Ulcerative Colitis And The Paleo Diet
Ulcerative colitis and diet
Ulcerative colitis is an inflammatory bowel disease that causes cramping and chronic diarrhea. It can often be managed with medication, but paying attention to your diet is also important. Triggers like certain foods and beverages and stress can worsen symptoms. Triggers vary from person to person, and theres no evidence that specific foods cause ulcerative colitis. However, diets that limit certain foods may alleviate symptoms. One such diet is the popular paleo diet.
Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms can vary, depending on the severity of inflammation and where it occurs they typically develop over time. Most people experience mild to moderate symptoms, but the course of ulcerative colitis may vary and some people have long periods of remission. The symptoms depend on the location of the disease-causing inflammation. If you have ulcerative colitis, you may have the following signs and symptoms:
- Diarrhea, often with blood or pus
- Abdominal pain and cramping
- An increased risk of blood clots in veins and arteries
How Can I Track Foods That Cause Flare
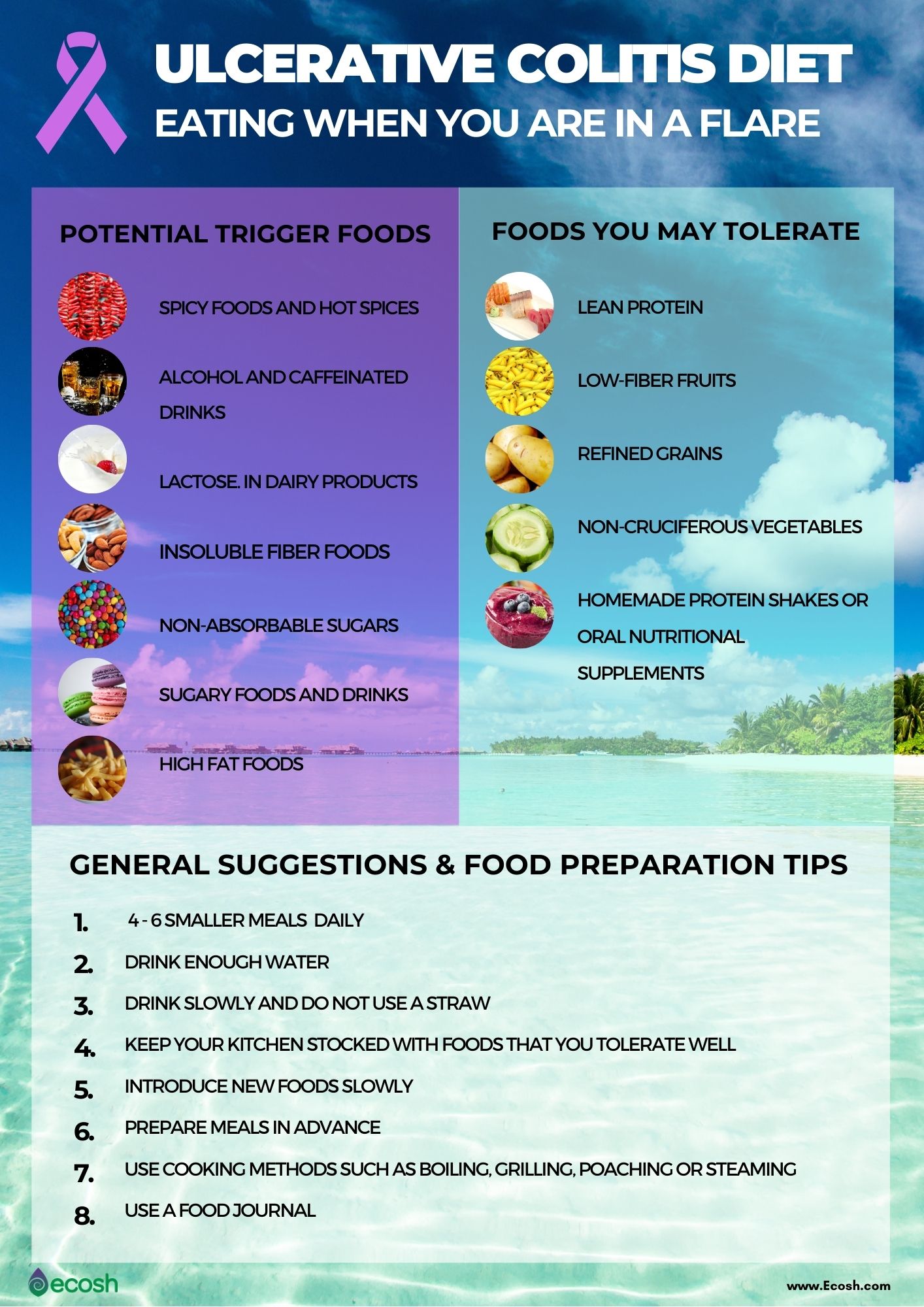
The Crohn’s and Colitis Foundation of America recommends people with ulcerative colitis keep a food journal to keep track of what they eat. Note what you eat and drink, and how you feel afterward, noting any symptoms that arise. Start to keep a list of any foods you suspect may trigger or aggravate your ulcerative colitis symptoms. A food diary will also help you figure out if you are getting adequate nutrition, and can help your doctor or dietician determine the right diet for you to manage your symptoms and prevent flares.
