What Are The Best Practices In Pressure Ulcer Prevention That We Want To Use
Once you have determined that you are ready for change, the Implementation Team and Unit-Based Teams should demonstrate a clear understanding of where they are headed in terms of implementing best practices. People involved in the quality improvement effort need to agree on what it is that they are trying to do. Consensus should be reached on the following questions:
In addressing these questions, this section provides a concise review of the practice, emphasizes why it is important, discusses challenges in implementation, and provides helpful hints for improving practice. Further information regarding the organization of care needed to implement these best practices is provided in Chapter 4 and additional clinical details are in Tools and Resources.
In describing best practices for pressure ulcer prevention, it is necessary to recognize at the outset that implementing these best practices at the bedside is an extremely complex task. Some of the factors that make pressure ulcer prevention so difficult include:
Data Analysis And Synthesis
2.4.1. Availability analysis
For the purpose of analysis, we considered each hospital individually, rather than considering their health networks. This was because some hospitals provided information for their hospital’s services with PIs in their hospitals’ sections of their health network’s site, but not in others, and a patient would ostensibly first look to the hospital’s own site, rather than a health network’s site. We assessed availability by checking if the site presented either the information on PIs for patients or if they had information on where a patient could get information directly from the hospital .
To assess the comparative likelihood of having PI materials on their sites, a chisquare test was chosen. We chose to compare the likelihood of having materials between hospital funding status and between proximity to metropolitan centres as two separate chisquare tests.
2.4.2. Content analysis
The first author conducted a pilot round of coding of the nonrandomly selected three educational materials and developed the analytical framework. The developed framework and the materials were shared with other coauthors, who reviewed, made final adjustments, and approved this framework. Two authors independently analysed all included materials using the developed analytical framework.
When You Are In Bed
Use a foam mattress or one that is filled with gel or air. Place pads under your bottom to absorb wetness to help keep your skin dry.
