What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
Diet Management In Ulcerative Colitis
Its important to pay attention to what you eat if you have ulcerative colitis . Foods do not drive the condition, although they can induce flare-ups.
How can you avoid those triggers while still getting the nutrition you require? A nutrition plan can be beneficial in this situation. Here we discuss diet in Ulcerative Colitis, including what foods to eat and what foods to avoid.
How To Calm An Ulcerative Colitis Flare
This article was co-authored by Peter Gardner, MD. Peter W. Gardner, MD is a board certified physician who has practiced Gastroenterology and Hepatology for over 30 years. He specializes in diseases of the digestive system and liver. Dr. Gardner earned his Bachelors degree from the University of North Carolina and attended Georgetown Medical School. He completed his residency in Internal Medicine and then his fellowship in Gastroenterology at the University of Connecticut. He is a previous Chief of Gastroenterology at Stamford Hospital and remains on the staff. He is also on the staff of Greenwich Hospital and New York Presbyterian Hospital. Dr. Gardner is an Approved Consultant in Internal Medicine and Gastroenterology with the American Board of Internal Medicine.There are 8 references cited in this article, which can be found at the bottom of the page.wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 100% of readers who voted found the article helpful, earning it our reader-approved status. This article has been viewed 9,951 times.
Also Check: What Is Refractory Ulcerative Colitis
What Other Conditions Can Cause Urgency And Incontinence
Accidental bowel leakage can happen because of weakness to the anal sphincter or damage to the muscles in the pelvic floor. This can result from trauma during childbirth or surgery, among other causes. Problems with feeling the sensation of rectal fullness causes some cases of incontinence. Bowel disturbances can cause accidental bowel leakage. One example is when chronic constipation leads to overflow diarrhea.
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
Also Check: Can You Eat Oatmeal With Ulcerative Colitis
Medications For Other Conditions
A medication you take for another condition can also trigger a flare-up.
This might happen if you take an antibiotic to treat a bacterial infection. Antibiotics can sometimes disrupt the balance of intestinal bacteria in the gut and cause diarrhea.
Certain over-the-counter nonsteroidal anti-inflammatory drugs , such as aspirin and ibuprofen , may also irritate the colon and cause a flare-up.
This doesnt mean you should stop taking antibiotics or pain medications, but you should speak with your doctor before taking these drugs.
If you take an antibiotic, you may also need a temporary antidiarrheal medication to combat possible side effects.
If you experience stomach pain after taking an NSAID, your doctor may suggest acetaminophen to reduce pain instead.
Natural Remedies For Ulcerative Colitis
11 min. read
Dr. David Williams
Ulcerative colitis is a serious inflammation of the lower bowel. This inflammatory bowel disease seems to be hereditary and usually begins between the ages of 15 and 40. Ulcerative colitis is rare in most populations that havent adopted the typical Western diet that is high in refined carbohydrates and fats and low in fiber. And in some cases, ulcerative colitis has been linked to allergic reactions to certain foods. Corn, wheat, and milk products seem to be the most common culprits.
With ulcerative colitis, the inflammation of the lower bowel surface often results in ulcerations that lead to profuse bleeding, along with other symptoms including severe, chronic diarrhea and bloody, mucus-laden stools. If the condition persists, the individual will suffer from fat, protein, vitamin, and mineral deficiencies. If ulcerative colitis continues for 10 years or more, studies have shown the risk of developing colon cancer is almost 200 times greater than that of the general population.
Most doctors in this country rely on powerful drugs to treat ulcerative colitis, even though their side effects can be substantial and their success rate is relatively low.
My plan below, however, consists of proven all-natural therapies, along with a few additional alternative remedies to try for especially stubborn cases. Of course, because ulcerative colitis can turn severe in some instances, it should always be monitored by a doctor.
Read Also: Carbohydrate Diet For Ulcerative Colitis
Pineapple Juice For Ulcerative Colitis Relief
One of the main protagonists of these home remedies to control ulcerative colitis is pineapple juice. The bromelain in pineapples is great to treat digestive diseases, since it has anti-inflammatory properties. In fact, by drinking two classes of pineapple juice every day , youll feel relief from your symptoms.