The Crohn’s and Colitis Foundation of America also has an interactive food tracking tool. It is available online or as a mobile app. www.ccfa.org/gibuddy
Also Check: Medication For Ulcerative Colitis Flare Up
What Types Of Diets Should I Consider
Both experts agree that everyones ulcerative colitis symptoms, triggers, and treatments are different, but there are certain eating styles that may be worth considering.
Talk with a health professional about whether one of these diets could be beneficial for you.
FODMAP is an acronym for types of carbohydrates that are poorly absorbed in the small intestine, specifically:
- Fermentable
Some health care providers may counsel their patients to try a FODMAP elimination diet during an UC flare, followed by reintroduction of FODMAP foods once in remission.
What does that mean for actually eating food? Well, you may want to try swapping high-FODMAPs like cauliflower, mushrooms, dried fruit, cows milk, and legumes for low-FODAMPs like eggplant, carrots, grapes, potatoes, eggs, quinoa, and tofu.
The Mediterranean diet is widely considered to be one of the worlds healthiest eating patterns for people with and without chronic conditions.
Characterized by a high consumption of fruits, veggies, whole grains, lean proteins, and healthy fatshello, olive oil and fish the Mediterranean diet has been linked with increased diversity of the gut microbiome9. Good news for people with IBD, since diversity in the gut bacteria could help to ease symptoms.
While you may have heard of the paleo diet, the autoimmune protocol diet , which is considered to be similar to the paleo diet, may have some benefits for people with IBD.
How Can Diet Help Uc
There is no single best diet for UC. Finding the right diet can help a person with UC lessen the occurrence of flares, improve their quality of life, and ensure proper nutrition.
People with UC, and other autoimmune conditions, widely use the elimination diet. This type of diet involves omitting certain foods or food groups that people believe to be causing the adverse reactions or food intolerance and gradually reintroducing them. About of people use this type of diet when in remission.
A showed that random food elimination could cause nutritional deficiencies. However, appropriate supplementation and monitoring from doctors can reduce this risk.
You May Like: Is Garlic Good For Ulcerative Colitis
Full Disclosure On My Paleo Bias
Yes, Im biased as far as meat and a Paleo eating model.
My Paleo bias is based on the fact that the basic Paleo diet and lifestyle model works for many health problems.
I was writing about the Paleo diet and UC as far back as 2010. I wrote my first Paleo book in 2011 and had a regular column in Paleo Magazine as early as 2012.
For more than a decade, my work has been read in print and online, in some of the most popular health and fitness magazines and websites.
Later, I co-authored a book that was a compilation of stories written by women who had managed and healed all kinds of health issues with a Paleo-based diet model.
Ive seen this eating template work for virtually everyone who tries it seriously, practices it consistently and modifies it for individual health conditions and preferences.
Paleo is diet genre and model.
There are a number of variations and permutations of a Paleo eating style. Its an adaptable model that can help us make sense of modern healing challenges.
Dont get hung up on the name or the dogma. The basic idea is to evaluate eating and living choices based on the types of foods and activities we had available to us through the majority of our evolution.
