Get Support For Your Ibd Today
MyCrohnsAndColitisTeam is the social network for people diagnosed with IBD and the people who love, support, and care for them. More than 142,000 members come together to ask questions, give advice, and share their experiences of life with IBD.
Have you experienced chills with Crohns disease or ulcerative colitis? Share your experience in the comments below or by posting on MyCrohnsAndColitisTeam.
Stay Strong Ulcerative Colitis And Lower Back Pain
As soon as your lower neck and back pain has actually declined, you can aid avoid future episodes of pain in the back by functioning the muscular tissues that support your lower back, consisting of the back extensor muscles. They aid you keep the appropriate posture as well as alignment of your spine. Having solid hip, pelvic, and abdominal muscles additionally provides you extra back support. Avoid stomach crunches, because they can really put even more stress on your back.
Read Also: How Do They Treat Ulcerative Colitis
How Is Ulcerative Colitis Diagnosed
To diagnose ulcerative colitis in children, teenagers and adults, your healthcare provider has to rule out other illnesses. After a physical exam, your provider may order:
- Blood tests: Your blood can show signs of infection or anemia. Anemia is a low level of iron in your blood. It can mean you have bleeding in the colon or rectum.
- Stool samples: Signs of infection, parasites , and inflammation can show up in your poop.
- Imaging tests: Your healthcare provider may need a picture of your colon and rectum. You may have tests including a magnetic resonance imaging scan or computed tomography scan.
- Endoscopic tests: An endoscope is a thin, flexible tube with a tiny camera. Specialized doctors can slide the endoscope in through the anus to check the health of the rectum and colon. Common endoscopic tests include colonoscopy and sigmoidoscopy.
Read Also: What Foods To Avoid With Ulcerative Colitis
Stress May Be A Trigger Of Bowel Disease Symptoms
By Amy Norton, Reuters Health
4 Min Read
NEW YORK – People with inflammatory bowel disease commonly believe that stress can trigger their symptoms, and a new study suggests they may be right.
Canadian researchers found that among 552 bowel-disease patients they followed for a year, the risk of a symptom flare-up increased when patients were feeling particularly stressed.
The findings, reported in the American Journal of Gastroenterology, lend support to what many people with inflammatory bowel disease have believed to be true.
IBD refers to a group of conditions marked by chronic inflammation in the intestines, leading to symptoms like abdominal pain and diarrhea. The major forms are Crohns disease and ulcerative colitis.
The precise cause of the conditions is unclear, but they are thought to involve an immune system overreaction that injures the bodys own intestinal tissue. While stress does not cause IBD, it is one of the environmental factors suspected of triggering symptom flare-ups in some people.
Studies show that many people with IBD feel that stress worsens their symptoms, but there has been relatively little scientific evidence of that.
This is among the first evidence to show that the perception of stress had a direct association with disease course, Dr. Charles N. Bernstein, the lead researcher on the new study, told Reuters Health in an email.