Where Does Ulcerative Colitis Pain Come From
Ulcerative colitis can be an unpredictable condition as the cause of it has yet to be uncovered. The illness is also associated with flare-ups, which can have unique triggers. Approximately 30% of people who are currently in remission will relapse in the next year.
It is believed that there is a genetic component that comes into play with this condition. Those with family members with ulcerative colitis are more likely to be afflicted by this condition. This disease can generally be found in any age group, but it is far more prevalent between the ages of 15 to 30, as well as 50 to 70. It is also believed that Caucasians are much more likely to develop this condition and the risk is even higher for those of Ashkenazi Jewish decent.
At one time, it was believed that ulcerative colitis was caused by stress and diet. Today, researchers believe these can be a trigger, but they no longer think it is a direct cause. Most studies are focused on searching the immune systems for a root cause for this condition. It is thought that the immune system might inadvertently attack the healthy cells in the GI tract when trying to fight off foreign invaders, which causes inflammation.
You May Like: What Are Diabetic Leg Ulcers
Cut Out Raw Veggies And Other Gut Irritants
In the midst of a ulcerative colitis flare, you want to be as gentle on your digestive system and colon as possible. Give your gut a little vacation, says Cohen. This ideally means eliminating or scaling back on: raw vegetables, raw and cooked fruits, high-fat foods , high fiber foods , spicy foods, alcohol, and caffeinated beverages. Basically, any food that takes significant digestive effort or stimulates the bowels.
Natural Intestinal Healing Remedies
Due to the common complaints associated with medications and surgery, research has uncovered many natural options for healing a damaged digestive system. From lifestyle changes, dietary adjustments, and stress reduction techniques, ulcerative colitis can not only be prevented, but it can also be successfully healed.
One additional benefit is that many people, especially the elderly, cannot tolerate many medications. Natural options allow for healing without additional pain. These include:
Regular Exercise: Exercise is beneficial to your overall health, but when it comes to ulcerative colitis, regular activity can help with many of the complications associated with the condition. Studies have shown that individuals with ulcerative colitis also suffer from decreased bone density, emotional health problems, weight gain, and suppressed immune system.
| Related: Why a Workout Plan Improves the Benefits of Probiotics |
Exercise can help boost moods, promote weight loss, boost energy levels, and support bone health. In addition to this moderate exercise triggers the release of specific chemicals called myokines that promote healing from inflammatory-related damage.
Yoga is a specific exercise that takes care of the digestive system and provides relief for many ulcerative colitis symptoms.
Stress Reduction: Stress and anxiety are intricately linked to inflammation. The release of inflammatory chemicals is a direct result of the body experiencing stress.
Recommended Reading: What Foods Should Be Avoided With Stomach Ulcers
Be Diligent And Careful With Medication
A physician will usually prescribe an anti-inflammatory and medication to help with an overactive immune system with a diagnosis of ulcerative colitis. This medication is vital to fight off flare-ups and missing a dose can be a trigger all by itself.
When taking medication for this condition, it is always wise to consult a doctor. Certain over-the-counter medications, like NSAIDs, can exacerbate ulcerative colitis as well as cause other issues.
Ways To Manage Ulcerative Colitis

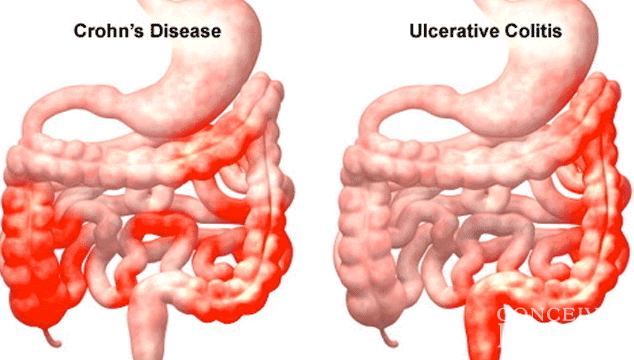
About 1.3% of American adults suffer from inflammatory bowel disease , a chronic disease including Crohns disease and ulcerative colitis . One of the significant differences between these two types of IBD is where they occur: Crohns can affect any part of the digestive tract, while ulcerative colitis affects the large intestine and rectum.
