Feeling Comfortable With Your Doctor
Its not always easy to talk about your bowel habits. Talking about poop can be embarrassing, and many people may not be ready to open up to their doctor about it.
Others may ignore the changes to their stool or think that nothing is wrong. However, ignoring symptoms will only make things worse.
Your doctor has studied the gastrointestinal tract along with all that it does and produces. They have seen and heard it all. Nothing you say about your bowel symptoms is going to offend or shock them.
Its part of their job to know about any changes in your symptoms. Your doctor is there to help you, not to judge you.
You dont have to know any fancy medical terms when talking with your doctor about your symptoms. Share your concerns and any changes in your bowel habits you have noticed. Talking with them about changes in your stool can only help get you closer to resolving the problem.
Surgical Therapy For Manifest Colorectal Cancer In Ulcerative Colitis
In all decisions, the nutritional state of the patient as well as the current medications have to be considered as this may significantly influence morbidity and mortality in these patients. If the patient is in a reduced state and/or under immunosuppressive therapy, primary restorative proctocolectomy should be generally avoided.
Biomarkers From Colorectal Biopsies
Aneuploidy
Aneuploidy is the presence of an abnormal number of chromosomes in a cell. It generally develops during cell division when chromosomes are not properly divided into two cells and a missing or extra chromosome in a fetus is a common cause of genetic disorders. An increased incidence of aneuploidy has been observed in correlation with dysplastic mucosal changes and Rubin et al. have reported that DNA aneuploidy precedes dysplasia by 12.5years in colonic biopsies, which makes it act as a possible predictive factor for the development of dysplasia in UC. Moreover, Meyer et al. have reported aneuploidy in non-malignant mucosa adjacent to CACC, which appears to be irrespective of dysplasia. A recent meta-analysis has indicated that aneuploidy is as competent as dysplasia in assessing CACC risk and a combinational analysis of the two parameters is superior to that of a single parameter .
Genetic susceptibility
P53 mutation
DNA methylation
Protein molecule
MicroRNAs
Signaling pathways
Read Also: How Is Ulcerative Colitis Caused
Prognosis Of Ulcerative Colitis
Ulcerative colitis is usually chronic, with repeated flare-ups and remissions . In about 10% of people, an initial attack progresses rapidly and results in serious complications. Another 10% of people recover completely after a single attack. The remaining people have some degree of recurring disease.
People who have ulcerative proctitis have the best prognosis. Severe complications are unlikely. However, in about 20 to 30% of people, the disease eventually spreads to the large intestine . In people who have proctitis that has not spread, surgery is rarely required, cancer rates are not increased, and life expectancy is normal.
Diagnosis And Surveillance Strategies
Surveillance colonoscopy should be performed for the early detection of dysplasia and CRC in IBD with colonic involvement. There is a proven benefit of endoscopic surveillance estimated up to 5 years in IBD patients, which is up to ten times greater than in the rest of the population. Diagnosis of dysplasia is a challenge because is asymptomatic in most cases and its detection can be operator dependent, as well as the ability and expertise of the endoscopist. In most cases, regardless of the operator’s ability, if the patient has activity at the time of the study, it may make difficult to detect dysplasia so thats why a screening colonoscopy is recommended in clinical remission to detect dysplasia and not only see inflammatory changes in the mucosa. Intervals between surveillance colonoscopy should be according to CRC risk factors and the previous results of colonoscopy studies . A high detection rate of dysplasia or CRC lesions is due to a trained endoscopist, complete bowel preparation, high definition equipment and the use of techniques that improve the detection of lesions such as chromoendoscopy Compared to standard evaluation with a big number of colonic biopsies and finally a procedure with longer duration to increase dysplasia detection .
Don’t Miss: What Foods Can I Eat If I Have An Ulcer
Never Skip A Regular Screening
People who have ulcerative colitis that extends past the sigmoid colon should start annual colonoscopiesa test where doctors use a long, flexible tube with a camera attached to inspect the inside of the colonno later than eight years after symptoms appear, says Dr. Ehrlich.
