Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
What Makes Cura Different From Other Forms Of Curcumin
Most curcumin products on the market are boosted in bioavailability. This is generally a benefit, but not when treating gut inflammation and digestive disorders. Thats why we specifically use a non-absorbable formulation that ensures increased concentration in the intestines. We call this formula gut-directed curcumin.
Give Yourself Some Tlc
Stress doesn’t cause UC, but it makes symptoms and flares worse for some people. If it affects you, try meditation, breathing exercises, or a massage. You could also see a pro to try biofeedback, hypnotherapy, or a type of counseling called cognitive behavioral therapy, which helps you learn new ways to handle problems. Being active helps, too. Try yoga, tai chi, or other low-impact exercises like walking.
10
You May Like: How To Remove Ulcers In Stomach
Foods To Avoid During Flares
Diet doesnt cause flares, but your food choices can make symptoms worse if your IBD becomes active.
How foods affect people who are flaring varies from person to person. But here are some of the foods that may worsen symptoms of a flare and cause complications:
- Beverages containing alcohol or caffeine.
- Sugar alcohols used to sweeten in sugar-free foods
- Raw fruits and vegetables
- Whole grain and high-fiber breads and cereals
- Fruits with seeds and skins
Find A Healthcare Provider
To learn more, find a rheumatology healthcare provider and ask them if XELJANZ could be an option to treat your moderate to severe RA when TNF blockers have been used and did not work well. Enter your information below to browse a directory of local physicians and specialists.
By clicking âSearch,â you acknowledge and agree with the Terms and Conditions.
Please note: While the directory is updated regularly, the search results may not include current physician information or a comprehensive list of all physicians who treat rheumatoid arthritis. Please see Terms and Conditions for more details.
Read Also: What Are The Side Effects Of An Ulcer
To Ease Abdominal Pain
As your doctor treats the flare, your abdominal pain should get better. Remember to avoid nonsteroidal anti-inflammatory drugs , but Damas also recommends avoiding opioid analgesics . Your doctor may prescribe an antispasmodic medication, which relaxes the gut muscles.
Warning signs of a flare: People with ulcerative colitis often experience abdominal pain, but if the pain is worse or markedly different from your baseline, Damas recommends calling your doctor. Red flags that require medical attention include fever, fatigue, and intense abdominal pain.
Why Do I Need To Take The Assessment
The reason many supplements fail is a lack of vital information, both on the side of patients and the side of providers. Supplement providers require the history, specifics, and state of your condition in order to recommend the most efficient recovery strategy. This data helps us provide the correct product, dosage & combinations for you.
Read Also: What Is A Bland Diet For Ulcers
Approved By Leading Gastroenterologists
My experience with this combination is very good. Weve had some patients who were able to avoid advancing them to biologics, and others we could give this combination to instead of steroids.
– Dr. Dror Shoval MD, Senior Pediatric Gastroenterlogist
I admit I was skeptical about these treatments. But with time I realized patients were reporting a significant benefit and I was surprised to see that they were improving not just subjectively but objectively.
– Henit Yanai MD, Senior Gastroenterlogist
Inflammatory Bowel Disease And The Balanced Dinner Plate
All together, a familiar message is beginning to come through: a balanced diet that is rich in fruits, nuts, and vegetables, and not heavily based on certain types of meat might decrease an individuals risk for developing IBD and might also help those who already have it to limit the occurrence of disease flares.
Inflammatory bowel disease is a collective term for a number of intestinal conditions, primarily Crohns disease and ulcerative colitis. In the search for a fuller understanding of IBD, numerous recent studies have looked at the effects of specific foods on the development of the disease and management of its associated flares.1 Along the way, researchers have found that while some foods do appear to be associated with an increased risk of IBD and flares, others may actually have a protective effect.
