Cooked And Peeled Vegetables
Many vegetables are high in fiber, but as with fruit, peeling them removes a layer of insoluble fiber.
Some vegetables do not need peeling, such as asparagus tips and mushrooms, but it can help to remove the skins of potatoes, carrots, and squash.
Cooking vegetables also makes them easier to digest, and it can reduce the fiber contents.
However, avoid roasting or frying vegetables in oil or butter, because fats can irritate the digestive system and worsen symptoms of Crohns. Try boiling or steaming them instead.
Also Check: Ulcerative Colitis Diet Plan During Flare Up
Avoid Foods That May Exacerbate Uc Symptoms
Because a healthy diet is a cornerstone for overall health, its no surprise that it tops Sniders list of natural remedies for ulcerative colitis. Diet is a foundational treatment for patients with ulcerative colitis, he says, adding that theres often a dietary component to the disease.
According to a review published in October 2014 in Clinical Gastroenterology and Hepatology, people who reported a diet high in fats were more likely to have a relapse of UC. Other studies highlighted in the paper suggested avoiding greasy foods, dairy products, caffeine, and raw fruits and vegetables if you have ulcerative colitis. But the review notes that theres no one-size-fits-all diet for UC, so youll have to figure out what works best for you through trial and error.
It helps to keep a food diary to discover which foods are best for you. Snider says it cant hurt to limit certain foods, and then if your symptoms improve according to your symptom diary, to continue doing so. He also notes that its worthwhile to avoid sugar because its effect on the pancreas hinders the output of anti-inflammatory enzymes.
Avoiding An Ulcerative Colitis Flare
I can still remember many years of living in fear of the next flare-up.
Its a constant worry when you have UC.
Flare-ups become this constant, nagging fear.
Always looking for signs of blood in the toilet.
That sinking feeling when things are looking worse, youre going more and its more urgent.
When you know its not going to slow down and youre in trouble.
Always afraid the next meal will set the UC off again.
Heres the thing we have to think in terms of systems not symptoms.
Flare-ups are actually starting weeks or months before we become aware of them.
Have you ever noticed that your UC or Crohns seems to get worse at the worst possible time?
When stress is at a peak in your life?
I used to always feel like my body was letting me down.
In truth it was the other way around I was letting my body down.
If you oscillate between periods where your UC is calm and periods where it flares-up, that means some things youre doing are helping and some are causing problems.
Almost certainly, the better times involve better eating, better sleep and less stress.
The times when the UC isnt doing so well are usually preceded by a pattern of dietary transgressions, high-stress, lower self-care and no downtime.
When you learn the patterns and learn to control and heal ulcerative colitis flare-ups on your own, you take control of your life back.
You can learn to eat and think and live in ways that move you toward health.
Recommended Reading: What Is The Treatment For Diabetic Foot Ulcers
Unpacking The Link Between The Brain And The Microbiome
byElizabeth Hlavinka, Staff Writer, MedPage Today January 25, 2020
This article is a collaboration between MedPage Today and:
AUSTIN — Patients with higher levels of stress reactivity had more frequent ulcerative colitis flares, according to a small study presented here.
Among 93 patients with ulcerative colitis in symptomatic remission, those with higher levels of stress reactivity — a composite measure of perceived stress and trait anxiety at baseline — were significantly more likely to experience clinical flares across 8 months , reported Jenny Sauk, MD, of the David Geffen School of Medicine at the University of California Los Angeles .
Notably, between patients with high versus lower levels of stress reactivity, there was no difference in baseline fecal calprotectin, a measure of disease activity, Sauk said during a poster presentation at the Crohn’s & Colitis Congress.
“You would think patients who are going to flair more will have higher calprotectin at baseline because calprotectin is a marker of inflammation,” Sauk told MedPage Today. “At baseline, the were not higher, but these patients are still reporting more clinical flairs, so it doesn’t seem to be correlated with our objective measure of inflammation.”