Your doctor may also take a biopsy during your screening, especially if he or she notices dysplasia or cells that look cancerous.
If youve previously had dysplasia or a bile duct inflammation called primary sclerosing cholangitis, your physician may spray a blue dye onto the colon walls to spot cancerous areas more easily.
If You Have Dysplasia Consider Having Your Colon Removed
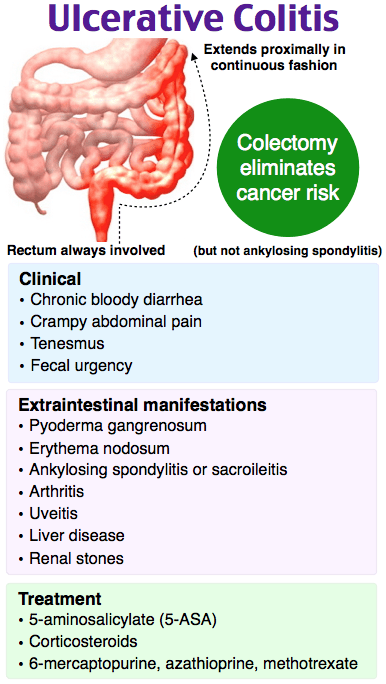
Patients with high-grade dysplasia may need to have a colectomy, a surgical procedure to remove some or all of the colon.
However, if the dysplasia is low-grade, the bumps and nodules can often be completely taken out during a colonoscopy.
Doctors may also choose to monitor low-grade dysplasia with more frequent colonoscopies to see if the inflammation regresses with treatment, says Dr. Ehrlich.
Also Check: How Does One Get Ulcerative Colitis
Molecular Biomarkers For Surveillance
Although conventional surveillance colonoscopy may contribute to a decline in CACC incidence, given that it can detect and remove some dysplasia lesions, it still has certain disadvantages that may impair an accurate evaluation. For example, both endoscopic and histopathological examinations are dependent on expert knowledge and experience thus, these examinations are slightly subjective, and an inexperienced or a careless expert may overlook the presence of dysplasia, making endoscopy incompetent for such surveillance. In addition, some studies have highlighted endoscopy surveillance failures in 5080% of cases with colitis-associated neoplasms, lesions remain undetected on endoscopy . In contrast, molecular monitoring has the advantage of high compliance and objectivity and may have a potential clinical value as a complement tool for screening dysplasia/cancer among UC patients.
Alarm Symptoms Of Ulcerative Colitis:
If you are already diagnosed with ulcerative colitis, there are several alarm symptoms to look out for. A change in your ulcerative colitis symptoms may mean that additional treatment is needed. Talk to your doctor immediately if you experience a new symptom, a change in your current symptoms or any of the following:
- An unusual amount of cankers or sores in your mouth
- Unexplained or unintentional weight loss
- Failure to gain weight
- Delayed puberty in teens
- Drainage of pus from, or severe pain near, the anus which is usually caused by an abscess.
- Anemia this blood condition results in fatigue and weakness. It is usually caused by heavy blood loss or a lack of dietary iron
- Rectal bleeding
- Nausea / vomiting – inability to keep food / drink down
Recommended Reading: Best Protein For Ulcerative Colitis
You Need To Know Your Family History
Among those with ulcerative colitis, not all cancer risk is the same.
A family history of colorectal cancer doubles your odds of getting the disease, according to a study in the World Journal of Gastroenterology, as compared to patients without a family history.