Natural Intestinal Healing Remedies
Due to the common complaints associated with medications and surgery, research has uncovered many natural options for healing a damaged digestive system. From lifestyle changes, dietary adjustments, and stress reduction techniques, ulcerative colitis can not only be prevented, but it can also be successfully healed.
One additional benefit is that many people, especially the elderly, cannot tolerate many medications. Natural options allow for healing without additional pain. These include:
Regular Exercise: Exercise is beneficial to your overall health, but when it comes to ulcerative colitis, regular activity can help with many of the complications associated with the condition. Studies have shown that individuals with ulcerative colitis also suffer from decreased bone density, emotional health problems, weight gain, and suppressed immune system.
| Related: Why a Workout Plan Improves the Benefits of Probiotics |
Exercise can help boost moods, promote weight loss, boost energy levels, and support bone health. In addition to this moderate exercise triggers the release of specific chemicals called myokines that promote healing from inflammatory-related damage.
Yoga is a specific exercise that takes care of the digestive system and provides relief for many ulcerative colitis symptoms.
Stress Reduction: Stress and anxiety are intricately linked to inflammation. The release of inflammatory chemicals is a direct result of the body experiencing stress.
Also Check: What Foods Irritate An Ulcer
Eating When You Are In Remission
While theres no cure for UC, you may experience periods of remission. During this time, youll be symptom-free and your UC wont interfere with your daily life.
Theres no definitive way to avoid flare-ups forever, but you can prolong your remission periods by maintaining a diverse and nutrient-rich diet that does not include trigger foods.
To stay symptom-free, it may be helpful to follow one of the diets that other individuals with UC find successful, as well as introduce new foods slowly and stay hydrated.
However, its important to consult with your doctor or dietician before making any changes to your diet.
Some foods that may help keep you feeling good and hydrated during remission
Nutrition And Ulcerative Colitis
There is no special diet for people with Ulcerative Colitis . This means that research has not shown any particular foods to either help or worsen disease activity.
However, ensuring good nutrition is an important part of managing UC.
People with UC are at risk for developing malnutrition and nutrient deficiencies. Poor nutrition makes it more difficult for your body to heal and fight infection. Malnutrition may also cause you to feel tired.
There are several reasons why people with UC may be at risk for poor nutrition, including:
|
So, people with UC should follow a balanced diet and be sure to get enough calories, protein, vitamins, minerals, and fluid. No specific foods must be avoided, but some people may notice that certain foods cause discomfort. If this is true for you, avoid these foods. Nutrition needs vary from person to person, so it is best to meet with a Registered Dietitian who can help you individualize your diet.
Calories and Protein
Vitamins and minerals
Low Fiber/Low Residue: Is it necessary?
What about the special diet I read about?
Special Situations
Lactose intolerance
Strictures, partial obstruction, or narrowed areas of bowel
Additional Resources
Also Check: How To Treat Venous Stasis Ulcers
Tips For Meal Prepping
Now that you have a sense of what to eat for ulcerative colitis, its time to get in the kitchen. Meal prepping some simple ingredients can make your life easier and prevent a UC flare. Here are some simple strategies:
- Buy pre-chopped fruits and veggies. Having produce in your fridge that dont require any preparation will make you more likely to add them to your plate at mealtime.
- Go frozen. Frozen fruits, veggies, and whole grains are generally as nutritious as fresh produce. Buy frozen fruit for smoothies, frozen veggies for soups and casseroles, and frozen grains to heat up in the microwave as a side dish.
- Pick up ready-made proteins. Stock up on simple options, like a rotisserie chicken or canned beans.
- Make a big batch of soup. Not only is soup soothing, its also an easy way to add a ton of veggies to your diet and is super easy to make in big batches.
- Stock up on healthy fats. Load up your cabinet with nuts, oils, and seeds for snacking, cooking, or adding texture to a recipe.
Recommended Diet For Lymphocytic Colitis
Lymphocytic colitis occurs when all or part of your large or small intestines becomes inflamed. Symptoms include fecal incontinence, abdominal pain, watery diarrhea, weight loss and nausea. After performing a colonoscopy or flexible sigmoidoscopy to properly diagnose you with this condition, your doctor will recommend that you to alter your diet in addition to treating you with anti-inflammatory drugs and anti-diarrhea medications.
