How To Know If You Have Crohns Disease Or Colitis And How To Treat Them
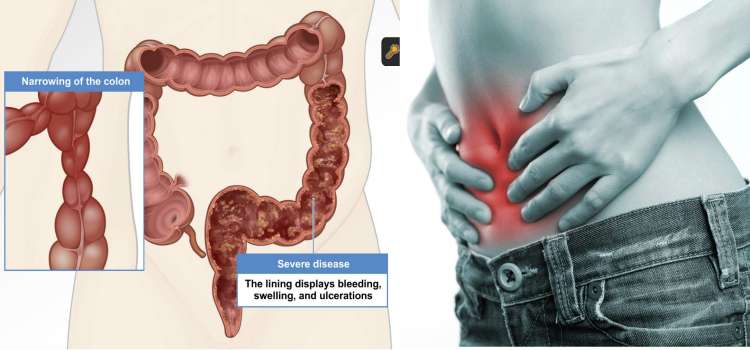
Colitis refers to the inflammation of the inner wall lining of the colon. This may be due to infection, allergies, reduced blood flow to the colon, or conditions such as Crohns disease or ulcerative colitis. The symptoms of colitis depend on the cause but often include a combination of abdominal pain, cramping, and diarrhea.
While some causes of colitissuch as infection, allergies, or microscopic colitiscan be effectively treated, other colitis conditions such as Crohns disease and ulcerative colitis have no known cure. However, these conditions do have treatments that can significantly ease symptoms or even send the disease into extended remission.
Crohns disease is an inflammatory bowel disease caused by inflammation in the digestive tract. It can cause abdominal pain, severe diarrhea, weight loss, malnutrition, and more. While the exact cause of Crohns disease is unknown, doctors suspect that factors such as heredity and immune system may play a significant role while diet and stress likely exacerbate the condition.
Ulcerative Colitis is also an inflammatory bowel disease but is characterized by having ulcers in your digestive tract. This disease causes diarrhea often with blood or pus, abdominal pain and cramping, rectal bleeding, and more. The exact cause of ulcerative colitis is unknown but is thought to have something to do with immune system malfunction
How to Know if You Have Crohns Disease or Coliti
Symptoms of Crohns Disease
- Unexplained weight loss
The Importance Of Colorectal Cancer Screening
Regular screening for colorectal cancer is important for people living with ulcerative colitis because it increases the likelihood of catching cancer in its earliest, most treatable stages.
Screening is done via a colonoscopy, a procedure in which a long, flexible tube with a camera is inserted into the rectum and used to look at the inside of the colon. This allows your doctor to identify and remove any polyps or other tissue that may be precancerous.
Recent technological advances have improved methods for identifying cancer or precancer in the large intestine during a colonoscopy. For instance, a chromoendoscopy may be used to identify polyps and precancerous changes in the large intestine. This involves using a blue contrast dye to highlight any changes to the lining of the intestine.
According to the Crohn’s and Colitis Foundation, those who have had UC symptoms for a period of eight or more years should have a colonoscopy every one to two years. The exception to this is those who have both UC and the liver disease PSC. In this case, surveillance through colonoscopy should begin as soon as a UC diagnosis has been given.
Signs Of Possible Colitis
General signs of colitis can include:
- Intense pain
- Swelling of the colon tissue
- Erythema of the surface of the colon
- Ulcers on the colon which may bleed
- Mucus and/or blood in stool and rectal bleeding
- Diarrhea, which may occur, although some forms of colitis involve constipation so the stool and bowel movements may appear normal.
Other symptoms may include gas, bloating, indigestion, heartburn, gastro esophageal reflux disease, cramps, bowel urgency and many other uncomfortable aches in the gastrointestinal system.
You May Like: Nursing Care Plan For Pressure Ulcer Prevention
What Are The Treatments For Ulcerative Colitis
There is no cure for ulcerative colitis and it is something you will have for the rest of your life, so the aim of treatment is to get your symptoms under control and into remission.
All ulcerative colitis patients are different and a treatment that works for one may not work for another, therefore you may need to go through a period of trial and error to find a medication that works for you. If the first treatment you try doesnt work for you then you may feel frustrated and disheartened and that’s understandable. There are now many different medication options available and more being licensed for ulcerative colitis all the time so there are now more options available to you than ever.
There is a new test available to people newly diagnosed with Crohn’s disease called PredictSURE IBD. This biomarker test can help to predict whether you will have a more ‘mild’ or ‘aggressive’ form of the disease. Your doctor can then use these results to help them choose the most appropriate course of treatment for you, hopefully resulting in a reduction of this period of trial and error before they find a medication that works for you.