When Youre In The Hospital
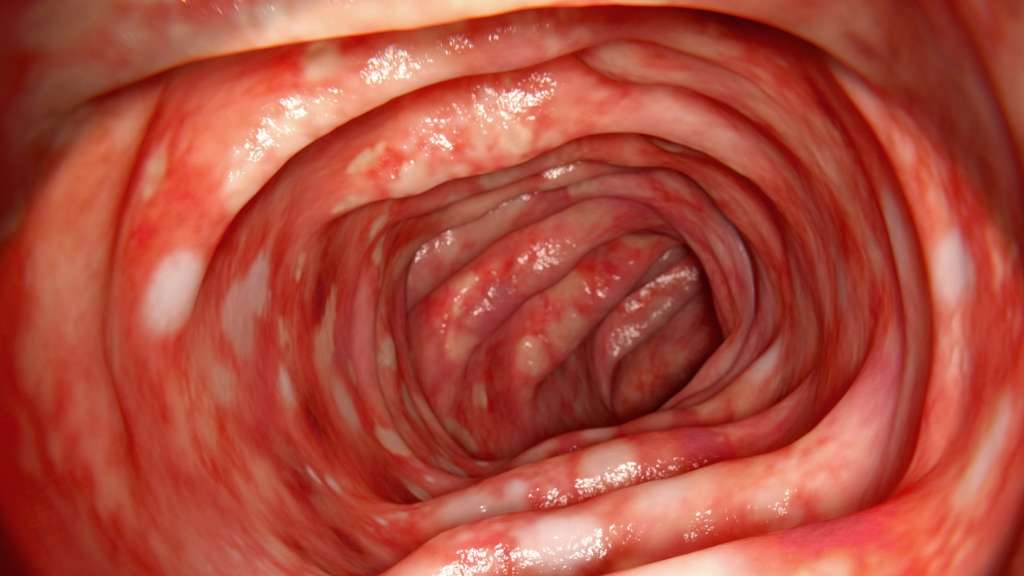
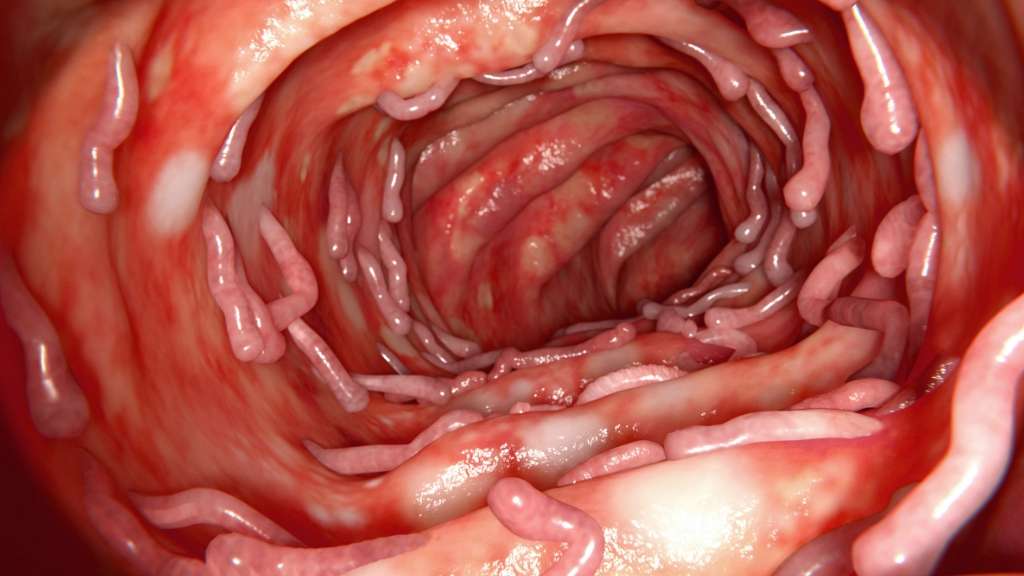
You were in the hospital because you have ulcerative colitis. This is a swelling of the inner lining of your colon and rectum . It damages the lining, causing it to bleed or ooze mucus or pus.
You probably received fluids through an intravenous tube in your vein. You may have received a blood transfusion, nutrition through a feeding tube or IV, and medicines to help stop diarrhea. You may have been given medicines to reduce swelling, prevent or fight infection, or help your immune system.
You may have undergone a colonoscopy. You also may have had surgery. If so, you may have had either an ileostomy or colon resection .
Also Check: New Meds For Ulcerative Colitis
Can I Treat Ibd If I Am Pregnant Or Breastfeeding
Yes, but your doctor may change the type or amount of the medicine you take. Some medicines, such as methotrexate and thalidomide, cause birth defects and other health problems and should not be taken while you are pregnant or breastfeeding.31
Before you get pregnant, make a plan with your obstetrician and gastroenterologist about the medicines you will take during and after pregnancy. Take your medicines as your doctor tells you to. If you stop taking your medicines and your symptoms come back , it may be difficult to get them back under control.31
Talk with your doctor about your medicines and breastfeeding before you give birth. You can search for your medicine in the LactMed database to find out if your medicine passes through your breastmilk and, if so, if it has any possible side effects for your nursing baby.
Also Check: How Do You Stop A Stomach Ulcer From Hurting
Treating Ibd And Anxiety
The study authors say it is important for physicians to determine whether patients with IBD also have a functional disorder. Differentiating symptoms between the two can be difficult, so they suggest that doctors first look for signs of inflammation, treat those, and then if symptoms remain it could indicate a functional disorder, at which point they should consider treatment for this disorder as well.
Physicians typically involved in caring for IBD patients, such as general practitioners and gastroenterologists, sometimes dont have much formal training in psychological disorders, and since patients are often hesitant to bring up psychological symptoms due to social stigma, they typically remain undiagnosed and untreated for too long. When IBD patients with an anxiety disorder experience stigma and therefore dont seek treatment, it can lead to further disability. It is very important that physicians are aware of the increased risk of anxiety in IBD patients, and should be prompt in detecting and treating any coexisting anxiety disorders. Patients also have a responsibility to speak up and ask for help if they perceive that anxiety is a problem for them.
If you are an IBD patient and are concerned that you might have anxiety or a functional gastrointestinal disorder, speak with your doctor.
First published in the Inside Tract® newsletter issue 195 2015
Email News Sign Up
Recommended Reading: What Is The Best Thing To Put On Leg Ulcers
Ulcerative Colitis And Colonoscopy
Doctors can use a colonoscopy to diagnose UC or determine the severity of the condition.