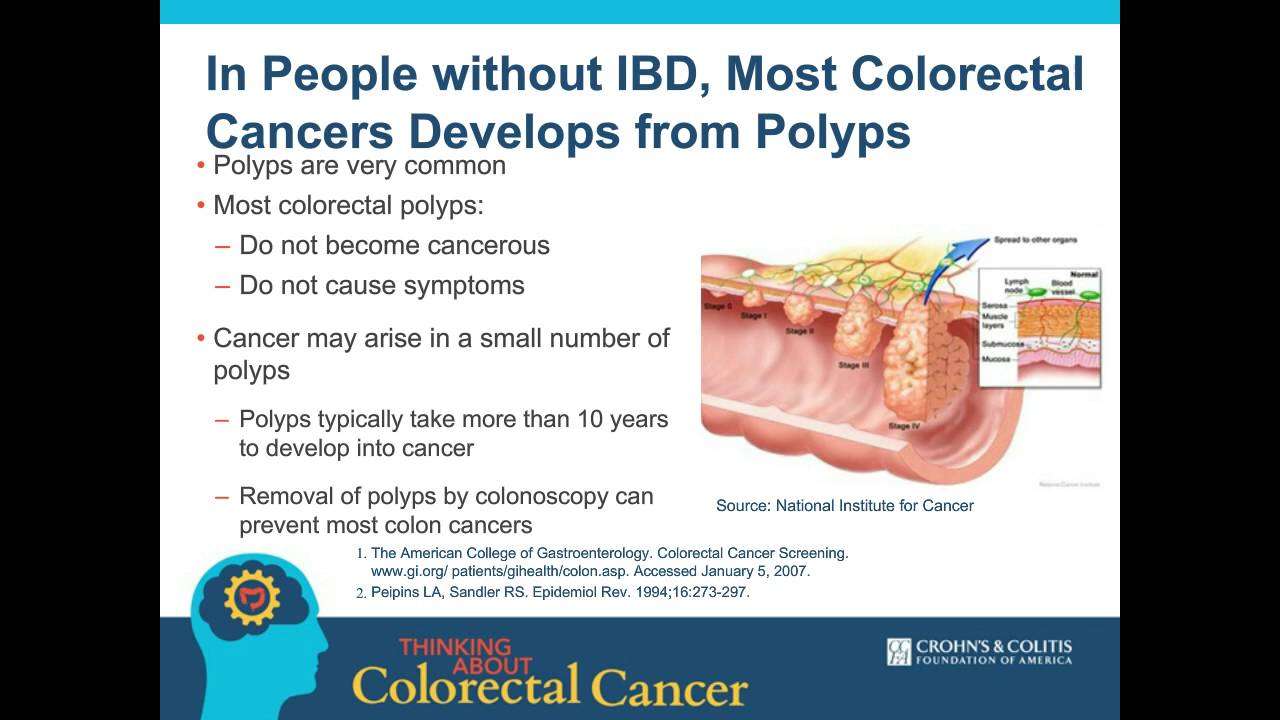
Tell your doctor if you have a family history of colorectal cancer familial adenomatous polyposis, a condition in which the intestine is lined with benign polyps or Lynch syndrome, a genetic disorder characterized by polyps in the colon.
All raise your cancer risk.
Treatment Based On Severity And Alternative Treatment
For mild symptoms of UC, steroid medicine, aminosalicylates, enemas or suppositories, antidiarrheal medication, and diet changes may be suggested. For moderate to severe symptoms of UC, higher doses of the previously mentioned medications may be prescribed, immunomodulator medicines or cyclosporine, biologics, surgery and the removal of the colon. In the hospital, to treat anemia, severe diarrhea, and nutrition deficiencies due to malabsorption of nutrients from foods, treatment may include blood transfusions, replacing electrolytes and fluids lost. There are also natural or alternative medicine treatments and therapies available in place of prescribed medications. These therapies may include nutritional supplements, herbal remedies, acupuncture, and diet changes. It is recommended that anyone considering alternative treatments have a discussion with their doctor.
Also Check: Ulcerative Colitis And Renal Failure
Genetics Of Ulcerative Colitis Associated Colorectal Cancers
Both genetic and environmental factors contribute to the pathogenesis of CRC in IBD. Most sporadic CRC cases arise from a preceding adenoma associated with unique genetic mutations. IBD-related cancers, however, are associated with a partially different genetic background. The increased risk is thought to be an acquired event in IBD, although common inherited factors have been proposed as a link between both forms of IBD and CRC.
