How Do Doctors Diagnose Ulcerative Colitis
To diagnose ulcerative colitis, doctors review medical and family history, perform a physical exam, and order medical tests. Doctors order tests to
- confirm the diagnosis of ulcerative colitis
- find out how severe ulcerative colitis is and how much of the large intestine is affected
- rule out other health problemssuch as infections, irritable bowel syndrome, or Crohn’s diseasethat may cause symptoms similar to those of ulcerative colitis
What Ulcerative Colitis Treatments Should You Consider After A Diagnosis
We could write a whole article on treatments for ulcerative colitis , but know this: The majority of patients can get control of their disease with medical therapy, Dr. East says. About 15 out of 100 patients may need surgery by 10 years after diagnosis, but this varies by extent of inflammation. New drugs are making the need for surgery less common.
Biologics, which are powerful medications made from living things that are delivered via injection, are very effective at controlling the inflammation associated with ulcerative colitis, and are based on your own antibodies, Dr. East explains. They have the ability to bind to specific molecules involved in triggering inflammation, and have revolutionized treatment of UC and other autoimmune disorders, he says.
Dr. East says lots of patients see a change for the better in two to four weeks. In some cases, a fast-acting drugsteroids, for examplemay be used to get control quickly and then a slow-acting maintenance therapy takes over. Maintenance medications are considered safer than steroids for longer term use.
For some people, the internal J-pouch just wont work. Surgeons create an opening called a stoma in the abdomen, and an external pouch does the waste collection.
Ct Scans And Ct Enterography
CT scans involve taking a series of X-rays to create detailed two- and three-dimensional images of the body. CT scans of the gastrointestinal tract can reveal a narrowing of the small or large intestine, called a stricture, or an obstruction. The test may also indicate inflammation in the small intestine, which suggests that Crohns disease may be causing your symptoms.
Occasionally, doctors may recommend an enhanced CT scan, known as a CT enterography. Prior to the scan, you drink a contrast agent. As the liquid passes through the digestive tract, the CT scanner takes pictures of the small intestine and may reveal anatomical problems. For example, if an obstruction is present, the contrast liquid is visibly blocked.