Before the procedure, a doctor will likely instruct you to reduce solid foods and switch to a liquid-only diet. Then youll fast for a period of time before the procedure.
Typical colonoscopy prep involves taking a laxative the evening before the procedure, too. This helps eliminate any waste still in the colon and rectum. Doctors can examine a clean colon more easily.
During the procedure, youll lie on your side. Your doctor will give you a sedative to help you relax and prevent any discomfort.
Once the medication takes effect, the doctor will insert a colonoscope into your anus. This device is long and flexible so it can move easily through your GI tract. The colonoscope also has a camera attached so your doctor can see inside the colon.
During the exam, the doctor will look for signs of inflammation and check for precancerous growth called polyps. The doctor may also perform a biopsy. The tissue can be sent to a laboratory for further examination.
If youve been diagnosed with UC, a doctor may conduct periodic colonoscopies to monitor inflammation, damage to your intestines, and healing progress.
These symptoms are sometimes associated with UC complications.
If you havent been diagnosed with UC, see a doctor if you experience multiple symptoms of the condition. They can help determine whether you may have UC or another bowel disease.
Find Your Support System
MyCrohnsAndColitisTeam is a community of more than 138,000 members who understand living with inflammatory bowel disease. Members share tips for managing flares and offer each other support and encouragement.
Do you struggle with UC flares? What has worked for you? Share your tips in the comments below, or on MyCrohnsAndColitisTeam.
Read Also: Signs And Symptoms Of Peptic Ulcer
Alternative Treatments For Managing Ulcerative Colitis Flare
Some people with ulcerative colitis feel better when they are on fish oil, probiotics, and herbal supplements. Alternative treatments such as acupuncture also work for some.
Some studies have investigated the impact of various formulations of cannabis on inflammation in IBD. Formulations of cannabis products can include CBD only, CBD with THC at various percentages, and THC alone. Cannabis was found to be effective in reducing symptoms of IBD, such as diarrhea and abdominal pain, but not in controlling inflammation associated with IBD.
Read MyCrohnsAndColitisTeams interview with Dr. Kinnucan to find out more about CBD oil and cannabis for IBD here.
Tips For Managing Anxiety When You Have Ulcerative Colitis
Learning how to cope with daily stressors will help manage UC-related anxiety.
Sam Cleasby was 23 years old when she was diagnosed with ulcerative colitis an inflammatory bowel disease that causes chronic inflammation and sores in the gut. Medication kept her flare-ups under control for nearly a decade. But in 2013, Cleasby required surgery to keep her disease under control. First, doctors removed her colon. Then they created an ileostomy, in which a piece of the small intestine is pulled through an opening in the abdomen so digested food can pass through a pouch called an ostomy bag, which she wears on the outside of her body. Later, they removed her entire large intestine.
Though I had times when life was tough and I was sad, frustrated, or angry, I didnt actually struggle with anxiety and my mental health until after surgery, says Cleasby, founder of the blog SoBadAss, who says she also suffers from post-traumatic stress disorder . It wasnt the surgeries themselves but the loss of control that was the source of my panic attacks and anxiety, explains Cleasby.
In addition to coping with their illness, people with UC have to manage doctors appointments, medication, and changes to their lifestyle and eating habits, says Mira Zein, MD, a psychiatrist with Stanford Health Care in California. Flare-ups can also put a damper on socializing.
Recommended Reading: Ulcerative Colitis Rectal Pain Relief
Coping With Stress And Ulcerative Colitis
To reduce ulcerative colitis flare-ups, it isnt always enough to take your medication and stick with your doctors treatment plan. Its can also be helpful to find ways to lower your stress level. Here are some strategies to help you manage stress:
Ways To Reduce Complications
Early intervention and frequent surveillance of ailments is key to reducing complications and improving outcomes. Its important to maintain proper nutrition and avoid emotional stress, though neither stress nor sensitivity to certain foods causes the disease. Avoiding steroids can also be helpful if you and your doctor have an alternative way of treating UC flares.
While the cure for UC has yet to be found, when the disease is treated properly, some complications may disappear altogether. Work with your doctor and other members of your healthcare team to get optimal control of the disease as soon as possible.
Additional reporting by Jordan M. Davidson.
You May Like: Homeopathic Medicine For Ulcerative Colitis
Southern Cross Medical Library
The purpose of the Southern Cross Medical Library is to provide information of a general nature to help you better understand certain medical conditions. Always seek specific medical advice for treatment appropriate to you. This information is not intended to relate specifically to insurance or healthcare services provided by Southern Cross. For more articles go to the Medical Library index page.
Dont Miss: Foods You Can Eat With An Ulcer
Speak With Your Doctor
Without treatment, people with UC tend to relapse.