Find out more about medications for ulcerative colitis
What Does Constipation In Ulcerative Colitis Feel Like
Constipation, in general, is defined as having fewer than three bowel movements per week. However, the frequency of bowel movements varies from person to person especially in those with gastrointestinal diseases like UC. Constipation usually causes a person to have dry, hard stools that are difficult to pass.
Of the MyCrohnsAndColitisTeam members with UC who report experiencing constipation, many find that this symptom alternates with diarrhea. I have ulcerative colitis, wrote one member, and Im either constipated or the exact opposite. Another member agreed, noting, Ive had UC for 15 years, and I alternate between diarrhea and constipation.
You May Like: Medications Used For Ulcerative Colitis
Figuring Out Which Foods Trigger Flare
As the NIDDK explains, although ulcerative colitis isnt caused by diet or nutrition, certain foods can trigger the symptoms or make them worse in some people. The tricky part is figuring out which ones.
Common ulcerative colitis triggers include dairy, high-fiber foods like fruit, vegetables, and whole grains, spicy foods, alcohol, and caffeine, according to the Mayo Clinic. That said, its really individual. Sam has always loved food and says that when it comes to what she can eat now, I have not figured that aspect out. And its not for lack of trying. I feel like I’ve done everything! she tells SELF, explaining that she tries to avoid various food groups like dairy that can trigger symptoms. It doesn’t mean I don’t ever eat them, but I try to avoid them, she says. I’m definitely still experimenting.
Stacey Bader Curry, 48, was diagnosed with ulcerative colitis in March 2020 and is concerned about giving up foods she loves, as well as alcohol and coffee. I’m trying to focus on what I can eat and not what I can’t eat, she says.
To figure out whether certain foods might be triggering your symptoms, the NIDDK recommends keeping a food diary where you record everything you eat and any flare-ups to help you work out what your dietary triggers could be.
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
- Alcohol.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Salt.
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
You May Like: Bland Diet Recipes For Ulcers
Why Does Ulcerative Colitis Cause Joint Pain
As you can probably guess, the joint pain that occurs as a symptom of some type of Enteropathic Arthritis develops because of the inflammation caused by Ulcerative Colitis.
And no, the cause for this is yet to be found out. In normal circumstances, for some unknown reasons, inflammation occurs and affects some or more than one joint, what is later diagnosed as some type of Arthritis.
So it is not a different story this time it is still the inflammation that has first occurred because of the Ulcerative Colitis that has later only spread and affected some joints in the body, causing the common Arthritis symptoms to develop as well.
But the good news is that there are some promising suggestions for a colectomy to make the Arthritis symptoms, as well as the Ulcerative colitis symptoms, to go away.
Ulcerative Colitis: Diagnosis And Treatment
ROBERT C. LANGAN, MD PATRICIA B. GOTSCH, MD MICHAEL A. KRAFCZYK, MD and DAVID D. SKILLINGE, DO, St. Luke’s Family Medicine Residency, Bethlehem, Pennsylvania
Am Fam Physician. 2007 Nov 1 76:1323-1330.
Patient information: See related handout on ulcerative colitis, written by the authors of this article.
This article exemplifies the AAFP 2007 Annual Clinical Focus on management of chronic illness.
Ulcerative colitis is a chronic disease characterized by diffuse mucosal inflammation of the colon. Ulcerative colitis always involves the rectum , and it may extend proximally in a contiguous pattern to involve the sigmoid colon , the descending colon , or the entire colon .1 This article reviews the diagnosis and treatment of ulcerative colitis from a primary care perspective.
Don’t Miss: Wound Care For Stage 4 Pressure Ulcer
Who Should I Contact If I Am Worried
If you have specific treatment concerns or symptoms you are worried about, you should speak to your GP or get in touch with your IBD nurse or team.
If youve got questions about coronavirus, see nhs.uk/coronavirus or use the online NHS 111 service to check your symptoms 111.nhs.uk/covid-19. Call the NHS 111 service if you cant access the service online, or if you feel you cannot cope with your symptoms at home or your symptoms get worse.
If you are worried about coronavirus and would like more information about things you can try to help your wellbeing during this difficult time, then MIND have lots of resources online.
Please do not go in person to a hospital or your GP unless you have been advised to do so.
Limit Your Fiber Intake
Fiber contributes to bowel regularity and bowel health, but too much fiber can also trigger UC flare-ups.
Try to stick to foods that have no more than 2 grams of fiber per serving. Low fiber foods include:
- refined carbohydrates such as white rice, white pasta, and white bread
- fish
- some cooked fruits
- juice with no pulp
Instead of eating raw vegetables, steam, bake, or roast your vegetables. Cooking vegetables results in some fiber loss.