Video of the Day
Don’t Miss: Wound Care For Stage 4 Pressure Ulcer
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
What Other Conditions Can Cause Urgency And Incontinence
Accidental bowel leakage can happen because of weakness to the anal sphincter or damage to the muscles in the pelvic floor. This can result from trauma during childbirth or surgery, among other causes. Problems with feeling the sensation of rectal fullness causes some cases of incontinence. Bowel disturbances can cause accidental bowel leakage. One example is when chronic constipation leads to overflow diarrhea.
You May Like: Best Wound Care For Stage 2 Pressure Ulcer
Ulcerative Colitis Diet: What To Eat To Manage Symptoms
Ulcerative colitis is a type of inflammatory bowel disease in which the immune system is thought to attack the gut lining, failing to recognise it as part of the body. A focused ulcerative colitis diet may therefore help with the management of symptoms. With the guidance of an IBD team or a dietician, those suffering from ulcerative colitis can be put on an elimination diet in order to identify potential trigger foods, or may be encouraged to keep a food diary in order to track links between certain foods and symptoms.
Those who have undergone surgery or are struggling with an ulcerative colitis flare up may be put on a low residue diet or a low fiber diet in order to manage symptoms and lessen the burden of their disease.
However, ulcerative colitis diets are often unique to the individual, so some experimentation under medical supervision may be necessary to find the right eating pattern for you. An ulcerative colitis diet may not work at all either, so it is important to collaborate with your medical team in order to properly manage your condition.
Do You Suffer From Ulcerative Colitis Discover How You Can Cure Ulcerative Colitis
Ulcerative Colitis can now be cured, not just treated! It is not the norm to hear that you can be cured, we think of remission as the only possibility. But this book is not about remission. It is about a curing Ulcerative Colitis. This is possible because over the last 10 years I discovered the true cause of Colitis and the raw materials that the body requires to heal and come back into balance. I have also discovered the ideal colitis diet that supports and helps heal the inflammation and not cause further damage to the colon. Once the true cause was found the cure became obvious. But does it work? Discovery of the cause and cure of Ulcerative Colitis has stood the test of time and here it is!
The step by step instructions including supplementation, Herbs, diet and lifestyle changes that will heal your condition in 90 days or less.
When you Download this Book you will Discover
What Ulcerative Colitis Disease is.The current supplementation & herbs available to cure it.Reasons for contracting it and the impact on our bodies.The diet and lifestyle you should be adopting.How to cure your symptoms in just 90 days.
Check out what others are saying
And youll wonder why you didnt try it sooner!
You May Like: Gluten Free Diet For Ulcerative Colitis
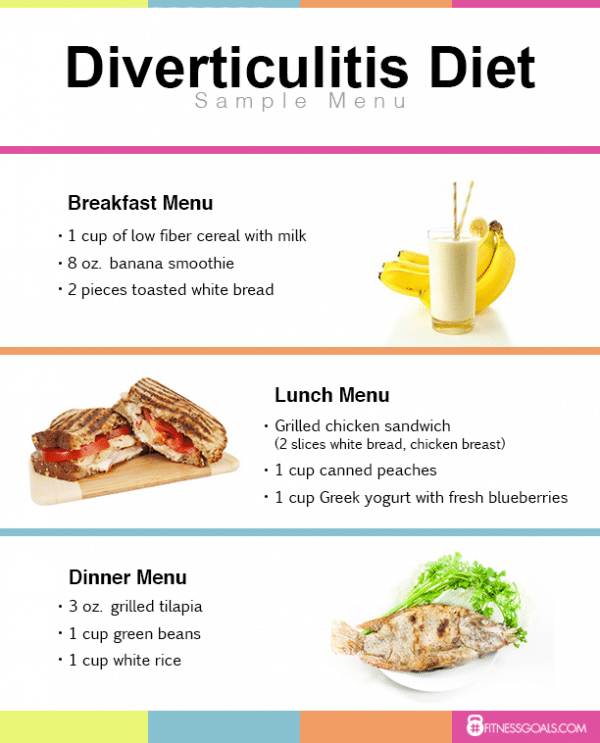
Diet Recommendations For Ulcerative Colitis Flare
- Follow a low residue diet to relieve abdominal pain and diarrhea.