Read Also: Total Contact Casting For Diabetic Foot Ulcers
Recommended Reading: Are Probiotics Good For Stomach Ulcers
Identify Daily Stressors And Put Your Health First
The second tip to help you prevent an ulcerative colitis flare-up is to ensure that you learn how to identify daily stressors so that you may eliminate them. Stressors for many people come up on a daily basis, whether it be work based, family based, or even relationship/friends based. I think that always keeping in mind that your health comes first no matter what. In other words, no issue is as important as your own health. By always keeping this in mind I find that it helps me mentally to filter things that brings stress instead of peace.
You May Like: Can Ulcerative Colitis Cause Body Aches
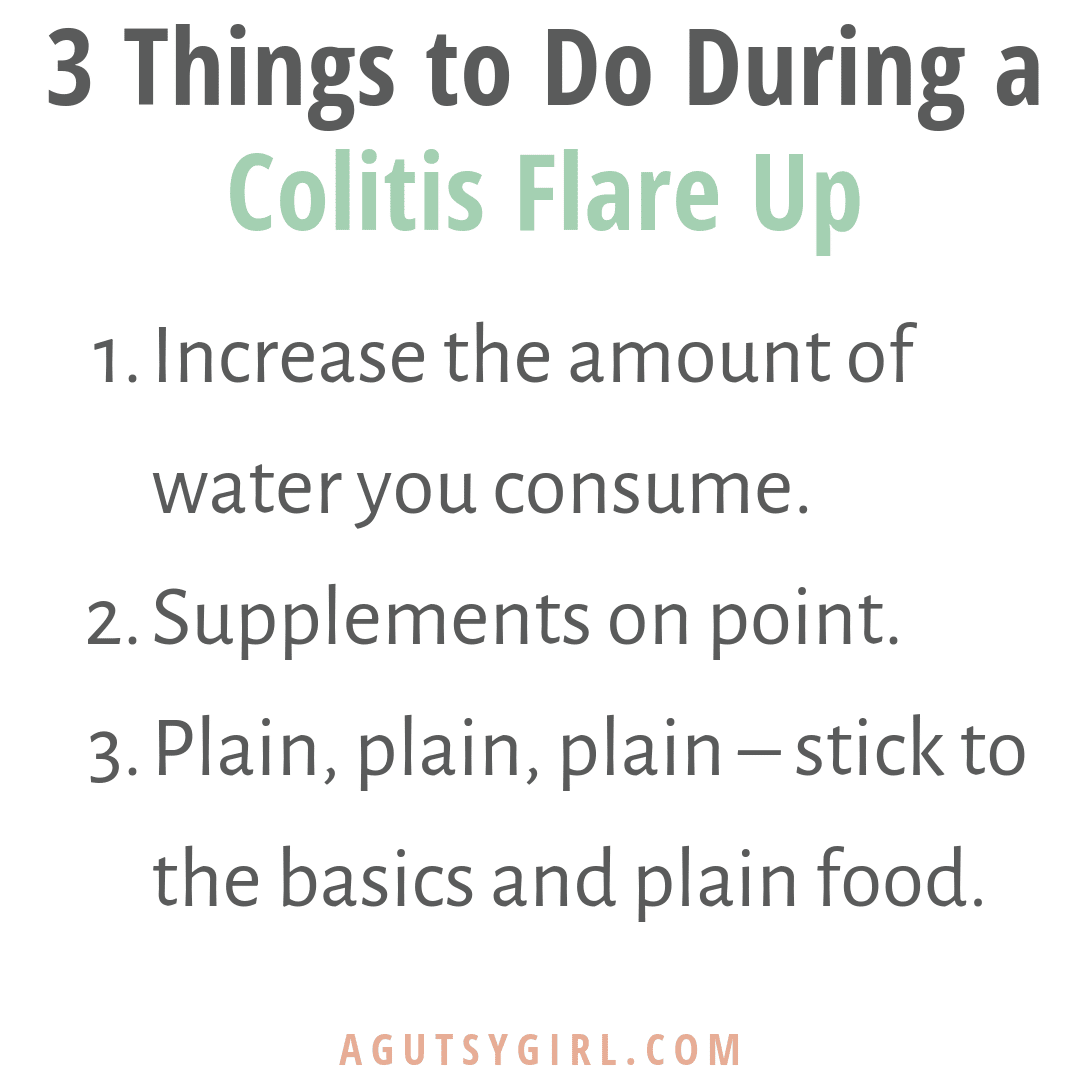
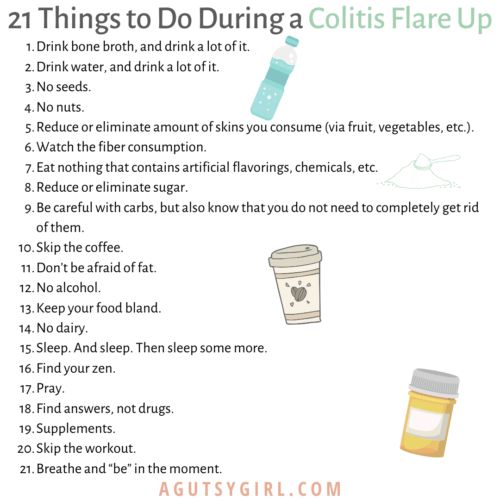
What To Do During An Ulcerative Colitis Flare To Minimize Symptoms
Youll inevitably experience another UC flare-up at some point, despite your best prevention efforts. When this happens, there are a few ways youll need to tweak your normal routine to minimize the severity of your symptoms and get back into remission ASAP. Even some of your typically healthy habits like loading up on veggies may be a no-go. Here are a few natural remedies that may help:
Read Also: How To Treat Skin Ulcers
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
What Should I Eat During An Ulcerative Colitis Flare
There is no specific type of diet that has been proven to relieve symptoms in people with ulcerative colitis. However, you may find that particular foods make symptoms worse.
It is important to identify and limit any foods that lead to worsening of your symptoms. Keeping a food journal may help you track how your diet relates to your symptoms.
Some suggestions that may help during a flare-up include:
- Reduce dairy products containing lactose
- Avoid high-fat foods
- What remedies help during an ulcerative colitis flare-up?