Complete elucidation of the mechanism of UC-CRC carcinogenesis will require further investigations however, chronic inflammation is thought to be the most important driving mechanism. Although the same three molecular pathways that have been described for sporadic colon carcinogenesis are also found in colitis-associated neoplasms, yet the timing and frequency of some of the key genetic changes are different ,1), possibly due to the different main driving mechanisms.
Summary of geneticalte-rations in sporadic colorectal cancer and colitis-associated colorectal cancer . The timing of p53 and APC mutations is different unlike in sporadic neoplasia, mutations and LOH in p53 are early events in UC-associated CRCs. The opposite was reported for APC mutations.
Recently, an association was reported by the Mayo Clinic between the G308A TNF polymorphism and the risk of UC-associated CRC in 114 UC-CRC cases and matched controls, further corroborating the importance of chronic inflammation in CRC pathogenesis.
Myth : Having Ulcerative Colitis Means You Need To Have Part Of Your Colon Removed
Most people with ulcerative colitis do not need surgery to remove their colon or rectum. Taking medications and making lifestyle changes are often enough to keep inflammation and other symptoms under control in people with ulcerative colitis.
However, surgery provides a treatment option when medications and lifestyle changes are not enough to control the symptoms.
According to the authors of a 2019 review, up to with ulcerative colitis will eventually need surgery to remove part or all of the colon.
There are several types of surgery for ulcerative colitis:
- partial colectomy, wherein a surgeon will remove part of the colon
- total colectomy, wherein a surgeon will remove the entire colon
- proctocolectomy, wherein a surgeon will remove the colon and the rectum
Getting treatment for ulcerative colitis can help:
- reduce inflammation
- ease pain and other symptoms
- prevent complications such as malnutrition
A doctor may prescribe a combination of treatments for ulcerative colitis, such as:
- biologic therapy or other medications to reduce inflammation
- pain relievers or other medications to relieve symptoms
- changes to diet or other lifestyle habits
If medications and lifestyle changes are not enough to relieve the symptoms, a doctor may recommend surgery.
You May Like: Is Soy Milk Good For Ulcerative Colitis
All Information You Need About Ulcerative Colitis Colon Cancer Screening
Useful and related information about Ulcerative Colitis Colon Cancer Screening are listed by MedicineContact on this page and you can take a look.
coloncancerscreeningulcerativecolitiscolitis
Colorectal Cancer Surveillance In Inflammatory Bowel …
Copy the link and share
hotgut.bmj.com
coloncolitiscancerscreeningcolon
Guidelines For Screening And Surveillance Of Asymptomatic …
Copy the link and share
News Result For Ulcerative Colitis Colon Cancer Screening
Colon CancerYour browser indicates if you’ve visited this link
CBS Philly
coloncancerScreeningCancercancerscreening
Healthbeat: A Holiday Discussion: Health Screening StatusYour browser indicates if you’ve visited this link