- Avoid foods that may increase stool output such as fresh fruits and vegetables, prunes and caffeinated beverages.
- Try incorporating more omega-3 fatty acids in your diet. These fats may have an anti-inflammatory effect. They are found in fish, including salmon, mackerel, herring and sardines.
- Patients often find that smaller, more frequent meals are better tolerated. This eating pattern can help increase the amount of nutrition you receive in a day.
- Consider taking nutritional supplements if appetite is poor and solid foods are not tolerated well .
Fodmap Diet Plan For Ulcerative Colitis
Fodmap diet plan for ulcerative colitis is made up of a list of foods high in certain carbohydrates called FODMAPs that, when consumed, may cause symptoms to flare. Fodmap diet plan for ulcerative colitis is ensuring patient follow recommended diet that includes foods that are well digested and limited intake of foods that can irritate the stomach.
The fodmap diet is a diet originally designed to treat people with Irritable Bowel Syndrome and other functional gut disorders. The specific foods that can trigger these kinds of problems are known as FODMAPs. FODMAPs stands for Fermentable Oligosaccharides Degrees and Polyols. FODMAPs are sugar alcohols, fibre and non-digestible carbohydrates.
Recommended Reading: How Do You Treat Mouth Ulcers
Nutrition Tips For Inflammatory Bowel Disease
Inflammatory Bowel Disease is a term used for two specific and separate diseases: Crohn’s disease and ulcerative colitis. Nutritional recommendations are different for each disease and for each individual patient. It is important to discuss the treatments that are right for you with a registered dietitian and with your doctor.
Meet Your Uc Surgeons And Team
Most people who have surgery for ulcerative colitis are referred from their gastroenterologist. The surgeon that will complete the surgery is most often a colorectal surgeon, who specializes in surgery of the digestive system.
An enterostomal therapy nurse will be helpful before and after surgery to place an ileostomy. An ET nurse will help decide where the stoma will be placed and will make suggestions on which type of appliance will work best.
Also Check: Do You Still Have Ulcerative Colitis After Colectomy
Should You Start A Low
A diet thats low in certain carbohydrates might help ease the symptoms of inflammatory bowel disease.
Everyday Health
If you have ulcerative colitis , a chronic inflammatory bowel disease that affects the colon, youre probably aware that certain foods can trigger symptoms such as abdominal pain, diarrhea, and more. Thats one reason some people with IBD have tried to adopt a low-FODMAP diet, an eating plan that limits foods that contain FODMAPS, specific types of short-chain carbohydrates.
While low-FODMAP diets have been shown to help ease the symptoms of irritable bowel syndrome , until now researchers werent sure whether these eating plans could alleviate the symptoms of IBD. But a study published in October 2019 in the journal Gastroenterology found that when people with IBD, including UC, stuck to a low-FODMAP diet, they experienced a significant reduction in several gut symptoms after just four weeks.
While adopting the diet had no effect on disease severity, the research adds to the growing evidence that a low-FODMAP diet may help ease GI symptoms and improve a persons overall quality of life.
Thinking of giving a low-FODMAP diet a try? Heres what you should know before you get started.
Ulcerative Colitis Treatment Medications
Treatments for ulcerative colitis includes both medications and surgery however, there is no medication that can cure ulcerative colitis. Medicationsthat treat ulcerative colitis are
- anti-inflammatory agents, for example, 5-ASA compounds like sulfasalazine , and olsalazine , and topical and systemic corticosteroids), and
- immunomodulators, for example, 6-mercaptopurine , azathioprine , methotrexate , cyclosporine .
Treatment of ulcerative colitis with medications is similar, though not always identical, to treatment of Crohn’s disease.
Avoiding foods that trigger ulcerative colitis symptoms is one way to help manage symptoms through diet. Another is knowing what foods to eat that may help relieve flares. Following is a list of foods that may help soothe ulcerative colitis flares:
Dietary choices do not cause ulcerative colitis, but certain foods can trigger and worsen symptoms. Learning to identify trigger foods can help reduce the frequency and severity of ulcerative colitis symptoms.
Not all people with ulcerative colitis have the same triggers, but a list of some of the most common includes:
Read Also: How To Prevent A Pressure Ulcer