Also Check: Peptic Ulcer Food To Eat
Tests To Diagnosis Of Ulcerative Colitis
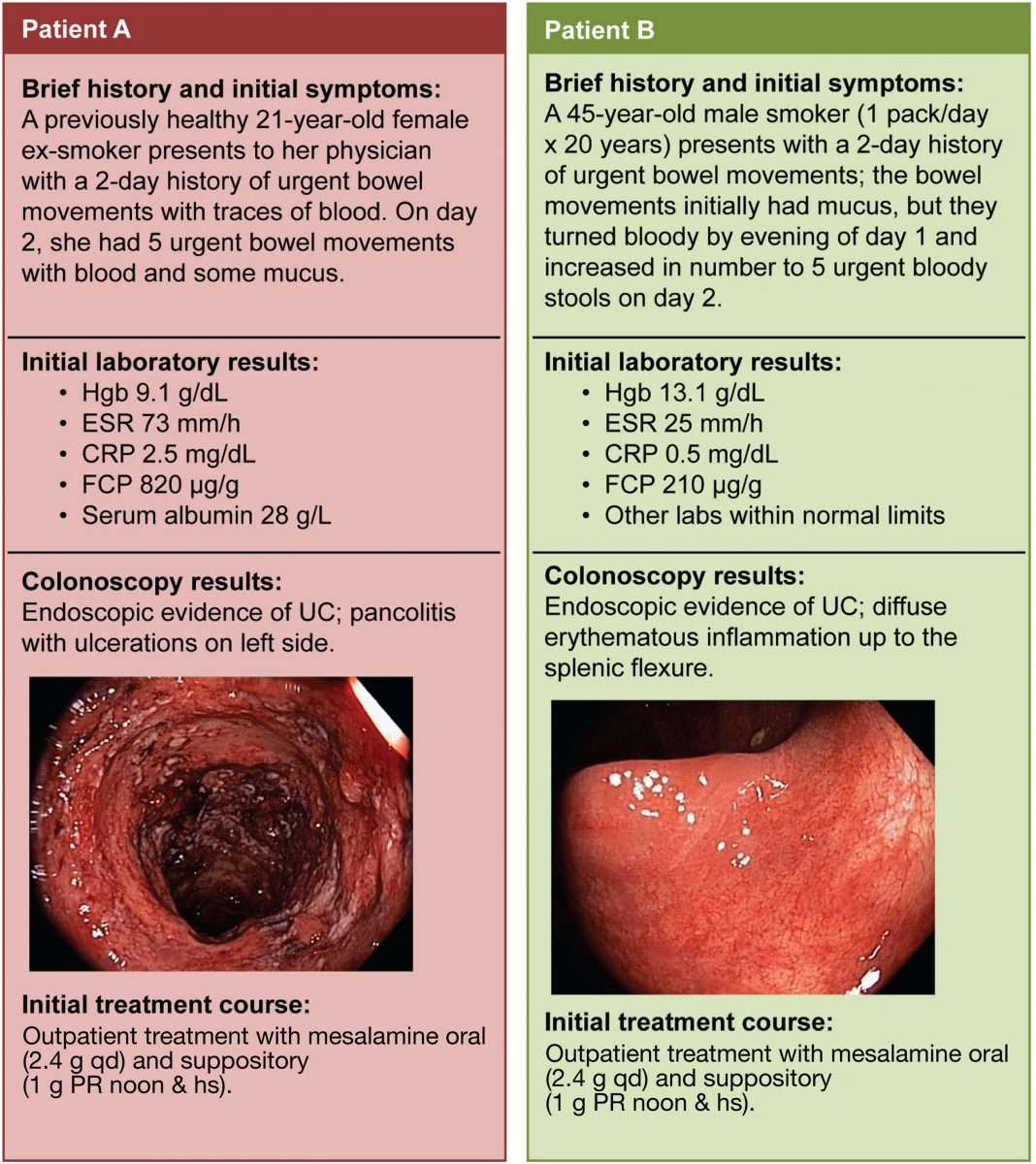
Your doctor may conduct a physical exam, get a history of the symptoms you suffer from and request for a number of tests. These diagnostic tests and procedures are done to differentiate and confirm it is ulcerative colitis and not another disease like the irritable bowel syndrome, Crohns disease or diverticulitis.To confirm the diagnosis following ulcerative colitis tests are conducted:
Ulcerative colitis tests can be suspected when a patient suffers from rectal bleeding, diarrhea, and severe abdominal pain. The blood tests done for ulcerative colitis may indicate anemia and signs of inflammation in the body. If it is suspected that the patient suffers from ulcerative colitis, an endoscopy would be recommended.
Endoscopy is one of the important diagnostic tests to determine ulcerative colitis. In this test, a small, flexible tube with a fiber optic camera is put into the rectum and the colon. This scope will then take images of the inner lining of the rectum and colon to check for signs of ulcers and inflammation inside. A biopsy of the inner lining tissue might also be done to check for the abnormalities of tissue.A barium X-ray can also help in determining the exact portion of the colon affected by ulcerative colitis.
Diagnostic And Differential Diagnostic Value
Previous studies have valued the usefulness of routine laboratory testing in UC. CRP is a helpful index of UC activity, but its utility, as a screening test has not been totally evaluated.
CRP is the most sensitive compared to other serologic markers of inflammation in adult population for detecting IBD. The sensitivity of CRP ranges from 70%-100% in the differential diagnosis between CD versus irritable bowel syndrome and from 50%-60% in UC. In high percentage of paediatric patients, the sensitivity of routine testing , varies from 62%-91% when evaluating the combination of 2 routine laboratory tests, whereas specificity ranged from 75%-94%.
Levels of CRP are higher in active CD than in UC and this difference might be used to differentiate between CD and UC. The measurements of circulating levels of CRP, ESR, platelets count are not useful at all for differentiation between both types of IBD.
Orosomucoid is not useful test for screening healthy populations or differentiating patients with inflammatory vs functional disorders.