However, stress has been shown to have effects on mucus, permeability, and immune function in murine models, he noted. It may also play a role in noradrenergic signaling and other microbiota processes.
Disclosures
Encountering Emotional Stressors And Facing Them
Possible Emotional Stressors
Other Peoples Perception of UCIts hard if you feel isolated because people around you dont understand how your condition affects you. The symptoms of UC can often be invisible on the outside and you could be worried that others may see you differently because of your condition.
Ways You Can Face Them
Refuse to Suffer in SilenceIf youre concerned that others dont understand what youre going through, try your best to talk about it. Open up and crush the stigma. Educate others that may not understand the facts and let go of the people who refuse to understand. Keep the people who really want to understand and support you close.
Having Symptoms at Work or SchoolWorrying about how to manage your UC symptoms when youre not in the comfort of your own home can be hard. Especially if you arent getting what you need, like a flexible schedule or support from your boss. And while you may know your rights as a patient with a medical condition, sometimes there are negative impacts, like unsupportive people, that are outside your control.
Being in Social SituationsIt can feel easy to stay isolated and keep yourself at home. But every now and then everyone needs to get out and have fun. Thinking of your UC might hinder you from doing things like going to parties, seeing friends, or attending events.
Possible Emotional Stressors
Ways You Can Face Them
You May Like: How Do You Get Rid Of Ulcers
The Relationship Between Stress & Colitis
The systemic effects of psychological stress on the immune and inflammatory systems are complex, and experts believe that both chronic and acute stress is associated with colitis, in terms of encouraging the inflammation that leads to colitis flare-ups. The duration and intensity of the colitis reaction most likely relate directly to the duration and intensity of the stressor. For example, adverse life events or difficult situations, such as being a caregiver or going through a marital separation are more likely to trigger more severe colitis symptoms than a bad day at work or an argument with your best friend.
Stress may not directly cause the condition of ulcerative colitis, but it can aggravate symptoms of the condition and increase the risk, frequency, and severity of flare-ups. And severe, chronic psychological stress may lead to increased bowel inflammation. Also, colitis patients who also live with chronic anxiety are at a higher risk for requiring surgeries, reduced medication adherence, lower quality of life, and higher perceived level of stress. In other words, left unchecked, your stress and anxiety may lead to additional and increased stress and anxiety.
Breaking the GI Stress Cycle can be as simple as focusing on taking deep, diaphragmatic breaths and muscle relaxation can begin to slow the sympathetic arousal mechanisms.
Find Out Whats Happening In Ramseywith Free Real
2: Identify Any Allergens In some cases, ulcerative colitis has been related to allergic reactions to certain foods. Corn, wheat, and milk products seem to be the most common culprits. Elimination of these foods in the beginning of treatment may be required.
3: Fill Up With Fiber Gradually institute a high-complex carbohydrate, high-fiber diet. Include fruits, vegetables and whole grains, excluding wheat and corn initially because they are potential allergens.
Read Also: Nursing Care Plan For Pressure Ulcer Prevention
Dont Skip Your Medication
If you already have prescription medication for colitis, take your medication as prescribed. Dont skip your medicine, even if you feel better.
If you need help remembering to take your medication, use a reminder on your phone and/or set a sticky note on your keys
Sticking with your medication schedule can help you stay in remission and avoid a flare-up.
Stress And Ulcerative Colitis
Experts havenât found an exact link. But they have some theories about the connection between the two.
Inflammation. Your body goes into fight-or-flight mode when stressed. That triggers the release of lots of chemicals, including cytokines. Those are molecules that turn on your immune system and lead to inflammation. People with UC might be more sensitive to this process.
Brain-gut axis. Stress changes the signals that travel between your brain and gut. This can cause all kinds of digestion problems, even in people who donât have UC. These changes are also linked to irritable bowel syndrome , food allergies, and heartburn.