Ulcerative colitis takes a physical and emotional toll on the men and women who suffer from it. The team at Desert West Surgery has extensive experience helping patients manage their UC symptoms, so they can focus on enjoying their lives again. Here are five things you can do to manage your UC symptoms.
Also Check: Best Meds For Ulcerative Colitis
Speak With Your Doctor
Without treatment, people with UC tend to relapse.
For many people with mild or moderate symptoms, things improve somewhat after diagnosis. This is thanks to medication, along with identifying and avoiding triggers.
More aggressive cases are less common, and only a small number of severe cases will require hospitalization.
Repeated flare-ups can indicate problems with your current treatment, so speak with your doctor and discuss adjusting your medication.
Several classes of medication now exist that can help you get into and stay in remission. Your doctor may need to add another type or increase your dosage.
The only way to prevent UC flare-ups is to have surgery. The most common type of UC surgery is the proctocolectomy, which involves the removal of the rectum and colon.
Candidates for UC surgery include people who:
- have sudden or severe disease
- have a perforated colon
- are at risk for colorectal cancer
- are unable to tolerate their UC medications due to side effects
- have stopped responding to their UC medications
In addition to knowing how to manage flare-ups, its also helpful to recognize factors that can trigger your flare-ups.
Ulcerative Colitis Treatment Medications
Treatments for ulcerative colitis includes both medications and surgery however, there is no medication that can cure ulcerative colitis. Medicationsthat treat ulcerative colitis are
- anti-inflammatory agents, for example, 5-ASA compounds like sulfasalazine , and olsalazine , and topical and systemic corticosteroids), and
- immunomodulators, for example, 6-mercaptopurine , azathioprine , methotrexate , cyclosporine .
Treatment of ulcerative colitis with medications is similar, though not always identical, to treatment of Crohns disease.
Don’t Miss: What Can I Take For A Stomach Ulcer
Can Surgery Affect Nutritional Status
Some patients need surgery for severe inflammation, strictures, fistulas and abscesses. In Crohn’s disease, the affected portion of the digestive tract is removed. In ulcerative colitis, the colon is often removed and the ileum may be attached to the anus.
Removal of portions of the intestine can affect nutritional status. When sections of the small or large intestine are removed, surface area for absorption of nutrients is decreased. The following diagram illustrates where nutrients are absorbed. If certain portions of the intestine are severely inflamed, or have been removed, absorption of nutrients may be affected. Malnutrition and nutrient deficiencies can result.
If you have had or are planning to have surgery to remove intestines, talk to your doctor or registered dietitian about which vitamins and minerals you need to take.
Diet And Lifestyle Changes
Although diet and stress do not cause ulcerative colitis, there may be times when changes in your lifestyle may help control your symptoms and lengthen the time between flare-ups. The following changes may help to ease your symptoms:
- Limit milk/dairy products. If you are lactose intolerant , milk and dairy products can produce symptoms of excess gas and diarrhea.
- Restrict intake of certain high-fibre foods: such as nuts, seeds, and raw vegetables.
- Limit intake of caffeine, alcohol, carbonated drinks and fatty foods. .
- Eat small, frequent meals, rather than large meals..
- Exercise regularly to promote movement of the colon and reduce stress..
- Minimize stress. Yoga, meditation and slow, relaxed breathing techniques can help people with ulcerative colitis manage stress..
Ask your doctor or pharmacist if one of these formulations may be right for you. It is important to take the probiotic in the dose and duration recommended by the manufacturer to achieve the best results.
