Teaching Your Child To Make Food Choices
When children eat healthy, they are more likely to follow good habits as an adult. Teaching your child to be involved in their food habits is important as they grown into young adulthood and beyond. For kids with IBD, meal planning, eating out, and food shopping may involve a little more preparation. Remind them that eating healthy can give them: more energy, better concentration, and help them feel better overall. Eating healthy can also improve behavior, and absorption of medications. Here are some tips to begin getting your child more involved in their food decisions:
Video Length00:01:44
Talkin’ Trish: IBD Nutrition Tips and Tricks Meet Trish, a teen with IBD and lots of personality. In her show, Talkin Trish she talks to kids who have IBD and answers their questions about IBD and nutrition. Today’s topic: IBD nutrition tips and tricks.
Learn more:
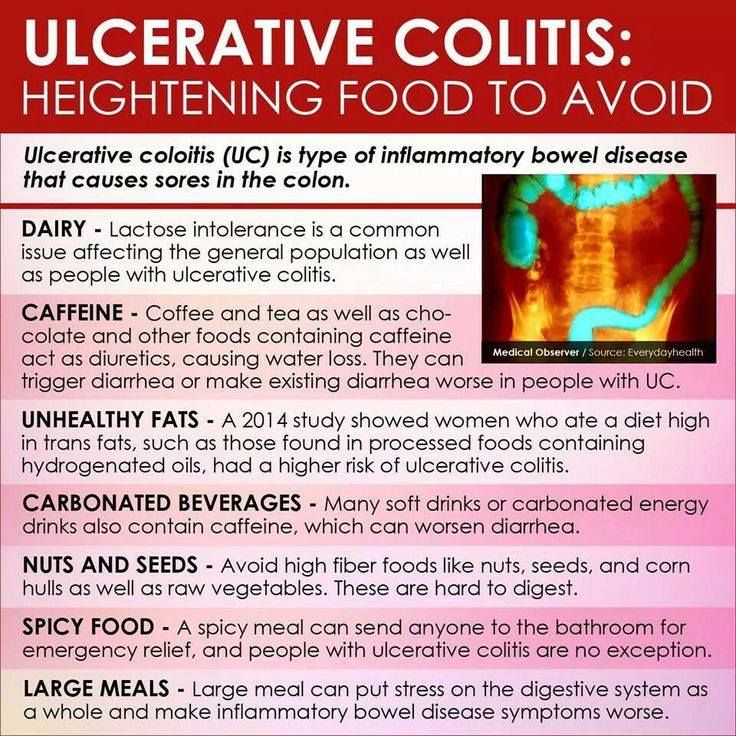
Nutritious Foods To Combat Ulcerative Colitis Complications
People with ulcerative colitis commonly experience anemia and unintended weight loss. Anemia is a low red blood cell count caused by chronic blood loss. It can cause fatigue unless treated. For this reason, the nutrients folate, magnesium, calcium, and iron are of special importance for individuals with UC.
Furthermore, steroid medications such as prednisone may contribute to risk of osteoporosis, which puts emphasis on dietary intake of calcium, vitamin D, magnesium, and vitamin K. Here are the vital body functions that depend on each of these nutrients, along with food sources rich in each.
Calcium
Calcium is important for healthy bones, teeth, and the heart. The best food sources include dairy products, such as yogurt, milk, cottage cheese, and more. Nondairy sources of calcium include sardines , fortified soy milk and almond milk, tofu, kale, broccoli, and chia seeds.
Folate
Folate is crucial for cell division and DNA synthesis. It is found in avocados, black-eyed peas, spinach, Brussels sprouts, asparagus, and fortified breakfast cereals.
Iron
Iron is an important mineral that helps transport oxygen in red blood cells from the lungs to body tissues. It is found in fortified breakfast cereals, tofu, spinach, lentils, chickpeas, and cashews.
Magnesium
Magnesium is an important electrolyte that may be lost through sweating or diarrhea. Foods such as halibut, nuts, nut butters, spinach, potatoes with skin, black-eyed peas, and spinach are rich in magnesium.
Vitamin D
How To Begin Including Smoothies In Your Diet
Start simple. You might be excited to eat these nutritious foods, but be careful to add only one new ingredient at a time. For example, if you tolerate bananas and almond milk then make a banana almond milk smoothie. From there, add blueberries. Did that work well? Great! Now add a handful of spinach. You get the gist.
While its tempting to become a creature of habit and eat your same favorite smoothie every day, I encourage you to mix things up. A key part of healthy eating is variety so youll want to incorporate all the colors of the rainbow. Plus, eating the same food every day when the gut is unwell can increase your risk of becoming sensitive to it.
Read Also: What To Take If You Have A Stomach Ulcer
Also Check: Ulcerative Colitis Caused By Alcohol
Keeping A Food Journal
Everyones body is different, so its possible for two people who have UC to have different trigger foods.
Logging what you eat throughout the day and when digestive issues occur can help you and your doctor narrow down your personal food triggers.
A food journal can be especially helpful if youre trying a new diet.
Whats The Role Of Fiber In Crohns
Dietary fiber is important for your overall health. It can help you keep your cholesterol, blood pressure, and weight at healthy levels. And getting about 23 grams of fiber a day can cut your risk of a Crohnâs flare by as much as 40%. But while youâre having a flare, high-fiber foods can aggravate your symptoms.