Use a soft pillow or a piece of soft foam between parts of your body that press against each other or against your mattress.
When you are lying on your side, put a pillow or foam between your knees and ankles.
When you are lying on your back, put a pillow or foam:
- Under your heels. Or, place a pillow under your calves to lift up your heels, another way to relieve pressure on your heels.
- Under your tailbone area.
- Under your shoulders and shoulder blades.
- Under your elbows.
Other tips are:
- DO NOT put pillows under your knees. It puts pressure on your heels.
- Never drag yourself to change your position or get in or out of bed. Dragging causes skin breakdown. Get help if you need moving in bed or getting in or out of bed.
- If someone else moves you, they should lift you or use a draw sheet to move you.
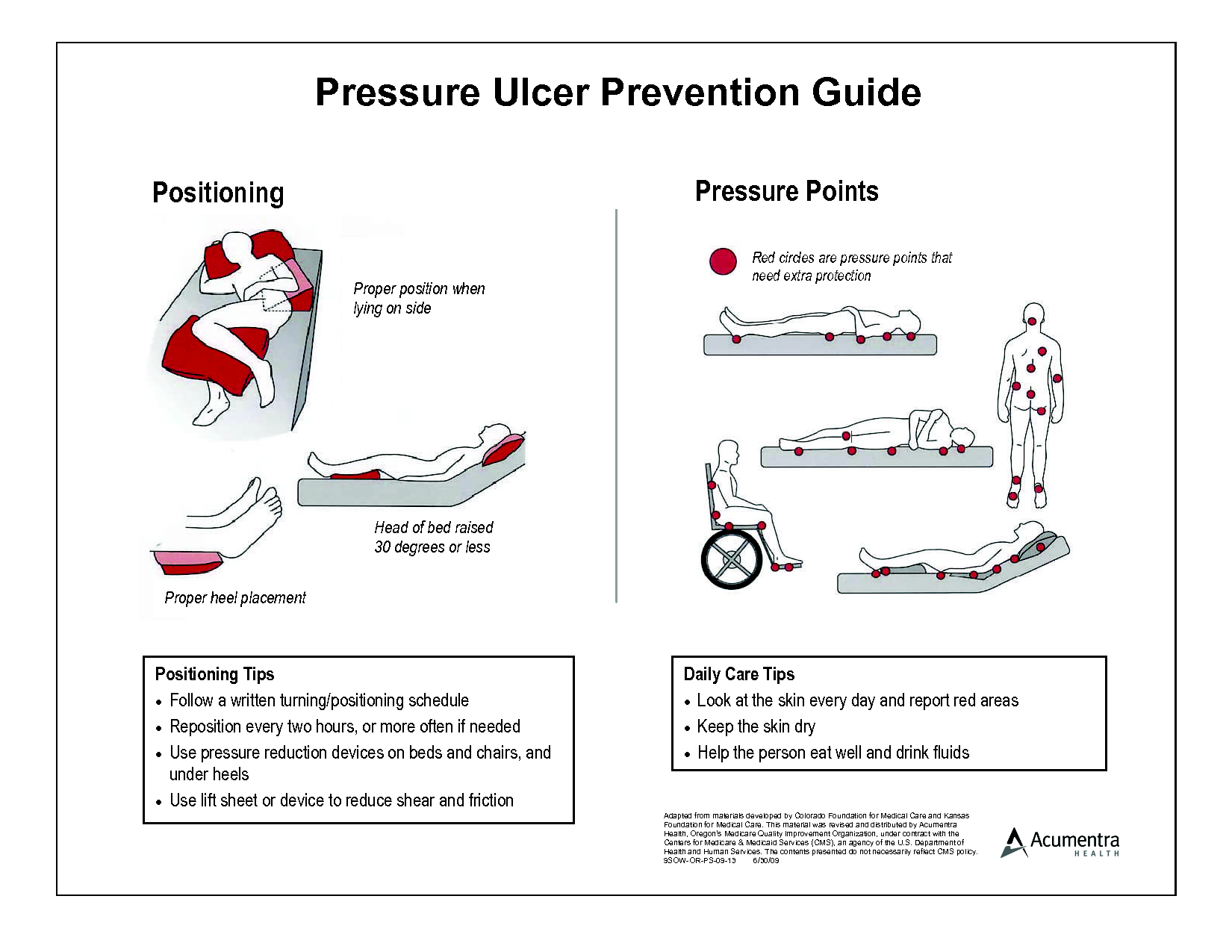
- Change your position every 1 to 2 hours to keep the pressure off any one spot.
- Sheets and clothing should be dry and smooth, with no wrinkles.
- Remove any objects such as pins, pencils or pens, or coins from your bed.
- DO NOT raise the head of your bed to more than a 30 degree angle. Being flatter keeps your body from sliding down. Sliding may harm your skin.
- Check your skin often for any areas of skin breakdown.
Read Also: Homeopathic Medicine For Ulcerative Colitis In Hindi
If You Use A Wheelchair
Make sure your wheelchair is the right size for you.
- Have your doctor or physical therapist check the fit once or twice a year.
- If you gain weight, ask your doctor or physical therapist to check how you fit your wheelchair.
- If you feel pressure anywhere, have your doctor or physical therapist check your wheelchair.
Sit on a foam or gel seat cushion that fits your wheelchair. Natural sheepskin pads are also helpful to reduce pressure on the skin. DO NOT sit on a donut-shaped cushions.
You or your caregiver should shift your weight in your wheelchair every 15 to 20 minutes. This will take pressure off certain areas and maintain blood flow:
- Lean forward
- Lean to one side, then lean to the other side
If you transfer yourself , lift your body up with your arms. DO NOT drag yourself. If you are having trouble transferring into your wheelchair, ask a physical therapist to teach you the proper technique.
If your caregiver transfers you, make sure they know the proper way to move you.
Risk Factors For Pressure Sores
A pressure sore is caused by constant pressure applied to the skin over a period of time. The skin of older people tends to be thinner and more delicate, which means an older person has an increased risk of developing a pressure sore during a prolonged stay in bed.