Other reasons. Research shows stress might:
- Damage the lining of your gut
- Disturb gut bacteria
- Tai chi
- Guided imagery
You can also just take a little time each day to do something you find relaxing. That could be gardening, reading, or listening to music. Whatever you enjoy.
Drug therapy is another option. Studies show antidepressants might ease pain in people with IBD. Common choices include selective serotonin reuptake inhibitors and tricyclic antidepressants . Ask your doctor if theyâre right for you.
Recommended Reading: Patient Education On Pressure Ulcer Prevention
Failure To Have A Gastroenterology Specialist On Your Side
Your primary care physician can only do so much for you. In order to adequately manage and treat your Crohns or ulcerative colitis, you will need to see a specialist for regularevaluation. In fact, you should have a whole team of doctors working for you, from surgeons to radiologists to nutritionists however, your gastroenterologist should be your main point of contact when it comes to your condition.
We treat patients with Crohns and ulcerative colitis as well as a variety of other gastrointestinal diseases, including colon cancer, hepatitis, biliary diseases, esophageal disorders, and peptic ulcer disease. Our specialists can offer you more tips on how to best manage your condition, and work with you one-on- one to develop a workable treatment plan.
Please note, the information provided throughout this site is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. All content, including text, graphics, images, and video, on or available through this website is for general information purposes only. If you are experiencing related symptoms, please visit your doctor or call 9-1-1 in an emergency.
GET OUR FREE NEWSLETTER
You May Like: What Should You Not Eat With An Ulcer
Study Design And Inclusion Criteria
This is a cross-sectional study and includes all patients18years old with a primary diagnosis of acute diverticulitis in 2014. The ICD-9 CM codes used were 56211, 56201, 56213, and 56203. The database was then queried to include all patients with prior diagnosis of CD or UC . Patients included in the study were required to have a primary diagnosis of acute diverticulitis with a prior diagnosis of either UC or CD. Primary study outcomes included mortality, cost of hospitalization, and length of stay for diverticulitis with either UC or CD. A second comparison was made between those with CD and those without IBD. Various patient demographics , comorbidities, and hospital characteristics were obtained. The severity of the co-morbidities was analyzed via the Deyo modification of the Charlson comorbidity index . This index measures 17 common medical conditions and assigns different weights to compile a score from 0 to 33, which correlates with overall severity of illness.
You May Like: Can Stress Give You An Ulcer
You May Like: What Is Good For Ulcers In Your Mouth
Talk With Others Who Understand
Another great tool for managing stress is connecting with others, and especially those who understand what youre going through. Joining an ulcerative colitis support group, whether in-person or virtual, can help address your stress levels and improve your quality of life.
MyCrohnsAndColitisTeam is the social network for people with Crohns disease or ulcerative colitis and their loved ones. On MyCrohnsAndColitisTeam, more than 139,000 members come together to ask questions, give advice, and share their stories with others who understand life with inflammatory bowel disease.
Are you living with stress and ulcerative colitis? Share your experience in the comments below, or start a conversation by posting on your Activities page.
