Diet Progression Following Flares For Ulcerative Colitis And Crohn’s Disease
- Continue to follow a low residue diet and slowly add back a variety of foods.
- Begin with well-tolerated liquids and advance to soft solids, then solids .
- Introduce one or two items every few days and avoid any foods that cause symptoms.
- Add fiber to diet as tolerated. Well-tolerated fiber sources include tender cooked vegetables, canned or cooked fruits, and starches like cooked cereals and whole wheat noodles and tortillas.
- Between flares, eat a wide variety of foods as tolerated. This includes fruits, vegetables, whole grains, lean protein, and low-fat and nonfat dairy products.
- Increase your calorie and protein intake following a flare. Abdominal pain, diarrhea and decreased appetite may have caused poor food intake. Steroids used to treat flares also can increase protein needs.
Suggestions for first foods after a flare include:
- Diluted juices
Dear Diary: Diet And Ulcerative Colitis
The idea is simple. By recording exactly what you eat over a period of time and how you feel afterward, you can nab particular foods that cause your symptoms to flare up. You’ll also be able to identify foods that soothe your digestive tract.
Make recording your meals convenient for you. Some dietitians recommend using a notebook small enough to carry with you. That way you can jot down what you eat at meals and in between throughout the day. Others say it’s fine to keep a notebook by the side of the bed and record everything you ate that day before going to sleep.
“Most people are pretty good at remembering what they ate over a 24-hour period,” says dietitian Tracie Dalessandro, RD, author of What to Eat with IBD. “I find that filling in the diary just once a day is easier and more convenient for many people than pulling it out after every meal.”
What Is An Ulcerative Colitis Diet
A person with ulcerative colitis may find they need to modify their diet to help manage their symptoms. There is not a single diet or meal plan that fits everyone with ulcerative colitis, and diets are individualized for each patient. Depending on symptoms different types of diets may be recommended, such as:
- A high-calorie diet: Many people with ulcerative colitis lose weight and can develop signs of malnutrition. A high calorie diet may prevent these problems.
- A lactose-free diet: People with ulcerative colitis may also have lactose intolerance.
- A low-fat diet: Ulcerative colitis may interfere with fat absorption and eating fatty foods may trigger symptoms. This is often recommended during an ulcerative colitis flare.
- A low-fiber diet : This can help reduce the frequency of bowel movements and abdominal cramps.
- A low-salt diet: This diet is used when patients are on corticosteroid therapy to help reduce water retention.
- A low FODMAP diet: FODMAPstands for Fermentable Oligo-Di-Monosaccha-rides and Polyols, which are types of sugars found in certain carbohydrates and sugar alcohols. This diet is used in people who have intolerance to FODMAPS.
- A gluten-free diet: People with ulcerative colitis may also be sensitive to gluten.
Read Also: What Foods Are Good To Eat With Ulcerative Colitis
Are Nutritional Needs Different For People With Ibd What Are The Specific Nutritional Needs For People With Crohn’s Disease And Ulcerative Colitis
Nutritional needs are specific to the individual and differ with disease state, body size and age. A nutritionist can help you estimate your individual needs. Calorie and protein needs are similar for Crohn’s disease and ulcerative colitis. In both diseases, needs increase during inflammation and immediately after to restore losses. The following are general statements about nutritional needs that may apply to you.
General Guidelines When Ulcerative Colitis Is In Remission
Some members of MyCrohnsAndColitisTeam find they can eat a wider variety of foods safely during remission periods when ulcerative colitis is not as active and symptoms are absent or mild. Still, every individual is different, and purportedly beneficial foods may trigger symptoms. Trial and tracking is the only way to know for sure.
If it is safe for you, these guidelines may help you stay your healthiest during remission:
- Get 25 grams to 35 grams of fiber per day to promote bowel regularity and reduce inflammation.
- Consume plenty of lean meats, which are a good source of B vitamins. Include fatty fish, tofu, and nut and seed butters.
- Include probiotic foods such as yogurt, tempeh, kefir, kimchi, miso, and sauerkraut.
While some members find kefir too sour for their liking, others report experiencing benefits from trying the fermented drink. Kefir has been helping me over the past week, wrote one. Been trying kefir the past few days. Will keep you posted. So far less pain, said another.
You May Like: Air Mattress For Pressure Ulcer Prevention
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
How Does Pediatric Ulcerative Colitis Affect My Childs Mental/emotional Health
Like many conditions, ulcerative colitis can have a negative psychological effect, especially on children. They can experience physical, emotional, social and family problems. Because of the medications and/or general stress from the situation, your child may experience:
- Mood swings.