In addition to taking medication as prescribed and eating a well balanced diet, maintaining a healthy lifestyle can be beneficial for managing ulcerative colitis. Regular exercise and mindfulness strategies have been shown to improve overall health and quality of life.
Arastéh, K., Baenkler, H. W., Bieber, C., Brandt, R., & Chatterjee, T. T. . Duale Reihe Innere Medizin. Georg Thieme Verlag.
Dignass, A., PreiÃ, J. C., Aust, D. E., Autschbach, F., Ballauff, A., Barretton, G., â¦& Jantschek, G. . Aktualisierte Leitlinie zur Diagnostik und Therapie der Colitis ulcerosa 2011Ergebnisse einer Evidenzbasierten Konsensuskonferenz. Zeitschrift für Gastroenterologie, 49, 1276-1341.
Elizabeth Oliver, PhD
Read Also: Foods To Stay Away From With Ulcerative Colitis
What To Eat During A Ulcerative Colitis Flare
Research shows that nutrition cant cause or cure ulcerative colitis. There are no foods that can cause someone to develop ulcerative colitis, and there is no miracle diet that will cure people of the condition. However, good nutrition does play an important role in the management of ulcerative colitis symptoms, especially during a flare.
Ulcerative colitis flare-ups are uncomfortable and frustrating. Pain, bloating, cramping, fatigue, rectal bleeding, and diarrhea are common symptoms during flare-ups. If youre in the midst of the flare, changes in your diet can help control your symptoms and allow your intestine time to heal. If you have a flare
While carefully watching what you eat can help ease symptoms of ulcerative colitis, there are very few treatments for ulcerative colitis currently available. Participating in research is one of the best ways to actively search for a cure. Research helps increase the understanding of ulcerative colitis and trial new treatment options.
If you or a loved one has ulcerative colitis, fill out the form below to learn more about a clinical trial that you may qualify for.