Are Nutritional Needs Different For People With Ibd What Are The Specific Nutritional Needs For People With Crohns Disease And Ulcerative Colitis
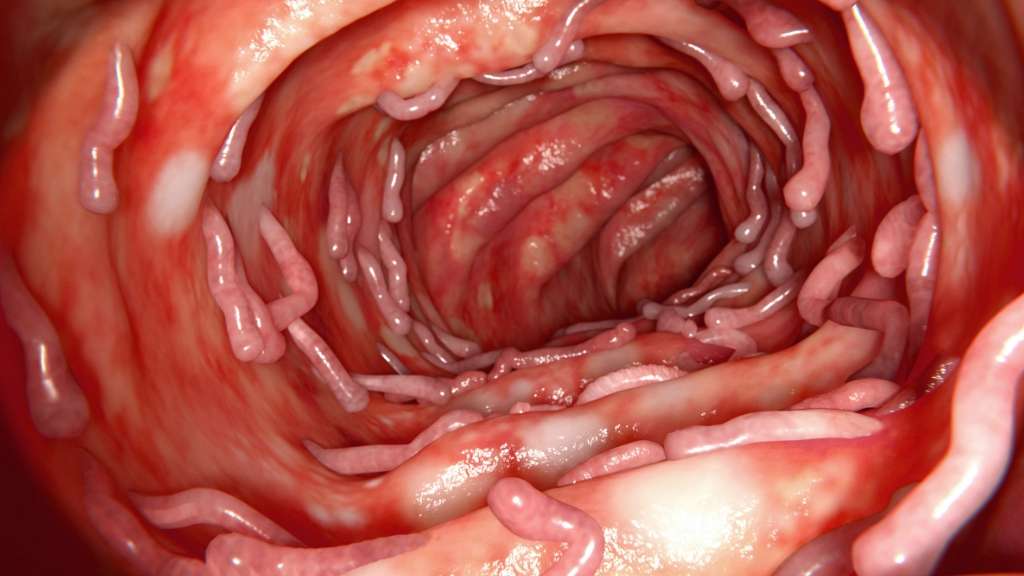
Nutritional needs are specific to the individual and differ with disease state, body size and age. A nutritionist can help you estimate your individual needs. Calorie and protein needs are similar for Crohns disease and ulcerative colitis. In both diseases, needs increase during inflammation and immediately after to restore losses. The following are general statements about nutritional needs that may apply to you.
Don’t Miss: Alternative To Sulfasalazine For Ulcerative Colitis
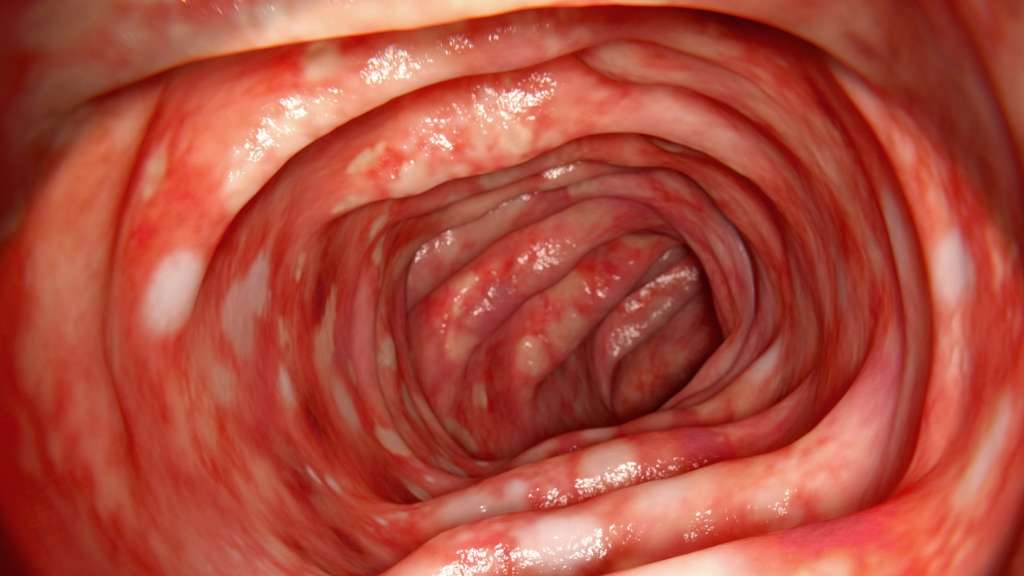
Colon Cancer And Ulcerative Colitis
When you have ulcerative colitis, you may be more likely to get colon cancer. Your chances go up if you dont get treatment for UC. Thats because unchecked inflammation can cause changes in the cells in your colon. These cells may turn into cancer down the road.
Your chances of getting colon cancer go up if youve had ulcerative colitis for 8 years or longer. The odds are also higher if:
- Your inflammation doesnt go away.
- Youre a man.
- You have a liver condition called primary sclerosing cholangitis.
- You have a family member whos had colon cancer.
Some research shows that people with UC may be less likely to get colon cancer now than in the past. Experts think its because doctors now have better ways to screen for colon cancer and they do it more often. It also helps that new medicines, like biologics, do a good job of curbing inflammation.
The Autonomic Nervous System
The sympathetic and parasympathetic autonomic nervous systems serve the entire gastrointestinal tract and are closely connected with the enteric nervous system . Together, these systems govern secretion, motility, sphincter control, and microcirculation in the gut . Under stress conditions, the ENS produces large neuropeptides, which in turn affect intestinal immunity and inflammation. Geboes et al. found that there are mixed abnormalities in all CD and UC patients for different cell types of the ENS . Another study showed that patients with UC have markedly lower autonomic functions in comparison to those with CD and healthy controls .
Stress can activate the sympathetic autonomic system, leading to increased production of major adrenal medulla hormones, mainly catecholamines, such as epinephrine and norepinephrine. Catecholamines mediate increases of central and peripheral inflammatory cytokines and activation of the inflammatory nuclear factor B signaling pathway in response to stress . In addition, the vagus nerve, which has anti-inflammatory effects, is inhibited by stress, leading to an increased systemic inflammatory response to endotoxin and intestinal inflammation .
Recommended Reading: Diet To Control Ulcerative Colitis
Stress: Pathways And Pathophysiology
More than 80 years ago, Hungarian endocrinologist Hans Hugo Bruno Selye first defined the medical term stress as the physiological adaptive responses of organisms to adverse threats , which are endogenous or exogenous, psychological or physical, real or perceived . To maintain homeostasis under threat, organisms have evolved an extremely complex system, called the stress system, which involves physiological and behavioral adaptations via appropriate central and peripheral neuroendocrine responses. When exposed to long-term or severe stress, the organisms may reach a state called cacostasis, in which many vital physiological functions are impaired, and may develop many acute and chronic diseases . Stress-induced disorders occur in multiple systems throughout the body, among which the gastrointestinal tract is a sensitive system.
When the brain receives stress input, multiple pathways containing the autonomic nervous system and hypothalamic-pituitary-adrenal axis are activated . Stress from different sources results in modifications of the brain-gut axis, which eventually leads to the progression of a wide range of gastrointestinal disorders. The frequently involved diseases include IBD, irritable bowel syndrome , peptic ulcers, food antigen allergic reactions, and gastroesophageal reflux disease. The potential mechanisms are summarized in the following sections .
How Is Ulcerative Colitis Treated
Treatment for UC depends on the severity of the disease and often involves both medications and lifestyle modifications.
Medications
Most people require a combination of medications to suppress and/or modulate the immune system:
- Anti-inflammatory drugs: Anti-inflammatory drugs such as 5-aminosalicylates and corticosteroids suppress the cells that cause inflammation. These drugs are usually the first step in the treatment of UC and are well tolerated by most people.
- Immune system suppressors: Immunosuppressant drugs work by suppressing the immune system response that stimulates the inflammation process. Examples include Azasan and Imuran Purinethol and Purixan Gengraf, Neoral and Sandimmune and Xeljanz .
- Biologics : Biologics target and neutralize proteins produced by the immune system. Examples include Remicade , Humira and Simponi . Entyvio is a type of biologic that works by blocking the inflammatory cells from reaching certain parts of the body, and can be used for people who cant tolerate other biologics.
- Anti-diarrheal medications: Your doctor may recommend anti-diarrheal medications such as Imodium for severe diarrhea. You should avoid taking over-the-counter anti-diarrheal medications without consulting your doctor, because they can increase the risk of toxic megacolon .
- Painkillers: Tylenol is safe to use for pain relief. Talk to your doctor before taking other OTC pain medications.
- Antispasmodic medications: Antispasmodic medications can help reduce cramps.
You May Like: Can Stress Cause Ulcerative Colitis Flare Up