- Worry about appearance and physical stamina.
- Vulnerability because their body doesnt function normally.
- Poor concentration.
- Misunderstandings with friends and family.
Children need mutual support from all family members. Its helpful for the entire family to learn about the disease and try to be empathetic. Seek out a psychiatrist and therapist to help your child manage such challenges of their ulcerative colitis.
Also Check: How To Prevent Skin Ulcers
Signs And Symptoms Of Ulcerative Colitis
The most common UC symptom is bloody diarrhea or pus in the stool. Besides, other symptoms include:
- Sudden and frequent need to poop
- Cramping bowel pain
- Canker sores
- Pain or bleeding with bowel movements
Although ulcerative has no cure, knowing what to eat with colitis can effectively mitigate the on-and-off cycle of these symptoms, and can aid in the reduction of inflammation and risk of flare.
Can Elimination Diets Cure It
Up to 60% of IBD patients have tried an elimination diet to relieve ulcerative colitis symptoms .
Unfortunately, the only known cure is total surgical removal of the colon and rectum .
There is no scientific proof that any diet can cause remission on its own. However, limited evidence suggests that certain diets can greatly improve comfort and quality of life.
The impact of diet on inflammatory bowel disease. Click to enlarge. Image .
Read Also: How To Treat Diabetic Ulcers On Toes
Ner With A Licensed Ibd Dietitian For A Healthy Nutritional Diet Plan To Reduce Uc Flare
Do you have IBD but are confused when choosing the best food for ulcerative colitis? Or do you find yourself restricted to just a few foods? It doesnt have to be this way. Working one on one can be a great way to get to symptom reduction faster and reduce the stress of figuring it out on your own.
Partner withCrohns and Colitis Dietitians today and get professional help creating a nutritional therapy plan to help reduce the symptoms of ulcerative colitis.Contact us today at 306-7517 orget started on your nutritional plan by booking a consultation.
Resources:
Living With Uc: Probiotics
Probiotics consist of bacteria that confer a health benefit on the person who ingests them. In general, they are bacteria that are normally found in the human intestine. Probiotics have beneficial effects in several medical conditions. Studies have shown that probiotics help people with ulcerative colitis maintain their remissions. Probiotics are found in yogurts and some other foods, but the probiotics that have been studied and found to be effective are sold separately as supplements and are not food products. The effects of probiotics vary greatly and depend on the exact bacteria that are present. Therefore, it is likely that many probiotics that are sold have no beneficial effect, and, therefore, the one that is used for treatment needs to be chosen carefully on the basis of scientific studies.
You May Like: Ulcerative Colitis And Canker Sores