How Do I Know If My Uc Has Gone Into Remission
UC doesn’t have a cure. Instead, the goal of any treatment plan is to send the disease into remission.
When UC is in remission, you don’t experience as many symptoms and start to feel better. If your UC medications and lifestyle changes work well for you, remission may last for months or even years. There are several different kinds of remission:
- Clinical remission: When a patient isn’t experiencing symptoms and may feel better.
- Endoscopic remission: Testing of the intestinal lining shows no inflammation
- Biochemical remission: Blood and stool tests show no sign of inflammation
- Surgical remission: When UC goes into remission after surgery to treat it
- Histologic remission: When both clinical and endoscopic tests didn’t show signs of UC
With UC, it can feel like life revolves around symptoms. If UC symptoms keep coming back, it can be a sign that medications aren’t working. Consider taking part in a clinical trial researching an investigational treatment option for people living with UC.
Don’t Miss: Horse Feed For Gastric Ulcers
What Do You Mean By A Tailored Plan
Its our duty to ensure you receive the most precise strategy for your age, sex, and state of condition. Thats why we tailor each treatment plan to the individual through our online assessment, which is based on official disease indexes. This information helps us provide the most accurate and evidence-based plan for each individual.
Skipping Or Forgetting To Take Your Uc Medication
UC causes inflammation and ulcers in the colon. If left untreated, this condition can lead to life threatening complications, such as:
- bowel perforation
- colorectal cancer
- toxic megacolon
A doctor will likely prescribe medication, such as an anti-inflammatory or immunosuppressant drug, to help reduce inflammation.
These medications can help ease symptoms of UC and also function as maintenance therapy to keep you in remission. Symptoms could return if you do not take your medication as directed.
At some point, the doctor may discuss slowly tapering off the medication. However, you should never decrease your dosage or stop taking your medication without speaking with your prescribing doctor first.
Read Also: Do Ulcers Make You Bloated
What Are Some Practical Steps To Take When A Flare
The first thing to do if a flare up occurs is to make sure you are eating a healthy diet which is low in fibre and contains plenty of water. Avoiding dairy products and cutting down carbohydrates may also help. The vast majority of people will requite adjustments to their medication, so you should seek medical advice from your GP or specialist.
Continue To Eat And Drink
If your symptoms are severe, you may not feel like eating or drinking. However, this increases the risk of becoming dehydrated. Instead, try to follow a healthy diet, but avoid high-fiber foods for a few weeks. These include bread and cereal made with whole grains, fresh and dried fruit, raw vegetables, seeds and nuts. Eating smaller meals may also help. Also avoid drinking carbonated drinks, which can worsen your symptoms. Instead, drink small amounts of water throughout the day to stay hydrated.
Also Check: Diet For Gerd And Ulcers
How To Calm An Ulcerative Colitis Flare
This article was co-authored by Peter Gardner, MD. Peter W. Gardner, MD is a board certified physician who has practiced Gastroenterology and Hepatology for over 30 years. He specializes in diseases of the digestive system and liver. Dr. Gardner earned his Bachelors degree from the University of North Carolina and attended Georgetown Medical School. He completed his residency in Internal Medicine and then his fellowship in Gastroenterology at the University of Connecticut. He is a previous Chief of Gastroenterology at Stamford Hospital and remains on the staff. He is also on the staff of Greenwich Hospital and New York Presbyterian Hospital. Dr. Gardner is an Approved Consultant in Internal Medicine and Gastroenterology with the American Board of Internal Medicine.There are 8 references cited in this article, which can be found at the bottom of the page.wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 100% of readers who voted found the article helpful, earning it our reader-approved status. This article has been viewed 14,663 times.
Get Your Free Protocol Today
Heres what they havent told you.
You dont have to suffer symptoms forever. Not with the right treatment.
We spent 10 years developing a natural therapy to alleviate chronic inflammation in Crohns & Colitis for good. The result was the CurQD® Protocol, a supplement regimen highly effective in inducing remission in difficult-to-treat cases.