Also Check: Remicade Vs Humira Ulcerative Colitis
Diet Progression Following Flares For Ulcerative Colitis And Crohn’s Disease
- Continue to follow a low residue diet and slowly add back a variety of foods.
- Begin with well-tolerated liquids and advance to soft solids, then solids .
- Introduce one or two items every few days and avoid any foods that cause symptoms.
- Add fiber to diet as tolerated. Well-tolerated fiber sources include tender cooked vegetables, canned or cooked fruits, and starches like cooked cereals and whole wheat noodles and tortillas.
- Between flares, eat a wide variety of foods as tolerated. This includes fruits, vegetables, whole grains, lean protein, and low-fat and nonfat dairy products.
- Increase your calorie and protein intake following a flare. Abdominal pain, diarrhea and decreased appetite may have caused poor food intake. Steroids used to treat flares also can increase protein needs.
Suggestions for first foods after a flare include:
- Diluted juices
Dietary And Lifestyle Modifications
As most nutrients are absorbed higher up in the digestive tract, those with ulcerative colitis generally do not have nutrient deficiencies however, other factors might influence your nutritional state. Disease symptoms may cause food avoidance, leading to food choices that might not provide a balanced diet. If bleeding is excessive, problems such as anemia may occur, and modifications to the diet will be necessary to compensate for this.
Generally, better overall nutrition provides the body with the means to heal itself, but research and clinical experience show that diet changes alone cannot manage this disease. Depending on the extent and location of inflammation, you may have to follow a special diet, including supplementation. It is important to follow Canadas Food Guide, but this is not always easy for individuals with ulcerative colitis. We encourage you to consult a registered dietitian, who can help set up an effective, personalized nutrition plan by addressing disease-specific deficiencies and your sensitive digestive tract. Some foods may irritate the bowel and increase symptoms even though they do not worsen the disease.
In more severe cases, it might be necessary to allow the bowel time to rest and heal. Specialized diets, easy to digest meal substitutes , and fasting with intravenous feeding can achieve incremental degrees of bowel rest.
Read Also: Cure For Peptic Ulcer By Diet
Find Ways To Chill Out
All of the stress-busting suggestions above are extra important when youre in the midst of a flare-up. Cohen also recommends implementing deep breathing exercises before every meal, as this relaxes your body and mind allows you to digest more optimally. And, since youll be eating 4-6 smaller meals, this is a great way to get a dose of calm at multiple points in the day.
Tips For Managing Ulcerative Colitis Symptoms

- Consult your healthcare provider or dietitian before making any changes to your diet
- Eat a well-balanced nutrient rich diet
- Eat more frequently. Eat five to six smaller meals over the course of a day
- Stay hydrated by drinking water and fluids with salt like broth, tomato juice or rehydration solutions
- Drink slowly and avoid using a straw because these may cause gas due to taking in air
- Use a food diary to record the foods you eat and how these impact your symptoms
- Avoid your specific trigger foods
- Use simple cooking methods boil, steam, grill, poach, broil or saute
Also Check: Vegetarian Diet For Ulcerative Colitis
How Food Affects Uc
Diet is really important, says Dr. Poppers. Red meat and alcoholic beverages are two variables associated with an increased likelihood of relapse for UC patients, according to a study in Nutrition and Metabolic Insights. While there is no specific UC diet, you can track symptoms in a diary to determine your own food triggers. Dr. Poppers also recommends seeing a nutritionist who can help you learn more about better-tolerated versus less-tolerated IBD foods.
How Is Fecal Incontinence Evaluated
Less than one-third of people with accidental bowel leakage tell their health care provider.2 The people who do talk to their provider about it tend to have more frequent and severe symptoms, diarrhea, or pain. It can be easier to talk about accidental bowel leakage with a provider that you see regularly.
Your provider may bring it up by asking you about feelings of urgency or rectal fullness.1 It may come up as part of a discussion of your medical or surgical history. Your provider may do a rectal examination to determine the reason for incontinence.
Don’t Miss: How To Cure Ulcerative Proctitis