The clinical usefulness of pANCA or ASCA testing in patients with non-specific gastrointestinal symptoms is limited, because of the low sensitivity. Assaying all the serum markers available for CD, the sensitivity for the diagnosis of CD is greater than 80% and the positive predictive value is over 90% but only when the prevalence of CD is > 38%.
Don’t Miss: Signs Of Ulcerative Colitis In Child
What Procedures And Tests Diagnose Crohns Disease And Ulcerative Colitis
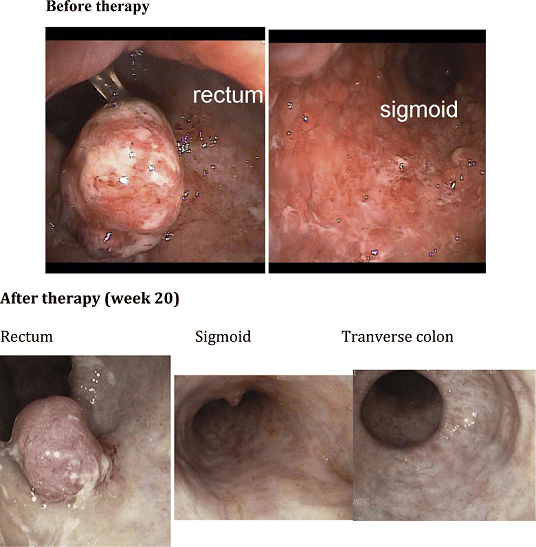
Doctors diagnose ulcerative colitis by endoscopy . During this procedure the doctor can see and take pictures of the patients abnormal gut mucosa , and the presence of continuous disease . Other blood tests and imaging tests like CT scan or MRI are used, but these tests are not definitive.
Doctors use the same procedures and tests to diagnose Crohns disease. However, they also use small bowel studies, colonoscopy, and upper GI endoscopy to identify the abnormal gut mucosa that usually occur in multiple areas anywhere in the intestinal tract. These areas are not continuous, but are separated by normal areas of intestinal mucosa that distinguish them from ulcerative colitis lesions.
As with Crohns disease, nutrition is important if you have ulcerative colitis because symptoms of diarrhea and bleeding can lead to dehydration, electrolyte imbalance, and loss of nutrients. It may be necessary to take nutritional supplements if your symptoms do not allow you to eat a nutritionally balanced diet. Talk to your health-care professional about what supplements to take.
Recommended Reading: Signs Of Having A Stomach Ulcer
Ulcerative Colitis And Colorectal Cancer
Ulcerative colitis increases the risk of colorectal cancer. Colorectal cancer often begins as small growths on the inside of the large intestine. The risk of colorectal cancer increases based on:
- the length of time a person has had ulcerative colitis
- how much of the colon is affected by ulcerative colitis
People with ulcerative colitis should have more frequent tests for polyps and colorectal cancer than people at average risk. The gold standard screening test is a colonoscopy. Polyps can be removed during a colonoscopy. This reduces the risk of colorectal cancer. Ask your doctor how often you should be checked for colorectal cancer.
Surgery to remove the entire colon eliminates the risk of colon cancer.
Also Check: Natural Medicine For Ulcerative Colitis
Watch A Video On Uc Testing And Disease Management
Understanding ulcerative colitis, or UC, doesnt stop at the diagnosis.
Its important to understand testing and disease management, too. We know this can be a lot, but youve got this.
Your doctor will discuss with you the proper tests that can help you find the proper treatment to manage your UC.
Because UC can progress over time, its important to ask your doctor how routine testing after diagnosis may help ensure your treatment is working.
Often together, doctors may test your blood, test biological molecules, called biomarkers, and take images throughout your body.
The results, along with the severity and area of inflammation in your large intestine, may influence how you manage your disease.
Prescription medication can be a common option to treat inflammation in your large intestine. Your doctor may suggest a range of things from changing your diet to surgery.
Ongoing testing is part of disease management, just like treatment.
Knowing more means you can do more. Youre in control of your condition, and now that youre in the know, you can better manage your UC.
When youre living with UC, tests are a routine part of taking care of yourself and managing your condition. Watch this video to understand the basics and help prepare for future visits to your gastroenterologist.