WYOU
screeningsscreeningsscreenings
The Role of Endoscopy in Inflammatory Bowel DiseaseYour browser indicates if you’ve visited this link
Medscape
Screeningcancerulcerativecolitis
Gastro Societies Recommend CRC Screening Begin at Age 45Your browser indicates if you’ve visited this link
Gastro & Endo News
Cancercancerscreening
Colon cancer: the chronic condition that puts you at a higher riskYour browser indicates if you’ve visited this link
Leicester Mercury
Ulcerativecolitiscoloncancercancerscreeningscreening
Cancer: Condition putting you at a higher risk – toilet signsYour browser indicates if you’ve visited this link
Daily Express
Ulcerativecolitiscoloncancercancerscreeningscreening
FDA Approves DNA-Based Colorectal Cancer TestYour browser indicates if you’ve visited this link
MD& M East
screeningulcerativecolitiscancers
Capsule Endoscopy versus Colonoscopy for the Detection of Polyps and CancerYour browser indicates if you’ve visited this link
The New England Journal of Medicine
ulcerativecolitis
Chattanoogan.com
screening
Colorectal Cancer Screening and EducationYour browser indicates if you’ve visited this link
Baylor College of Medicine
cancerscreeningScreeningcancercancer
Medscape
colitiscancerscancersulcerative
Don’t Miss: How To Test For Ulcerative Colitis
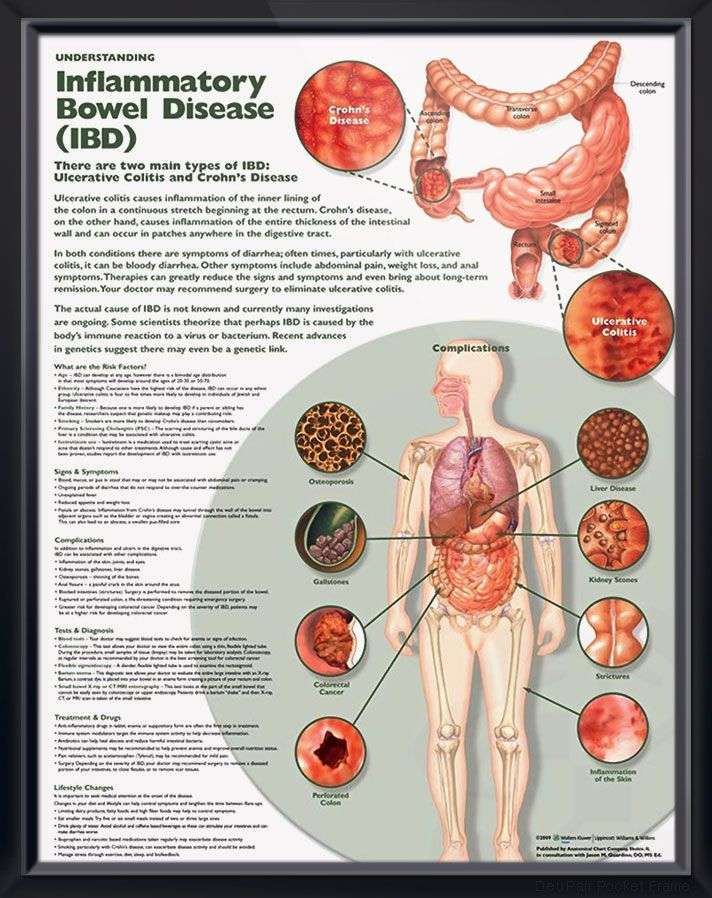
What Is Ulcerative Colitis
Ulcerative colitis is a chronic disorder affecting the large intestine . The digestive system converts food into nutrients and absorbs them into the bloodstream to fuel our bodies. The colons main role is to absorb water and salts from undigested food waste. This action helps to thicken and solidify the stool, which is then expelled from the body through the anus.
Ulcerative colitis causes inflammation and ulceration along the lining of the colon which can lead to abdominal pain, cramps, bleeding and diarrhea. The disease usually begins in the rectal area, which holds stool until you go to the bathroom, and may involve the entire colon over time. Ulcerative colitis is classified as an inflammatory bowel disease , due to the inflammation that occurs in the intestines. Another common form of IBD is called Crohns disease. Although the symptoms of ulcerative colitis are similar to Crohns disease, the conditions are different in several ways.
While both ulcerative colitis and Crohns disease are types of IBD, they should not be confused with Irritable Bowel Syndrome , a disorder that affects the muscle contractions and the sensitivity of the colon. Unlike ulcerative colitis and Crohns disease, IBS does not cause intestinal inflammation nor damage the bowel.
How Do I Spot The Signs And Symptoms Of Ulcerative Colitis
The most common symptoms of ulcerative colitis are abdominal pain and diarrhea, which often contains blood or pus.
Symptoms of the disease typically develop gradually and come and go.
Periods without active disease known as remission may last for months or even years.
Over time, ulcerative colitis can progress to cover more of the colon. This typically leads to more severe disease and greater symptoms.