Other risk factors for pressure sores include:
- immobility and paralysis for example due to a stroke or a severe head injury
- being restricted to either sitting or lying down
- impaired sensation or impaired ability to respond to pain or discomfort. For example, people with diabetes who experience nerve damage are at increased risk of pressure sores
- urinary and faecal incontinence skin exposed to urine or faeces is more susceptible to irritation and damage
- malnutrition can lead to skin thinning and poor blood supply, meaning that skin is more fragile
- obesity being overweight in combination with, for example, immobility or being restricted to sitting or lying down can place extra pressure on capillaries. This then reduces blood flow to the skin
- circulation disorders leading to reduced blood flow to the skin in some areas
- smoking reduces blood flow to the skin and, in combination with reduced mobility, can lead to pressure sores. The healing of pressure sores is also a slower process for people who smoke.
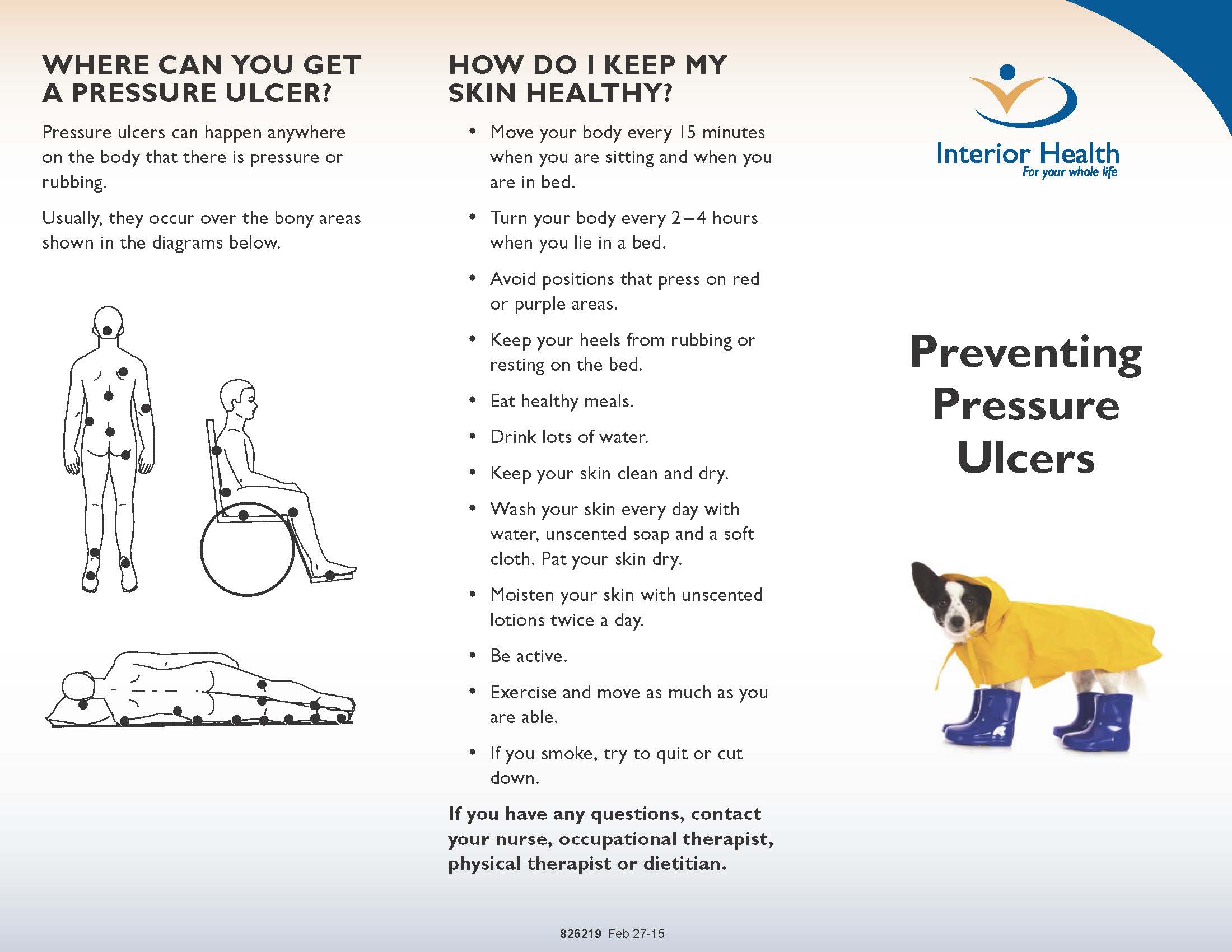
If youre bedridden, pressure sores can occur in a number of areas, including:
- back or sides of the head
- rims of the ears
- backs or sides of the knees
- heels, ankles and toes.