Vitamin B12 And Folic Acid
Vitamin B12 and vitamin B9 are both important for your health. They are vitamins that cannot be made in your body, so you need to get them from the food you eat.
Vitamin B12 and folic acid are used to make red blood cells. Both vitamin B12 and folic acid are absorbed into the body in the small bowel . People who have had their ileum removed or who have inflammation in that area can have difficulties absorbing vitamin B12 from food. This means that many people with Crohns, and some with Colitis, may have a vitamin B12 or folic acid deficiency. When having a vitamin B12 and folic acid test, your doctor will ask about any medicines you are taking.
You May Like: How To Cure Mouth Ulcer Permanently
What Symptoms Should Prompt A Trip To The Doctor
So, we know that bloody diarrhea is probably what will get you into the doctor quickly, but its good to understand why its happening in the first place. When UC inflames your colon, it cant perform one of its chief functions: absorbing liquid from the waste products moving through your system. Too much water in the waste? Thats diarrhea.
But wheres the blood coming from? Its those open sores. It isnt uncommon for people with ulcerative colitis to feel the strong urge to go to the bathroom and discover its just blood theyre passing . Over time, the blood loss can even lead to anemia and fatigue, according to the Crohns and Colitis Foundation. Thats why its really important to see a gastroenterologist if any of these symptoms sound familiar. Other symptoms to take note of include abdominal pain and cramping, the inability to go poop despite feeling like you need to, and sometimes even pus in the diarrhea.
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
Also Check: Types Of Steroids For Ulcerative Colitis
Also Check: Best Toothpaste For Mouth Ulcers
Who Gets Ulcerative Colitis And What Causes It
Colitis can develop at any age, but usually first appears in people aged 15 to 30.
Experts are not sure why UC or Crohn’s disease occurs in some people. It may be due to a combination of genetic, environmental and infectious factors that cause a fault in the immune system leading to inflammation of the bowel.
Microscopic Featuresappraisal Of The Diagnosis

4.3.1 Early stage disease
It has been proposed that a non-specific increase in the inflammatory infiltrate in the lamina propria in combination with absent crypt architectural distortion, indicates a diagnosis of acute, infective colitis, rather than UC. This finding, however, is not confirmed in those studies of patients with early onset colitis .,
Basal plasmacytosis at the initial onset has a high predictive value for the diagnosis of IBD Repeat biopsies after an interval may help to solve differential diagnostic problems and establish a definitive diagnosis especially in adults, by showing additional features
Basal plasmacytosis is observed in biopsies obtained at early onset in 38100% of adult patients, and can help differentiate between UC and infectious colitis. It is particularly a feature in young children in these cases it is notably present in rectal biopsies and decreases proximally. It is an early feature, sometimes the first lesion to appear,,,, and a good predictive marker.
In young children or patients with an aberrant presentation of colitis, UC should always be considered in the differential diagnosis even if the pathology is not typical
Reliable diagnostic features may be absent from biopsies obtained in early onset disease, in acute severe colitis, or in patients with an atypical immunological response . The routine use of additional techniques such as immunohistochemistry is not recommended at present.
4.3.2 Established disease
Recommended Reading: What To Eat During An Ulcerative Colitis Flare
Treatment Of Ulcerative Colitis
Ulcerative colitis is a chronic condition that requires proper treatment to reduce inflammation and prevent the symptoms from worsening.
Several drugs and medications are used to treat UC. The type depends upon the severity of the condition. A medication that works for someone may not work for other people, so sometimes it takes time to identify a proper medication that helps you.
Reasons To Be Open And Honest With Your Doctor
Having a good relationship with the right specialist for your UC can help you both have a clear idea of what is going on with your body and how to manage it.
Your doctor relies on what you tell him or her to get the full picture of how your disease is affecting your life. Use resources like the Doctor Discussion Guide to help make appointments go a little more seamlessly.
When you and your doctor have a good sense of whats going on with your UC, youll be able to confidently move toward a treatment plan thats right for you.
Learn about treatment options for ulcerative colitis.