For many people with mild or moderate symptoms, things improve somewhat after diagnosis. This is thanks to medication, along with identifying and avoiding triggers.
More aggressive cases are less common, and only a small number of severe cases will require hospitalization.
Repeated flare-ups can indicate problems with your current treatment, so speak with your doctor and discuss adjusting your medication.
Several classes of medication now exist that can help you get into and stay in remission. Your doctor may need to add another type or increase your dosage.
The only way to prevent UC flare-ups is to have surgery. The most common type of UC surgery is the proctocolectomy, which involves the removal of the rectum and colon.
Candidates for UC surgery include people who:
- have sudden or severe disease
- have a perforated colon
- are at risk for colorectal cancer
- are unable to tolerate their UC medications due to side effects
- have stopped responding to their UC medications
In addition to knowing how to manage flare-ups, its also helpful to recognize factors that can trigger your flare-ups.
Don’t Miss: How To Heal Mouth Ulcers Fast
Cut Out Raw Veggies And Other Gut Irritants
In the midst of a ulcerative colitis flare, you want to be as gentle on your digestive system and colon as possible. Give your gut a little vacation, says Cohen. This ideally means eliminating or scaling back on: raw vegetables, raw and cooked fruits, high-fat foods , high fiber foods , spicy foods, alcohol, and caffeinated beverages. Basically, any food that takes significant digestive effort or stimulates the bowels.
General Causes Of Ulcerative Colitis
The exact cause for ulcerative colitis continues to be not acknowledged. However, researchers link the sickness to:
- A combination of environmental factors.
- A system that is awry.
- Genetic predisposition.
- A microorganism or microorganism infection within the colon, that initiates uncontrolled inflammation that is closely joined to colitis.
The condition may additionally be aggravated by the sort of diet and stress. For example consumption of Trans fats in masses will increase the danger of the condition. These fats square measure chiefly in processed foods. On the opposite hand, the intake of Omega -3 fatty acids in massive quantities lowers the danger of developing the condition.
Read Also: How To Get Remission In Ulcerative Colitis
Also Check: How Is Ulcerative Colitis Caused
Etiology Of Ulcerative Colitis
The exact cause of ulcerative colitis is unknown. The most accepted theory about its etiology is that ulcerative colitis is an autoimmune disorder. Also, genetic and environmental factors play a role.
Unlike Crohns disease, smoking doesnt represent a risk factor in ulcerative colitis. The incidence of ulcerative colitis is lower among smokers 80% of the patients are nonsmokers.
Page 2 of 18
Recommended Reading: Advil Or Ibuprofen For Back Pain
What To Do If Your Flare
Stress management goes a long way in supporting your overall mental and physical health, but sometimes stress management alone just isnt enough. If youre struggling with flare-up after flare-up, we can help.
Here at Atlantic Medical Group, its our mission to help you get the relief you need so you can live the life you want. For troublesome cases that dont respond to medication, we may suggest surgery.
To explore your treatment options for Crohns disease or colitis, our Kinston or Jacksonville, North Carolina, office today. You can also visit us online to request an appointment.
You Might Also Enjoy…
Recommended Reading: Can Ulcerative Colitis Cause Low Testosterone
Colon Cancer And Ulcerative Colitis
When you have ulcerative colitis, you may be more likely to get colon cancer. Your chances go up if you dont get treatment for UC. Thats because unchecked inflammation can cause changes in the cells in your colon. These cells may turn into cancer down the road.
Your chances of getting colon cancer go up if youve had ulcerative colitis for 8 years or longer. The odds are also higher if:
- Your inflammation doesnt go away.
- Youre a man.
- You have a liver condition called primary sclerosing cholangitis.
- You have a family member whos had colon cancer.
Some research shows that people with UC may be less likely to get colon cancer now than in the past. Experts think its because doctors now have better ways to screen for colon cancer and they do it more often. It also helps that new medicines, like biologics, do a good job of curbing inflammation.
The Role Of Peripheral Substance P

In addition to its central effects, peripheral release of SP from the ENS may have a role in stress induced increases in mucosal inflammation. Although there are no published data to show an increase in mucosal SP in response to stress, SP containing neurones are found in close association with mast cells, a cell type implicated as central in mediating stress induced permeability changes . SP has been shown to increase histamine release from mucosal mast cells in patients with IBD. Lastly, SP can act not only as a neurotransmitter but also an inflammatory cytokine in its own right, enhancing cytokine production and stimulating chemotaxis of inflammatory cells. It also increases expression of leucocyte adhesion molecules on microvascular endothelium, and of CD11b on neutrophils, facilitating leucocyte adhesion at sites of inflammation.
You May Like: Are Eggs Bad For Ulcerative Colitis