While testing CurQD® in our clinical trials, we found that tailoring the formula to the patient significantly improved symptom relief and remission rates. So we created customized formulas to target each stage of disease severity.
Whether youre suffering severe symptoms or seeking a natural approach to prevent relapse, we have a protocol for you.
After one month I felt better.
Also Check: Ulcerative Colitis And Blood In Urine
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
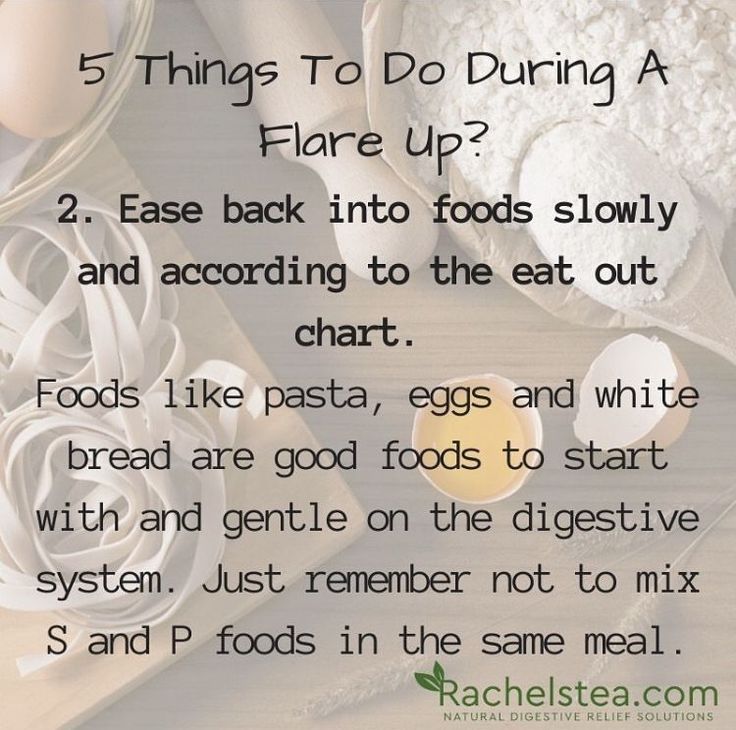
Eat What Works For You
Avoiding dairy products and fiber during a flare just might bring relief, Dr. Bedford says. In addition, a low-residue diet can sometimes assist. This means eating more refined grain products like white breads, cereals, and some pastas mashed potatoes and apple sauce while avoiding foods like whole grain breads, whole grain cereals, and whole grain pastas. It also means no fresh fruits or vegetables , Dr. Boxer points out. I always tell patients, if you would normally see a portion of this food in your stool, stay away from it during a flare.
Also Check: Can Vyvanse Cause Stomach Ulcers
Should I Change My Diet During A Flare
During a period of active inflammation, any food can make pain, bloating, cramping, and diarrhea worse. However, you still need to eat during a flare. You also need to drink plenty of fluids with salt and water so that you absorb and retain fluid. Many people switch to a bland diet or to an all-liquid diet during a flare. Bland foods like rice, toast, bananas, applesauce, and nutritional drinks like Carnation® Instant Breakfast, Boost® or Ensure® can help.
A low-residue diet limits the amount of fiber and other material that cannot be digested as it passes through your small intestine. A low-residue diet reduces the size and number of your stools and helps relieve abdominal pain and diarrhea.
What Are Ulcerative Colitis Flare
Ulcerative colitis is a condition which affects thousands of people across the UK. Luckily, many people with ulcerative colitis flare-ups receive advice and treatment, meaning the condition has minimal impact on their quality of life.
This doesnt mean flare-ups are completely avoidable though. Depending on whether you have proctitis, distal or total colitis, a flare-up may have different effects on the individual. Knowing how to recognise and manage these effects is very important.
In this short blog post, we will discuss what happens during a flare-up and how best to alleviate problems when it does.
Read Also: What Are The Symptoms Of Ulcerative Colitis