You May Like: Can I Take Tylenol With An Ulcer
Pressure Ulcer Risk Assessment
A person is at risk for pressure ulcers if s/he…
- Is in a bed or chair for eight hours or more excluding sleeping
- Has urine or fecal incontinence
- Has a chronic medical condition
- They already have redness or pain in pressure ulcer areas: such as sacrum, trochanter, scapulae, elbow, heel, inner and outer malleolus, inner and outer knee, back of the head
- Has trouble getting enough calories or fluids every day
- Is already under-nourished
Inclusion And Exclusion Criteria
Information on PIs available on the hospital and health services’ websites, including pamphlets, booklets, leaflets, and online information, was included in the analysis. We included all available information on PI prevention and management, including booklets developed by hospitals for admitted patients on admission. Information on PIs for health professionals and information presented as part of hospital reports and educational courses on PI for health professionals was excluded.
Also Check: What Does A Venous Leg Ulcer Look Like
Pressure Ulcer Prevention: Home Health Careplan & Teaching
Posted byMelissa Cott on Apr 14, 2022
Any person who is in a bed or chair for 8 hours or longer is at risk for pressure ulcers. Pressure ulcers – also known as bed sores, decubitus ulcers, pressure sores and skin ulcers – often develop in patients with the following conditions: diabetes mellitus, deep venous thrombosis, s/p hip fracture, s/p hip surgery, limb paralysis, dependent edema, cancer, malnutrition, osteoporosis, Parkinsons disease, rheumatoid arthritis, and urinary tract infections. In addition, patients with Alzheimers disease, congestive heart failure, chronic obstructive pulmonary disease, and c/p cerebral vascular accident are at risk for pressure ulcers.
When Should I Call The Doctor
If you suspect you have a pressure injury, speak with your doctor. A pressure injury is easier to heal if it is discovered in the early stages. It is important to prevent a wound from becoming infected. Healing is delayed in an infected wound and the infection could cause problems in other areas of the body.
You May Like: Can Ulcerative Colitis Lead To Crohn Disease
Take Care Of Your Skin
Taking care of your skin and doing regular skin checks are important in preventing pressure sores. Check your skin at least once a day for redness, changes in colour, blisters, bruises, cracked, scraped or dry skin. Closely inspect areas that are at especially high risk for pressure sores. The highest risk is where your bones are close to the surface and your skin is directly over bone. Use a mirror to inspect skin in hard-to-see areas or ask your caregiver to help you. If you notice a discolored area, stay off the area until it returns to normal skin colour.Keep your skin at the right moisture level, as damage is more likely to occur if your skin is either too dry or too moist. Use moisturising products to keep your skin supple and prevent dryness, but avoid massaging bony areas where the skin is too delicate. Immediately wash and dry skin and change clothing after any leakage of stool or urine . Avoid harsh soaps, skin agents with alcohol and antibacterial or antimicrobial soaps.
Empowering Patients To Play An Active Role In Pressure Ulcer Prevention
Developing a pressure ulcer can cause the patient pain, lead to social isolation, result in reduced mobility, and can even be fatal. According to the Agency for Healthcare Research and Quality, estimated costs for each pressure ulcer range from $37,800 to $70,000, and the total annual cost of pressure ulcers in the United States is an estimated $11 billion.