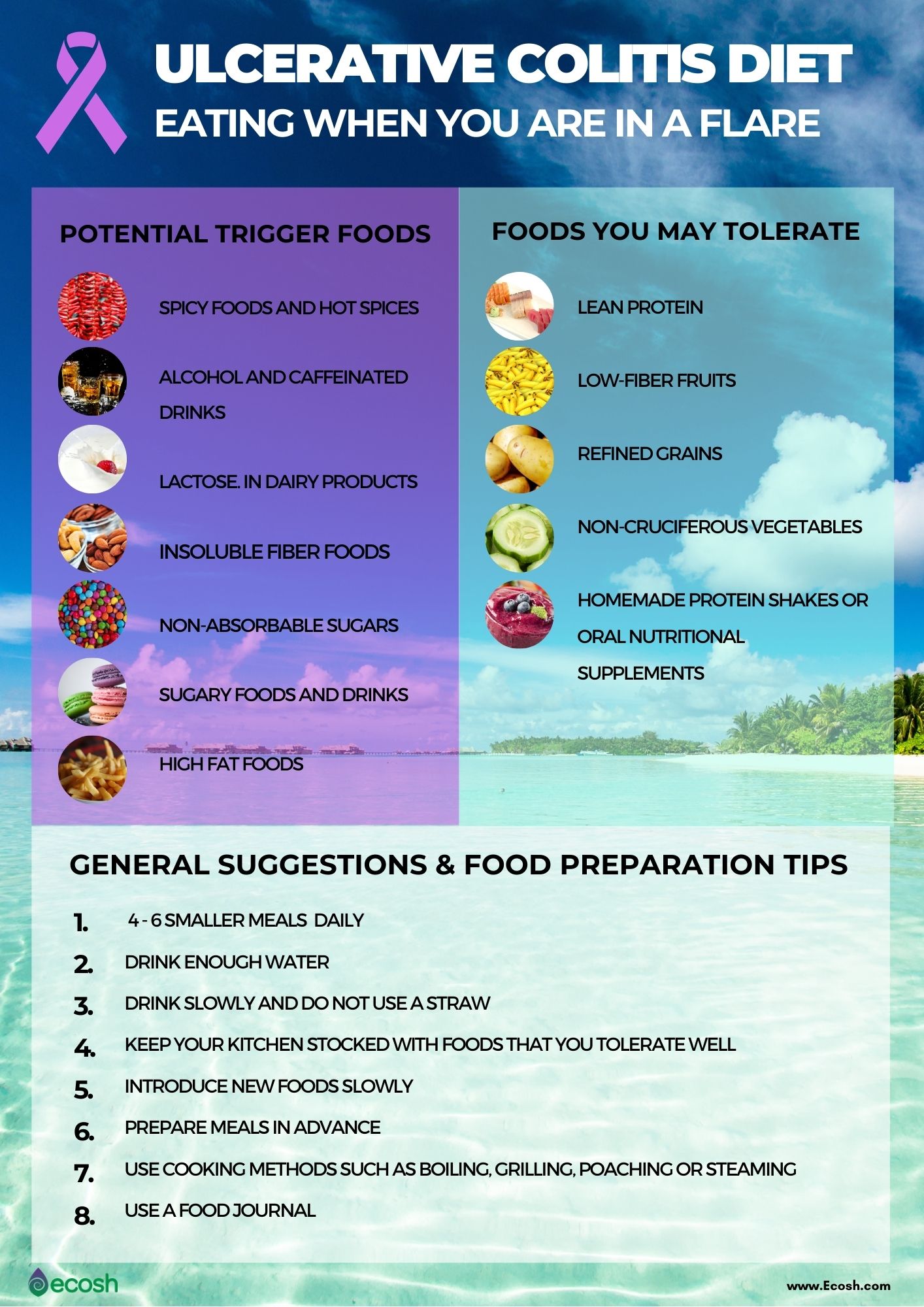
Food Preparation And Meal Planning
While there is no one-size-fits-all for meal planning, these tips can help guide you toward better daily nutrition:
-
Eat four to six small meals daily.
-
Stay hydrated drink enough to keep your urine light yellow to clear with water, broth, tomato juice, or a rehydration solution.
-
Drink slowly and avoid using a straw, which can cause you to ingest air, which may cause gas.
-
Prepare meals in advance, and keep your kitchen stocked with foods that you tolerate well .
-
Use simple cooking techniques boil, grill, steam, poach.
-
Use a food journal to keep track of what you eat and any symptoms you may experience.
Carbonated Beverages May Increase Abdominal Pain

Fizzy drinks may cause gas or bloating in some people, possibly leading to increased abdominal discomfort. Many soft drinks or carbonated energy drinks also contain caffeine, which can stimulate the intestines and worsen diarrhea, according to Mayo Clinic. Drinking sugary soft drinks can contribute to obesity as well, which raises the risk of heart disease and other health problems.
An analysis of drinks published in May 2019 in the journal Medicine found that a high intake of soft drinks was associated with an increased risk of developing Crohns disease, while a high intake of tea was associated with a lower risk of the inflammatory bowel disease. For a refreshing beverage, choose fruit-infused water or herbal iced teas.
Read Also: How To Prevent Decubitus Ulcers
How Should I Begin To Find The Right Diet For My Ulcerative Colitis
Ulcerative colitis is a difficult condition to live with. Curing it is impossible: You can only hope to manage it to the best of your ability. Doctors advise eating foods that help to calm down your symptoms, so you should pay attention to what you eat and simultaneously avoid “bad” foods that aggravate your ulcerative colitis.
The food you eat is crucial to your nutrition and wellbeing. People with inflammatory bowel disease are frequently malnourished, and this is because ulcerative colitis often causes:
- Limited absorption of proteins, fats, carbohydrates, water, vitamins, and minerals
- Loss of the urge to eat
- Unintentional weight loss
- More significant nutritional needs due to the disease
Because of this, you must eat a diet that helps manage your ulcerative colitis and contains many nutrients. No one diet works for everyone that has this condition. The best way to figure out what works for you is by keeping a food journal.
To do this, you should write down what you eat every day. Then, write down all of your symptoms and their severity. From this, you will be able to tell which foods trigger or worsen your ulcerative colitis.
Be sure to never eliminate a whole food group at once, as this can often lead to a lessening of vital nutrients. Additionally, try to only add in types of food one at a time so that you can understand their impact on your body.