Recommended Reading: How Long Does A Ulcerative Colitis Flare Up Last
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
The Intensity Of Your Symptoms Might Vary Over Time

The most common ulcerative colitis symptoms are diarrhea containing blood or pus and abdominal pain, the National Institute of Diabetes and Digestive and Kidney Diseases says. Theres a lot of cramping, Cristal Steuer, 38, who was diagnosed with ulcerative colitis while she was in college, tells SELF. You might also experience things like fatigue, fevers, nausea, unintended weight loss, joint pain, and rashes. Whichever symptoms you do have, they may wax and wane, the NIDDK explains. You may have periods when youre in remission interspersed with periods when your symptoms are worse. But some people experience constant symptoms from ulcerative colitis.
Just because you can’t see it doesn’t mean that it’s not hard every single day, Tatiana Skomski, 26, who was diagnosed at 21 after years of unexplained fatigue and pain when an especially bad flare-up nearly caused her to bleed to death, tells SELF.
I’ve had to increase my tolerance for what is a background level of pain, Sam, 22, who was diagnosed with ulcerative colitis in the summer of 2019, tells SELF. I’ll have sharper moments where I can’t functionbut for the most part, it’s more like a constant level of chronic pain.
If pain or other ulcerative colitis symptoms are really interfering with your life, make sure your health care provider knows so that you might be able to tweak your treatment plan if necessary.
Read Also: How To Check A Horse For Ulcers
Ulcerative Colitis Can Take A Toll On Your Mental Health Too
Being told you have a chronic illness can feel like someone has just rerouted the course of your whole life. I went through my own acceptance process, Skomski says. I definitely went through a period of questioning if my life would ever be normal. With time, processing the reality of having ulcerative colitis became easier. I had to learn there’s nothing wrong with me it’s just part of who I am, Skomski says. You have to do a lot of mental work to flip the way you perceive it because otherwise it can really eat away at you.
Dealing with the symptoms can also be mentally and emotionally taxing. The psychological side of the pain is a lot worse than the actual physical sensation, Sam says. It’s when you feel like it’s never going to end, or you’re going to be stuck in that high level of pain for a long period of time, or that no one gets how hard it is to deal with it. This has led to constant vigilance about her health. It’s very hard for me to not be closely monitoring my body 24/7, Sam says. The catch-22 is that stress is definitely a trigger for me.
Medications For Other Conditions
A medication you take for another condition can also trigger a flare-up.
This might happen if you take an antibiotic to treat a bacterial infection. Antibiotics can sometimes disrupt the balance of intestinal bacteria in the gut and cause diarrhea.
Certain over-the-counter nonsteroidal anti-inflammatory drugs , such as aspirin and ibuprofen , may also irritate the colon and cause a flare-up.
This doesnt mean you should stop taking antibiotics or pain medications, but you should speak with your doctor before taking these drugs.
If you take an antibiotic, you may also need a temporary antidiarrheal medication to combat possible side effects.
If you experience stomach pain after taking an NSAID, your doctor may suggest acetaminophen to reduce pain instead.
You May Like: How Serious Is A Stomach Ulcer
Fatigue From Ulcerative Colitis Can Be Brutal
Exhaustion from ulcerative colitis can be so severe its hard to get through day-to-day life. For Sam, fatigue was one of the first signs that something was wrong. I’m usually a pretty energetic person, she says. I like running every day, things like that. And I just couldn’t do it anymore.
After developing ulcerative colitis, you might have to be more careful than youre used to about how you use your energy. Some days I’m just hit with a truck of fatigue, Skomski says. So I always give myself an out. If I have plans with friends or we’re going out of town, Ill tell the other people, I might not feel good and we might have to reschedule.
Sam has had to have similarly frank conversations about the fact that her energy can take a major dip sometimes. I’ve had to teach everyone around me that it doesn’t mean I’m mad at them, it doesn’t mean I’m not happy, she says. It’s just that I have a very concrete amount of energy that day.
Ulcerative Colitis Questions To Ask Your Doctor
Whether youâre worried your symptoms are UC, or you already have the condition and want more information, here are questions to ask your doctor:
- Are my symptoms a sign of ulcerative colitis or another condition?
- Are there different kinds of UC? Do they have different symptoms?
- What tests will I need?
- If I have ulcerative colitis, what will my treatment plan be?
- Will changing my diet or lifestyle help ease my symptoms?
- How serious is my ulcerative colitis?
- If I take medication for ulcerative colitis, will there be side effects?
- Should I take nutritional supplements like probiotics?
- How often will I need to come in for checkups?
- What should I do if my symptoms suddenly get worse?
- How do I know if my ulcerative colitis is getting worse?
- How do I know if I should change my ulcerative colitis medication?
- Should I consider surgery? What does surgery involve?
- What is my risk of getting colon cancer?
Don’t Miss: What’s The Signs Of An Ulcer