Nurses understand their role in preventing pressure ulcers, but what role do patients play in the prevention plan? Nurses need to empower the patient to be an active member in health promotion activities and participate in prevention measures. In this article, I highlight the importance of incorporating pressure ulcer prevention into patient education for high-risk patients as a way to empower patients. Empowered patients can help improve outcomes and reduce overall costs of this hospital-acquired complication.
Patient engagement
A basic element of empowerment is engagement. Nurses must practice a patient-centered approach to healthcare delivery that embraces and supports the belief that patients are, or can become, competent to make informed decisions. Engaged patients tend to function better, experience fewer symptoms, and are less likely to experience an adverse event compared to those who arent engaged.
The value of teach-back
Integrating into care
Promoting engagement
ulcers.
Hannah Miller is a clinical learning lab specialist at Chamberlain College of Nursing in Cleveland, Ohio.
Don’t Miss: What Do You Do For An Ulcer In Your Stomach
Who Is At Risk For Developing Pressure Injuries
- People with a limited amount of mobility or a total inability to move. Those in wheelchairs or bedridden are at particular risk and need to be moved or turned regularly.
- Those with prosthetic limbs. If the device does not fit properly, the skin can be irritated and a pressure injury can develop.
- People with a loss of sensation. They are at risk because they may not feel the pressure being applied to the skin. As a result, they may not move, which could worsen the damage.
- Those with malnutrition. Wound healing is slowed when nutritional needs are not met.
- The elderly. As people age, the skin naturally becomes thinner and more easily damaged.
Preventing Pressure Ulcers In Hospitals
Each year, more than 2.5 million people in the United States develop pressure ulcers. These skin lesions bring pain, associated risk for serious infection, and increased health care utilization. The aim of this toolkit is to assist hospital staff in implementing effective pressure ulcer prevention practices through an interdisciplinary approach to care.
Prepared by: Dan Berlowitz, M.D., M.P.H. Bedford VA Hospital and Boston University School of Public Health Carol VanDeusen Lukas, Ed.D. VA Boston Healthcare System and Boston University School of Public Health Victoria Parker, Ed.M. D.B.A. Andrea Niederhauser, M.P.H. Jason Silver, M.P.H. and Caroline Logan, M.P.H. Boston University School of Public Health Elizabeth Ayello, Ph.D., RN, APRN, BC, CWOCN, FAPWCA, FAAN, Excelsior College School of Nursing, Albany, New York and Karen Zulkowski, D.N.S., RN, CWS, Montana State University-Bozeman.
You May Like: Best Way To Treat Ulcers In Horses
Availability Of Any Information On Pis
In total, our search yielded 23 sources of PI patient education materials, including brochures, leaflets, static websites , pamphlets, and a video clip .1). Figure Figure11 shows the availability of patient education materials in relation to hospital funding and location. The results show more than half of the hospital websites accessed did not contain any information for patients on prevention and management of PIs, indicating that only 71 of the 212 hospitals had these materials. Private hospitals were more likely to have patient information about PIs on their website than public hospitals . A chisquare test showed that there was a statistically significant association between the hospital type and the likelihood of having PI material on their website, 2 = 26.31, P< .001. Similarly, metropolitan hospitals were more likely to have PI materials on their websites compared to rural hospitals , and the association between the location type and PI educational material availability was statistically significant 2 = 24.37, P< .001.
Position Changes To Prevent Pressure Sores
If you use a wheelchair shift position within your chair about every 15 minutes. If you spend most of their time in bed change position at least once every two hours, even during the night and avoid lying directly on your hipbones.
Pillows may be used as soft buffers between your skin and the bed or chair. The head-of-bed elevation should be maintained at/or below 30 degrees. Or depending on the your medical condition, the bed should at least be elevated to the lowest degree to prevent injury. When lying on your side, a 30 degrees position should be used.