If left untreated, UC can also lead to a number of complications, including:
- Malnutrition
Also Check: What To Eat To Help Stomach Ulcers
Surgical Approach: Laparoscopic Versus Open
Multiple randomized controlled trials have shown that laparoscopic colectomy is as good as the open approach in CRC in regard to the oncological results . The same has also been shown for rectal cancer . Therefore, also in UC, CRC can be operated by minimally invasive means without oncological disadvantage for the patient, provided the learning curve of laparoscopy has been overcome. Whether the typical short-term advantages as demonstrated for other laparoscopic colorectal procedures also hold true for restorative proctocolectomy remains controversial. Feasibility and safety of the laparoscopic approach have been shown in various studies nevertheless, clear evidence for the superiority of the laparoscopic compared to the conventional IPAA is not available. In 2009, a Cochrane review of 11 trials failed to demonstrate a difference between laparoscopic and open IPAA with regard to morbidity and mortality. However, some of the studies confirmed the most obvious advantage, i.e. a significantly improved cosmesis, if the patient had undergone laparoscopic surgery .
Fig. 4
Second postoperative day after laparoscopic restorative proctocolectomy .
Top Results For Ulcerative Colitis Colon Cancer Screening
topwww.cms.gov
cancer
Article – Billing And Coding: Colorectal Cancer Screening …
Copy the link and share
coloncancerscreeningulcerativecolitis
Colon Cancer Screening And Surveillance In Inflammatory …
Copy the link and share
ulcerativecolitisscreeningcancercancercolitis
Ulcerative Colitis And Colon Cancer: Risks, Screenings …
Copy the link and share
topwww.crohnscolitisfoundation.org
ulcerativecolitiscolonscreeningcancercancer
The Risk Of Colorectal Cancer In Crohn’s Disease And …
Copy the link and share
colitiscoloncolon
Ulcerative Colitis And Colonoscopy: Screening And More
Copy the link and share
greatwww.cancer.gov
coloncolonscreeningcolon
Screening Tests To Detect Colorectal Cancer And Polyps …
Copy the link and share
Also Check: Psc Liver Disease Ulcerative Colitis
How Colitis May Affect Your Cancer Risk
Signs and symptoms of colon cancer can be tougher to discern in ulcerative colitis patients. Blood in the stool, for example, which is a warning sign of cancer, may also happen as a result of a flare-up of the condition. The cancer itself is different, too, says Dr. Chang. Cancer in UC patients looks more like lesions, and less like masses or tumors, she says. But certain factors can increase your likelihood of developing cancer, including:
- The Severity of the Condition The longer you have uncontrolled inflammation, the more likely you are to develop dysplasia. Put another way, its not just having ulcerative colitis that ups your cancer risk its having uncontrolled UC that puts you in the danger zone.
- How Much of Your Colon is Affected If just the 5 to 10 centimeters of colon closest to the rectum is affected a condition called ulcerative proctitis your risk is similar to that of the normal population. If your entire colon is affected, your risk rises.
What To Expect During A Colonoscopy
About 24 hours before a colonoscopy, you will be asked to clear your bowels with laxatives, enemas, or an all-liquid diet. Be sure to follow the fasting instructions given to you by your healthcare provider.
On the day of the procedure, you will be asked to change into a hospital gown and given a sedative and pain medication, either orally by pill or intravenously . In most cases, you will be awake during the procedure.
Once sedated, your doctor will ask you to lie on your left side, insert the colonoscope through the rectum and use the tool to take pictures. They will also remove any polyps and tissue samples.
The procedure usually takes about 30 minutes, and then you will moved to a recovery room to allow the sedative to wear off. Typically, you will be able to go home the same day.
You May Like: Treating Hindgut Ulcers In Horses
Can I Prevent Ulcerative Colitis
There is currently no known way to prevent or cure for ulcerative colitis but the proper strategy for managing your disease can help you lead a happier, healthier, fulfilling life.
The exact cause of ulcerative colitis is unknown. However, it is believed to be due to a combination of factors, including a persons genes and triggers in the environment. This interaction of genetic and environmental factors activates an abnormal response of the bodys immune system.
Normally, the immune system protects the body from infection. In people with ulcerative colitis, however, the immune system can mistake microbes , food, and other material in the intestines, as invading substances.
When this happens, the body launches an attack, sending white blood cells into the lining of the intestines where they cause inflammation and ulcerations.