Are Food Triggers The Only Cause Of An Ulcerative Colitis Flare
Regardless of your diet, there may be times when your ulcerative colitis symptoms seem to disappear completely for months at a time before making a dramatic reappearance. When this happens, its .
But the foods youre eating arent the only possible culprit. Emotional stress, not taking medications as prescribed, and use of certain medications, like steroids and antibiotics, can also trigger ulcerative colitis flares, according to the Cleveland Clinic.
Flares take different forms for different people, and theres no formula that predicts what will bring them on. Different people will claim a medicine or anxiety will set their symptoms off. But some people just seem to have had flares when they have flares, and you can drive yourself crazy trying to find the cause, Dr. Schwimmer says.
Also Check: How To Get Remission In Ulcerative Colitis
What Foods Trigger Colitis
Ulcerative colitis is a chronic type of inflammation in the bowel. Today, about 750,000 people in the U.S. are living with this disease. To improve this potentially debilitating condition, colitis sufferers must closely watch their food consumption to help maintain a healthier colon and avoid triggering a disease flare-up. This article will help you understand colitis and how to avoid symptoms by changing what you eat.
What Are The Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms often get worse over time. In the beginning, you may notice:
- Diarrhea or urgent bowel movements.
- Abdominal cramping.
- Liver disease.
- Loss of fluids and nutrients.
Symptoms are similar in pediatric ulcerative colitis and may also include delayed or poor growth. Some ulcerative colitis symptoms in children can mimic other conditions, so it is important to report all symptoms to your pediatrician.
Recommended Reading: Is Ulcerative Colitis Considered An Autoimmune Disease
Whats The Difference Between Ulcerative Colitis And Crohns Disease
UC and Crohns disease are the most common forms of IBD. Both conditions are thought to be the result of an overactive immune system.
They also share many symptoms, including:
- cramps
- diarrhea
- fatigue
However, UC and Crohns disease do have distinct differences. Understanding the key differences between them can help you obtain a proper diagnosis.
Location
These two conditions affect different portions of the GI tract.
Crohns disease may affect any part of the GI tract, from the mouth to the anus. Its most often found in the small intestine. UC only affects the large intestine and rectum.
Response to treatment
Similar medications are prescribed to treat both conditions. Surgery is also a treatment option. Its a last resort for both conditions, but it can be a cure for UC, whereas its only a temporary therapy for Crohns.
Hydrogen Sulphide: Bad Malodorous Gas Responsible For Relapses In Uc
Mercaptides such as sodium hydrogen sulphide are reducing agents that help maintain anaerobic conditions in the colonic lumen. They are produced in the human large intestine by bacterial reduction of dietary inorganic sulphate and sulphite and by fermentation of sulphur amino acids. The acute toxicity of hydrogen sulphide appears to result from inhibition of cytochrome oxidase leading to mucosal damage, loss of barrier function, and histological changes resembling UC. Hence the colonic mucosa has developed a very effective means of detoxifying hydrogen sulphide.
Mainly exogenous sources contribute to the colonic pool of sulphur, such as red meat, cheese, milk, fish, nuts, and eggs, and as preservatives found in commercial breads, beers, many alcoholic drinks, sausages, and dried fruits. Faecal sulphide levels increase after consumption of increasing amounts of meat, providing evidence that meat is an important substrate for sulphide generation by bacteria in the human large intestine.
You May Like: 5 Asa Drugs Ulcerative Colitis
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.
Faecal Butyrate: Key Metabolite In Uc

Short chain fatty acids, including butyrate, proprionate, and lactate, are generated in the colon as result of bacterial fermentation of dietary fibre by luminal bacteria such as Bifidobacterium, Eubacterium, and Lactobacillus species. Roediger et al demonstrated significant inhibition of butyrate but not glucose oxidation by hydrogen sulphide in the ascending colon, splenic flexure, and in the rectosigmoid region. A direct anti-inflammatory effect for butyrate, the most extensively studied of the short chain fatty acids, may be attributable to its inhibition of nuclear factor B, thus preventing the transcription of proinflammatory cytokines. In this study, butyrate also attenuated dextran sulphate sodium induced colitis. Furthermore, butyrate has been demonstrated to reduce colonic permeability by enhancing peroxisome proliferator activated receptor activation. This is of special interest as PPAR- ligands show antineoplastic and anti-inflammatory effects in experimental colitis.
Patients with active extensive UC have decreased colonic butyrate oxidation. As remission of disease is associated with normalisation of butyrate oxidation, UC mucosa is not intrinsically altered in butyrate oxidation. Butyrate enemas have been shown to be of benefit in the management of distal UC.
Also Check: What To Drink For Ulcers