Recommended Reading: Crohn’s And Ulcerative Colitis Diet
How Is Ulcerative Colitis Diagnosed
Colitis shares many symptoms with other common conditions, such as Crohn’s disease, irritable bowel syndrome, gastroenteritis and coeliac disease. Your doctor will examine you and take a detailed history of your symptoms to help rule these out.
There is no single test that can be used to diagnose UC, so a combination of tests is usually required:
- Blood tests help to rule out other medical conditions, and certain markers in the blood can indicate that inflammation is present.
- A stool sample may find other possible causes of diarrhoea and inflammation, such as an infection.
- A colonoscopy may be performed, where a thin, flexible tube that contains a tiny camera looks inside the bowel for ulcers, inflammation and bleeding.
- A biopsy may be taken from inside the bowel so a pathologist can examine it under a microscope to look for signs of disease.
Other types of imaging are sometimes used to help in the diagnosis and to help rule out other diseases.
Family And Medical History
A physical examination can involve:
- checking the persons blood pressure, temperature, and heart rate
- listening to the persons stomach with a stethoscope
- checking for tenderness or lumps by pressing on the persons stomach
Sometimes, the doctor may also carry out a digital rectal examination. This means gently inserting a lubricated finger into the rectum to check for signs of ulcerative colitis.
You May Like: Can Diverticulitis Cause Ulcerative Colitis
Don’t Miss: Signs Of An Ulcer In A Woman
Living Positively With Ulcerative Colitis
Ulcerative colitis is a chronic condition with symptoms that can disappear and then flare up again throughout your life. Living with the unpredictable nature of ulcerative colitis can pose physical and emotional challenges that may seem overwhelming at times. However, there are several things that you can do to contribute to your health and well-being.
Be informed, proactive, and involved in your care. By establishing a solid partnership with your health care team, developing coping skills, and maintaining a positive outlook, it is possible to stay healthy and happy, despite living with ulcerative colitis.
Also Check: Foods To Avoid With Ulcers And Gastritis
How Do I Prepare For A Sigmoidoscopy Or Colonoscopy
Truly the worst part of these tests is the prep you have to do before. Both require that you follow a special diet before the procedurethink clear liquidsand take a laxative, to effectively clean out your colon for the scope. You may also be asked to fast for a period of time and use an enema to flush out anything that remains in your colon . Your doctor may also need to adjust your medication schedule, if you take any, according to the Mayo Clinic.
Don’t Miss: Ulcerating Breast Cancer Life Expectancy
Can I Prevent Ulcerative Colitis
There is currently no known way to prevent or cure for ulcerative colitis but the proper strategy for managing your disease can help you lead a happier, healthier, fulfilling life.
The exact cause of ulcerative colitis is unknown. However, it is believed to be due to a combination of factors, including a persons genes and triggers in the environment. This interaction of genetic and environmental factors activates an abnormal response of the bodys immune system.
Normally, the immune system protects the body from infection. In people with ulcerative colitis, however, the immune system can mistake microbes , food, and other material in the intestines, as invading substances.
When this happens, the body launches an attack, sending white blood cells into the lining of the intestines where they cause inflammation and ulcerations.
You May Like: When Was Ulcerative Colitis Discovered
Complications Of Ulcerative Colitis
A small number of people with colitis can develop inflammation in other parts of the body, such as the liver, skin, joints and eyes.
Regular monitoring by a gastroenterologist, as well as colonoscopies, may help prevent complications from developing. But medications, including steroids and drugs designed to prevent inflammation and occasionally surgery may be needed.
Osteoporosis can develop as a side effect of long-term corticosteroid use.
Cases of marked inflammation caused by UC can also lead to:
- nutritional deficiencies
- heavy bleeding due to deep ulcers
- perforation of the bowel
- problems with the bile ducts, affecting the liver
- fulminant colitis and toxic megacolon, conditions that cause the bowel to stop working
In the long-term, UC is associated with an increased risk of developing bowel cancer. After 10 years the risk of bowel cancer is 1 in 50, and after 20 years it increases to 1 in 12. This risk can be decreased by maintaining a healthy diet, exercising and avoiding alcohol and smoking.
Also Check: Healing Ulcerative Colitis With Plant Based Diet