Recommended Reading: Cheap Ulcer Treatment For Horses
Causes Of Pressure Sores
Pressure sores happen if you cant move around and so stay in one position for a long time. We normally move about constantly, even in our sleep. This stops pressure sores developing.
People who are unable to move around tend to put pressure on the same areas of the body for a long time. If you are ill, bedridden or in a wheelchair, you are at risk of getting pressure sores.
A number of things can increase your risk of pressure sores, including:
- being unable to move around easily due to old age or illness
- weight loss – you may have less padding over bony areas
- sliding down in a bed or chair – pressure on the skin cuts off blood supply because the skin is being pulled in different directions
- friction or rubbing of the skin, for example against sheets
- a poor diet
- moist skin – for example, due to sweating or incontinence
- other medical conditions, such as diabetes
- having a previous pressure ulcer
Use Pillows Cushions Or Special Mattresses
Using pillows or cushions as soft buffers between your skin and the bed or chair can be helpful. No two skin surfaces should rest against each other, eg, while lying in bed, place a pillow between your knees and ankles to prevent them from touching each other. If you are confined to bed, ask your healthcare provider about the use of heel and knee protectors or pressure relieving mattresses.
Also Check: Do Ulcers Hurt All The Time
Study Design And Methods
We conducted availability analysis of PI educational materials located on the web pages of health services and hospitals in Victoria, Australia. We then explored the relationship between the availability of PI materials and a range of factors including the funding status of the hospital and location using two separate chisquare tests. We also conducted a qualitative content analysis to evaluate the accuracy of information about PI prevention and management. This method is increasingly used in nursing and health promotion to analyse the content of patient education materials in various health fields.53, 54
Pressure Injury As A Public Health Issue
Pressure injury , also known as a pressure ulcer, was defined as a localised injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear,1. PI imposes a significant economic and social burden to Australia2 and globally.3, 4, 5, 6 The National Pressure Ulcer Advisory Panel, the European Pressure Advisory Panel, and the Pan Pacific Pressure Injury Alliance1 categorise PIs into six clinical stages and acknowledge the increase of the negative health impacts with the depth of the PI. One of the most common forms of PI are hospital acquired pressure injuries , defined as an area of damage to the skin/underlying tissue that develops during an inpatient hospital stay.7 From 2015 to 2016, the approximate rate of HAPIs in Australia totalled 9.7 injuries per 10000 hospitalisations.8 The Australian Commission on Safety and Quality in Healthcare9 has identified HAPIs as a serious and preventable hospitalacquired complication. Prevention and management of HAPIs is addressed in the Australian National Safety and Quality Health Service Standards.9
Don’t Miss: Best Prebiotic For Ulcerative Colitis
How Should A Standardized Pressure Ulcer Risk Assessment Be Conducted
As discussed above, one purpose of comprehensive skin assessment is to identify visible changes in the skin that indicate increased risk for pressure ulcer development. However, factors other than skin changes must be assessed to identify patients at risk for pressure ulcers. This can best be accomplished through a standardized pressure ulcer risk assessment.
3.3.1 What is a standardized pressure ulcer risk assessment?
After a comprehensive skin examination, pressure ulcer risk assessment is the next step in pressure ulcer prevention. Pressure ulcer risk assessment is a standardized and ongoing process with the goal of identifying patients at risk for the development of a pressure ulcer so that plans for targeted preventive care to address the identified risk can be implemented. This process is multifaceted and includes many components, one of which is a validated risk assessment tool or scale.
Other risk factors not quantified in the assessment tools must be considered. Risk assessment does not identify who will develop a pressure ulcer. Instead, it determines which patients are more likely to develop a pressure ulcer, particularly if no special preventive interventions are introduced. In addition, risk assessment may be used to identify different levels of risk. More intensive interventions may be directed to patients at greater risk.
Action Steps
Ask yourself and your team:
3.3.2 Why is a pressure ulcer risk assessment necessary?
Action Steps
Ask yourself and your team: