Treating Ulcerative Colitis Is Important To Prevent Complications
Robert Burakoff, MD, MPH, is board-certified in gastroentrology. He is the vice chair for ambulatory services for the department of medicine at Weill Cornell Medical College in New York, where he is also a professor. He was the founding editor and co-editor in chief of Inflammatory Bowel Diseases.
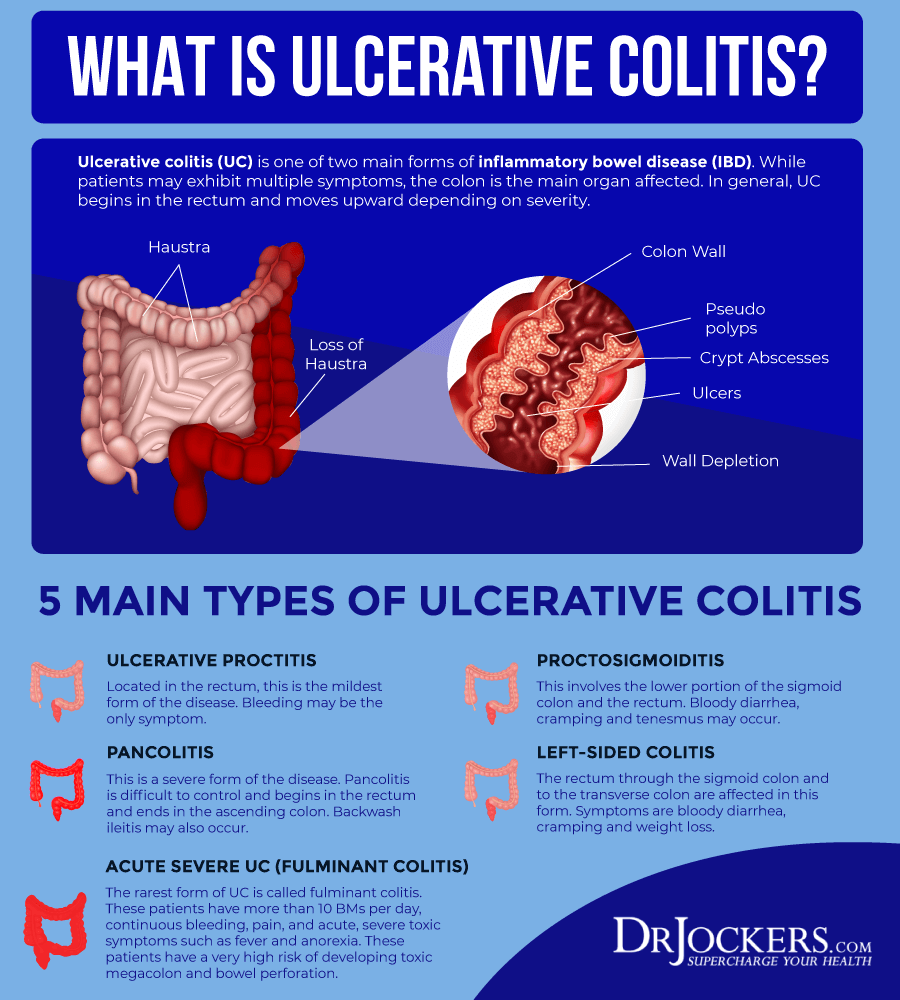
Ulcerative colitis is a chronic illness that is a type of inflammatory bowel disease . Ulcerative colitis is usually characterized as causing inflammation in the lining of the colon, but it is an immune-mediated condition. This means that it involves the bodys immune system, which can lead to effects in organs and body systems other than the digestive tract.
A diagnosis of ulcerative colitis is difficult to receive for many reasons. Often people have not even heard of the disease before their diagnosis. Learning that it will probably mean taking medication for the rest of their lives can be upsetting and daunting.
In addition, ulcerative colitis goes through periods of active disease and less active or no activity . Little is currently known about why ulcerative colitis might flare-up, though some people living with the disease are able to identify their personal triggers.
Also Check: Symptoms Of A Bleeding Ulcer In Your Stomach
How Are Ulcerative Colitis And Mental Health Connected
UC is an unpredictable disease. You might feel energetic and well one day, but experience debilitating pain and diarrhea a few days later.
The constant ups and downs of this condition can make it difficult to plan ahead or complete everyday activities. You might have trouble keeping up with work or school, or it might be a challenge to maintain an active social life.
UC is a chronic, long-term condition that doesnt have a cure yet. Most people living with UC experience symptoms on and off for their whole life. The unpredictable nature of this disease can significantly affect quality of life.
Depending on the severity of your symptoms, it can feel as if youre being held hostage by your own body. For these reasons, some people living with UC may develop anxiety and depression.
Some researchers also believe that the connection between UC and mental health extends beyond the unpredictable and chronic nature of this condition.
UC is an inflammatory bowel disease, and theres evidence suggesting a link between inflammation and depression.
Inflammation is your bodys natural response to foreign substances and infections. When your body is under attack, your immune system stimulates an inflammatory response. This prompts the healing process.
Depression isnt an inflammatory disorder. But inflammatory pathways in the brain can interfere with neurotransmitters. This reduces your level of serotonin, a chemical that plays a role in happiness and well-being.
Ethics Approval And Consent To Participate
The nature of the study was discussed with each patient, and written informed consent was obtained from all parents before participating in the study. This study was approved by Ain Shams University Hospital Ethics Committee after a very clear statement that provided information on the following points: study rationale participation in this study was completely free and voluntary participation in the study had no direct benefit to him, although the data obtained could be used for the benefit of other patients they may be withdrawn at any time without giving any justification and without affecting their care service and the results of the study may be used for scientific publication but the identities of the patients would be completely secret.
The committees reference number is R 107/ 2021.
Recommended Reading: What Is The Medication For Ulcerative Colitis
Ulcerative Colitis And Colorectal Cancer
Ulcerative colitis increases the risk of colorectal cancer. Colorectal cancer often begins as small growths on the inside of the large intestine. The risk of colorectal cancer increases based on:
- the length of time a person has had ulcerative colitis
- how much of the colon is affected by ulcerative colitis
People with ulcerative colitis should have more frequent tests for polyps and colorectal cancer than people at average risk. The gold standard screening test is a colonoscopy. Polyps can be removed during a colonoscopy. This reduces the risk of colorectal cancer. Ask your doctor how often you should be checked for colorectal cancer.
Surgery to remove the entire colon eliminates the risk of colon cancer.
What Are The Symptoms Of Irritable Bowel Syndrome
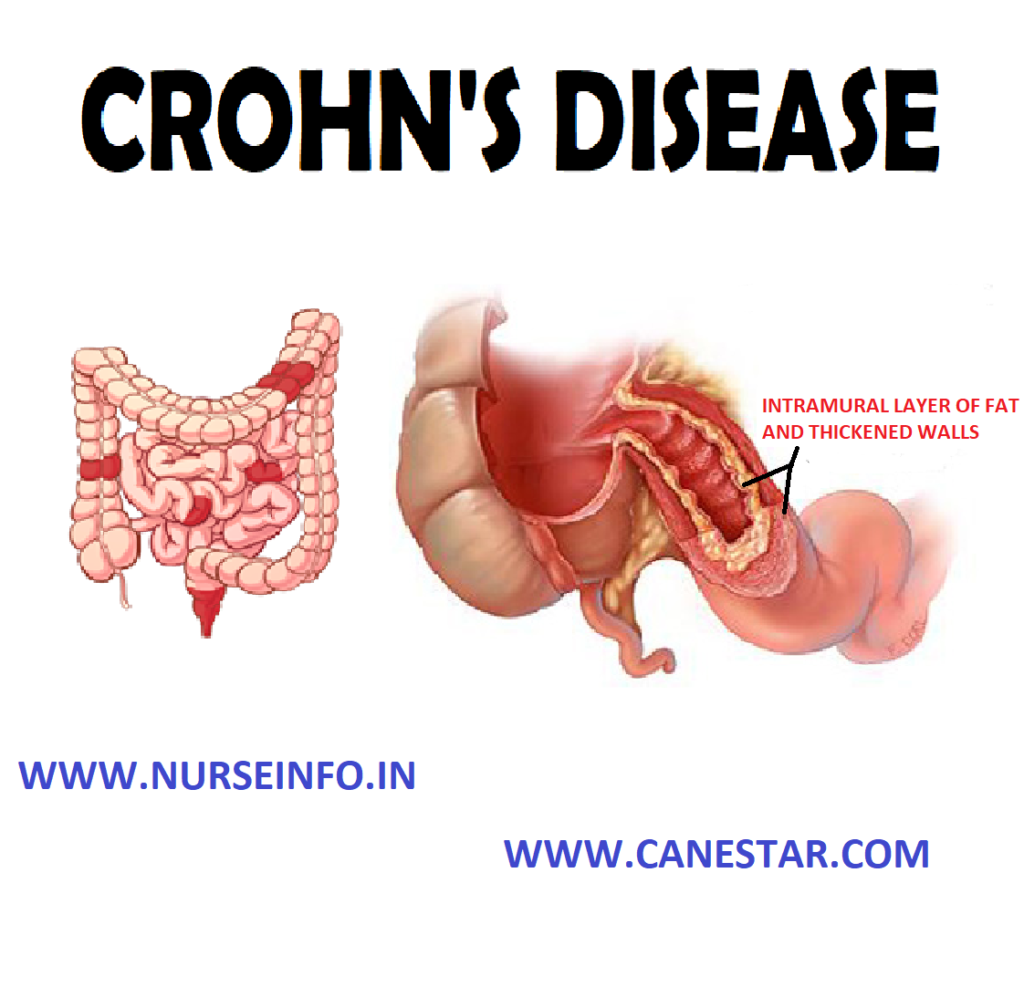
Even though UC and Crohns disease affect different areas of the body, they often produce some of the same symptoms, such as:
- Abdominal pain
- Blood in the stool
- Loss of appetite
If you experience several of these symptoms for more than several days, particularly rectal bleeding or blood in the stool, it would be wise to make an appointment with your healthcare provider. While rectal bleeding could be something as simple as a hemorrhoid, it could indicate something more serious. IBD usually isnt a fatal disease, but it can lead to lifelong medical complications that can seriously decrease ones quality of life if left untreated and ignored.
Also Check: Do Ulcers Cause Weight Loss
What Do Anxiety And Depression Look Like
Whether youve just been diagnosed, or this is your 200th Crohns flare-up, and its simply the last straw, youre not the only one who may be feeling stressed, anxious, or down about an IBD diagnosis. Everyone gets sad and feels down at times, but one thing to realize about depression is that symptoms stick around for two weeks or longer. If youve been experiencing:
- Loss of interest in things and activities you once enjoyed
- Insomnia
- Feelings of guilt or worthlessness
- Difficulty concentrating
For two weeks or more, and youre wondering, what do I do about anxiety or depression? The best thing to do is to contact your healthcare provider. There are various treatments for depression, and its important to know that a depressive episode is not likely permanent. Cognitive-behavioral therapy and medication-assisted treatment both have efficacy when it comes to depression treatment.
Anxiety and depression often appear together, although its possible to have just one without the other. Anxiety presents with different symptoms, some of which include:
- Feeling nervous or edgy
- Feeling doom, as if something bad is about to happen
- Not being able to stop worrying
- Ruminating on problems
- Feeling annoyed or easily irritated
Southern Cross Medical Library
The purpose of the Southern Cross Medical Library is to provide information of a general nature to help you better understand certain medical conditions. Always seek specific medical advice for treatment appropriate to you. This information is not intended to relate specifically to insurance or healthcare services provided by Southern Cross. For more articles go to the Medical Library index page.
Also Check: How To Heal Venous Stasis Ulcers
Articles On Managing Ulcerative Colitis
Ulcerative colitis can make life hard to predict. A flare-up of symptoms is stressful and can leave you worn out for days, weeks, or even months. Even in remission, you might get tired a lot or have a hard time meeting friends or going to work. Itâs easy to see why living with this long-term inflammatory disease can affect your mental health.
There’s no evidence that stress actually causes inflammatory bowel disease , which includes UC and Crohnâs disease. But stress can definitely bring on a flare-up. And you’re more likely to feel anxious and depressed than your friends without UC. Your chances are even higher if you are a woman. Even rats with IBD in lab studies show signs of mood problems.
But there are steps you can take to lift your mood, even when your symptoms get you down.
Ways To Keep Your Heart Healthy If You Have Uc
Follow these steps to lower your risk of heart disease and ease your UC flares.
You May Like: Best Cure For Mouth Ulcers
Don’t Miss: What Foods Irritate An Ulcer
Coping With Stress And Ulcerative Colitis
To reduce ulcerative colitis flare-ups, it isnt always enough to take your medication and stick with your doctors treatment plan. Its can also be helpful to find ways to lower your stress level. Here are some strategies to help you manage stress:
Prevalence And Risk Factors Associated With Anxiety And Depression Disorders
Furthermore, large longitudinal studies had consistently shown more frequent IBD flares and worse disease activity in those with symptoms of anxiety and depression disorders . In a cohort of 2,007 patients followed over 9 years from the Swiss, the results showed an association between depressive symptoms and clinical recurrence of IBD . In a large longitudinal study of patients with IBD from USA with almost 2 years follow-up, Bharati Kochar et al. found that baseline depression patients with CD have an increased risk of recurrence , hospitalization or IBD-related surgery . UC patients with baseline depression also have an increased risk of relapse , hospitalization , or surgery at follow-up .
In conclusion, new onset of disease, disease activity, side effects of medications, stressful life events, inpatient status and lower socioeconomic status can easily affect the mood of one or two types of IBD . The increased prevalence of anxiety and depression disorders required a mental screening of each patient with IBD at initial consultation.
Recommended Reading: What Is The Recommended Diet For Horses With Ulcers
The Role Of Peripheral Substance P
In addition to its central effects, peripheral release of SP from the ENS may have a role in stress induced increases in mucosal inflammation. Although there are no published data to show an increase in mucosal SP in response to stress, SP containing neurones are found in close association with mast cells, a cell type implicated as central in mediating stress induced permeability changes . SP has been shown to increase histamine release from mucosal mast cells in patients with IBD. Lastly, SP can act not only as a neurotransmitter but also an inflammatory cytokine in its own right, enhancing cytokine production and stimulating chemotaxis of inflammatory cells. It also increases expression of leucocyte adhesion molecules on microvascular endothelium, and of CD11b on neutrophils, facilitating leucocyte adhesion at sites of inflammation.
Alternative Treatments For Managing Ulcerative Colitis Flare
Some people with ulcerative colitis feel better when they are on fish oil, probiotics, and herbal supplements. Alternative treatments such as acupuncture also work for some.
Some studies have investigated the impact of various formulations of cannabis on inflammation in IBD. Formulations of cannabis products can include CBD only, CBD with THC at various percentages, and THC alone. Cannabis was found to be effective in reducing symptoms of IBD, such as diarrhea and abdominal pain, but not in controlling inflammation associated with IBD.
Read MyCrohnsAndColitisTeams interview with Dr. Kinnucan to find out more about CBD oil and cannabis for IBD here.
Don’t Miss: Pediatric Ulcerative Colitis Treatment Guidelines
Growth And Development Problems For Children
You can get ulcerative colitis at any age, but its more common among 15- to 30-year-olds. A child with UC may:
- Be underweight
- Red or discolored
Continued
Talk to your doctor right away if youre worried that you might have DVT. Its possible for a deep-vein blood clot to break loose and get stuck in a lung artery. If that happens, its an emergency called a pulmonary embolism . You could have symptoms like shortness of breath, sharp chest pain, and a cough with or without blood. Call 911 if you have these signs.
Doctors can treat DVT and pulmonary embolisms with medications, a filter through a vein that removes the clot, or surgery.
You could be more likely to get DVT or PE if you:
- Have ulcerative colitis that flares often or affects a large amount of your colon.
- Get surgery for severe ulcerative colitis.
Some studies also link certain ulcerative colitis meds, like steroids or tofacitinib, to DVT and PE.
Cut Out Raw Veggies And Other Gut Irritants
In the midst of a ulcerative colitis flare, you want to be as gentle on your digestive system and colon as possible. Give your gut a little vacation, says Cohen. This ideally means eliminating or scaling back on: raw vegetables, raw and cooked fruits, high-fat foods , high fiber foods , spicy foods, alcohol, and caffeinated beverages. Basically, any food that takes significant digestive effort or stimulates the bowels.
Also Check: How To Treat A Diabetic Ulcer
Manage Your Anxiety Manage Your Colitis
Managing symptoms of psychological stress and anxiety, unfortunately, won’t cure your ulcerative colitis, but it may help alleviate some of its symptoms and reduce the frequency of ulcerative colitis incidents. Put simply, reduce your stress levels, reduce your discomfort caused by colitis.
It’s virtually impossible to avoid psychological stress and stressful situations at all times completely, so it’s unreasonable and unrealistic to think that you can manage your ulcerative colitis by keeping stress and anxiety out of your life. You can, however, realistically keep stress levels down by eating well and avoiding foods that trigger your ulcerative colitis, like whole grains, nuts, seeds, and fibrous fruits. It is also helpful to take any prescribed medications as directed, sleep well, exercise, have a strong support system, and commit to taking time to relax, through meditation, or just a few dedicated minutes each day for self-care. Yoga can be especially effective because, in addition to relieving symptoms of stress and anxiety, yoga has also been shown to relieve symptoms of ulcerative colitis.
Cognitive behavioral therapy can also be extremely helpful. Using CBT techniques, a psychologist or therapist can help you learn to observe your negative thoughts and then change or reframe them. Instead of “Oh no, here we go againâ¦,” you might think, “I’m going to face this flare-up more calmly, so it will be less severe than last time.”
What Every Physician Needs To Know:
The inflammatory bowel diseases , ulcerative colitis and Crohns disease, are immune-modulated disorders of the gastrointestinal tract that also have a number of manifestations outside the gut. Extraintestinal manifestations of IBD include pyoderma gangrenosum, erythema nodosum, uveitis, hemolysis, arthritis, and a broad variety of respiratory disorders. Respiratory disease in IBD patients can manifest anywhere from the larynx to the pleura. Bronchiectasis is the most common pulmonary manifestation of IBD.
Evidence of respiratory abnormalities in patients with IBD include more frequent symptoms of wheeze, cough, sputum production, and/or breathlessness than those in the general population abnormalities of pulmonary function testing, including decreased DLCO and bronchial hyperreactivity decrements in pulmonary function during IBD flares more radiographic abnormalities, such as air trapping, peripheral reticular opacities, cysts, and ground glass opacification on high-resolution scans compared to non-IBD controls increased frequency of asthma increased incidence of venous thromboembolic disease with even higher risk during IBD exacerbations bronchoalveolar lavage fluid lymphocytosis and inflammatory changes in the submucosa of airways as occurs in regions of the GI tract affected by IBD.
You May Like: How Do You Heal An Ulcer
You May Like: How To Get Remission In Ulcerative Colitis
Metabolomic Signatures Of Patients With Active Uc And Depression/anxiety
Compared with UCNA/UCND, UCA/UCD harbored more glycocholic acid and glycochenodeoxycholate ). The ROC analysis showed that glycochenodeoxycholate alone had a fair prediction performance on UC-related depression and anxiety ), while 1-stearoyl-2-hydroxy-sn-glycero-3-phosphocholine was positively associated with anxiety based on both analyses and had a potential to be a predictor of anxiety levels Supplementary Figure S5). Besides, 2-deoxy-D-ribose, 1-stearoyl-sn-glycerol,1-stearoyl-rac-glycerol, and thioetheramide-PC were all revealed by both analyses to be related with depression and anxiety in patients with UC ). It should be noted that dopamine, a well-known neurotransmitter related to the reward system in the brain, was positively associated with both anxiety and depression levels in patients with UC , Supplementary Figure S5).