wound Guidelines Task Force, WOCN 2016 Guideline for Prevention and Management of Pressure Injuries : An Executive Summary. J Wound Ostomy Continence Nurs. 2017 May/Jun 44:241-246
- Scafide KN, Narayan MC, Arundel L. Bedside Technologies to Enhance the Early Detection of Pressure Injuries: A Systematic Review, J Wound Ostomy Continence Nurs. 2020 Feb 13.
- Munoz N, Posthauer ME, Cereda E, Schols JMGA, Haesler E. The Role of Nutrition for Pressure Injury Prevention and Healing: The 2019 International Clinical Practice Guideline Recommendations. Adv Skin Wound Care, 2020 Mar 33:123-136.
- Qigui X, Qinling Y, Huapeng L. Meta-analysis of effect of foam dressing and hydrocolloid dressing on bedsore management. Chinese Nurs Res. 2017 31:3397-3400.
- Westby MJ, Dumville JC, Soares MO, Stubbs N, Norman G. Dressings and topical agents for treating pressure ulcers. Cochrane Database Syst Rev. 2017 6.
Don’t Miss: How Do You Get Mouth Ulcers
Sample Of Materials Related To Elder Law
We sampled legal and policy materials such as cases, legislation, government reports, guidelines, regulations, and principles that were relevant to aged care and elder abuse. These materials broadly fall into an area of law called elder law. We also included secondary source commentary on the legal and policy documents that we subsequently identified. We reviewed these documents to assess the legal implications of two-hourly repositioning and the use of restraints.
How The Intervention Might Work
Pressure, from lying or sitting on a particular part of the body results in oxygen deprivation to the particular area . Normally, this results in pain and discomfort, which stimulates the person to change position. However, if the person is unable to reposition themselves, or has impaired sensation and therefore does not experience the discomfort, assistance will be required. Repositioning reduces the duration of pressure experienced by the tissues and so decreases tissue hypoxia and consequently the theoretical risk of pressure ulceration .
Negative aspects of frequent repositioning
Whilst frequent repositioning underpins current practice guidelines, it may also be associated with negative consequences for patients, nursing staff and health care . Repositioning can lead to disruption of sleep, particularly sleep fragmentation . In acutely ill people, disruption of sleep can lengthen recovery, suppress immune function and predispose people to infection . A sleep cycle, which has light and deep stages of sleep, occurs about every 90 minutes. Consequently if repositioning is undertaken every two hours, it may result in fragmentation of sleep at a detrimental stage of the sleep cycle .
Other negative effects of repositioning include possible increases in patients pain perception. Although regular movement is important, unnecessary repositioning may cause increased discomfort for people with wounds, stiff joints, bony pain or contractures.
Don’t Miss: Humira Not Working For Ulcerative Colitis
Reduce Friction And Shear
Friction is the rubbing of skin on an external surface, usually bed sheets. Friction to the most commonly affected areas can be reduced with protective devices. Heel and elbow cradles are typically made of egg-crate material and Velcro on.
Skin protecting dressings, such as films and thin hydrocolloid bandages can protect the skin from repeated friction but wont help reduce pressure.
The most important thing you can do to prevent injury from the friction is to make sure you dont create any yourself when youre repositioning your loved one. Use a draw sheet to help you lift your loved one off the bed when you lift and reposition.
Shear is created when the deeper fatty tissues and blood vessels are damaged by a combination of friction and gravity. The best way to avoid this type of injury is to avoid a semi-Fowler and upright position in bed. A semi-fowler position is where the head is raised less than 30 degrees and upright positions more than 30 degrees.
Now, you obviously cant avoid these positions all of the time. Many patients need to be semi-Fowler to help ease shortness of breath or prevent gastric reflux and all patients need to be in an upright position to eat safely.
To minimize the risk of shear injury in a semi-Fowler or upright position, take precautions to prevent your loved one from sliding down in bed. You can do this by raising the foot of the bed and propping the knees up with pillows.
What Bundle Of Best Practices Do We Use
Given the complexity of pressure ulcer prevention, with many different items that need to be completed, thinking about how to implement best practices may be daunting. One approach that has been successfully used is thinking about a care bundle. A care bundle incorporates those best practices that if done in combination are likely to lead to better outcomes. It is a way of taking best practices and tying them together in a systematic way. These specific care practices are among the ones considered most important in achieving the desired outcomes.
The pressure ulcer bundle outlined in this section incorporates three critical components in preventing pressure ulcers:
- Comprehensive skin assessment.
- Standardized pressure ulcer risk assessment.
- Care planning and implementation to address areas of risk.
Because these aspects of care are so important, we describe them in more detail in the subsequent subsections along with helpful clinical hints. While these three components of a bundle are extremely important, your bundle may stress other aspects of care. It should build on existing practices and may need to be tailored to your specific setting. Whatever bundle of recommended practices you select, you will need to take additional steps. We describe strategies to ensure their successful implementation as described in Chapter 4.
The challenge to improving care is how to get these key practices completed on a regular basis.
Resources
Practice Insights
Recommended Reading: Ulcer Signs Symptoms And Treatment
Contact One Of Our Attorneys For Legal Assistance
If you do not live near your loved ones nursing home, it can be harder to capture early signs of substandard care. However, it may help to talk to staff regularly regarding how your loved ones care is being managed. Speak to your loved one by phone often and listen for signs of neglect or something that may be out of the ordinary. Write down and check out anything that seems unusual or concerning.
At PKSD,our Wisconsin nursing home abuse lawyers are prepared to provide legal help if your loved one suffered serious or life-threatening bedsores due to nursing home neglect. Representatives at our firm are available to take your call and schedule your consultation anytime, day or night. If we represent you, there are no costs to pay unless we achieve a recovery on your behalf.
Call PKSD for legal help today:
FREE CASE REVIEW
How Often Do Nursing Home Residents Need To Be Turned
There has been a lot of debate over the years regarding how often a wheelchair-confined or bedridden patient needs to be turned or repositioned to prevent a bed ulcer also called a bedsore or pressure ulcer. According to other medical institutions, including Johns Hopkins and the Mayo Clinic, caregivers should reposition or shift a patient who is bedridden or wheelchair-bound at least once every two hours.
Also Check: How To Treat An Ulcer After Gastric Bypass