The best fiber choices when you have Crohnâs are foods that contain soluble fiber. Soluble fiber soaks up extra fluid in your gut. Foods rich in soluble fiber can help you slow down your digestion and ease diarrhea. The other kind of fiber, insoluble fiber, can boost the amount of water in your gut. Youâll digest foods quickly. That can lead to watery diarrhea, stomach cramps, or gas. At worst, too much insoluble fiber can cause a blockage.
Foods that come from plants are the best source of fiber. This includes fruits, vegetables, grains, beans, and nuts. Most plant-based foods contain both soluble and insoluble fiber. Remove peels, skin, and seeds of fruits or veggies to cut down on insoluble fiber. And check labels for added fiber in foods you wouldnât expect, like dairy products.
During times when you donât have active Crohnâs symptoms, choose whole grains and a variety of fresh fruits and vegetables.
Read Also: How To Fix Mouth Ulcers
Also Check: Stage Iv Sacral Decubitus Ulcer
I Have Heard That Fiber Is Good For Ulcerative Colitis What Does Onpoint Say
-
We encourage you to eat a medium/high fiber diet when you are not experiencing a flare up. A high fiber diet is almost always encouraged in all adults, part of maintaining a healthy gut as well
-
If you decide to increase your fiber intake, increase it gradually, even if you are not having GI or IBD issues presently
-
You may find a “Low Residue” approach helpful. We have seen it work well for some people
-
Increase or be aware of hydration and fluid intake. Try to drink at least 64 oz of water per day
-
Some studies show that a higher fiber diet can improve IBD conditions
Dried Pineapple And Coconut Dates
Dried fruits and coconut dates are available at most grocery and health food stores.
High in sugar and not for those who arent well-healed, dried fruits can be a welcome sweet treat in an otherwise strict Paleo-AIP food plan.
Treat them like candy and eat them sparingly when you need a treat.
Dried fruits are loaded with carbs and sugar. They can trigger diarrhea or a flare-up. Too much of these, especially the pineapple, can really get you into gastrointestinal discomfort.
Some dried fruits may not work for you at all. Test them individually and be careful.
Read Also: Foods To Eat During Ulcerative Colitis Flare Up
You May Like: Best Diet For Ulcerative Colitis Flare Up
Nutrition Tips For Inflammatory Bowel Disease
Inflammatory Bowel Disease is a term used for two specific and separate diseases: Crohn’s disease and ulcerative colitis. Nutritional recommendations are different for each disease and for each individual patient. It is important to discuss the treatments that are right for you with a registered dietitian and with your doctor.
Ulcerative Colitis Diets You Might Try
So much research still needs to be done to find the ideal combination of foods that will keep IBD in remission, but you can work with a gastroenterologist or registered dietitian to find what works for you.
That may require a lot of trial and error, so be patient with yourself.
Some of the diets experts recommend are:
Read Also: How Do You Develop Stomach Ulcers
Peeled Or Poached Fruit
Removing the skin or peel from a piece of fruit can reduce the amount of insoluble fibers, such as lignin and cellulose.
Poaching and preserving fruit can also decrease the amount of fiber. Generally, the more processing fruit goes through, the easier it is for the body to digest.
Canned and cooked fruits are often low in fiber, but they can contain high amounts of sugar, so eat them in moderation.
One Syllable Describing Words
To diagnose ulcerative colitis, doctors review medical and family history, perform a physical exam, and order medical tests. Doctors order tests to. confirm the diagnosis of ulcerative colitis. find out how severe ulcerative colitis is and how much of the large intestine is affected. rule out other health problemssuch as infections.
The ongoing coronavirus disease 2019 pandemic, caused by severe acute respiratory syndrome coronavirus 2, represents a potentially major challenge to patients with immune-mediated inflammatory diseases who are treated with immunomodulatory therapies. We report the case of an 18-year-old ulcerative colitis patient in sustained clinical remission who 4 days.
Ulcerative colitis is an inflammatory bowel disease that causes long-lasting inflammation and ulcers in your digestive tract. Ulcerative colitis affects the innermost.
COVID-19 Resource Center. Review the latest information on visitor policies, safety procedures, … Ulcerative colitis is an autoimmune disease and inflammatory bowel disorder that affects the large intestine and rectum. Although it can begin at any age, it often starts in young adulthood. … Monitoring diet to limit foods that cause.
Read Also: Is Constipation A Symptom Of Ulcerative Colitis
How To Receive Collect Calls From Jail On A Cell Phone
gramsims cc folder
aboriginal cultural heritage nsw
In humans, some of these viruses are common and cause mild symptoms like the common cold, while other types of human strains can be more severe. A new coronavirus affecting humans, named SARS-CoV-2, was identified at the end of 2019. SARS-CoV-2 causes COVID-19. Reported COVID-19 cases have ranged from mild to severe, including death.
Research suggests that most people taking immunosuppressants for IBD are still able to mount an immune response to the COVID-19 vaccine. Health Conditions Featured.
Both Crohn’s disease and ulcerative colitis – the two main forms of IBD — cause chronic inflammation in the intestines, triggering symptoms like abdominal pain, diarrhea and weight loss. The.
Symptoms of disease flare that can mimic COVID-19 The clinical presentation of several gastrointestinal diseases can mimic COVID-19 infection . Examples include diseases that manifest with diarrhea, nausea, vomiting and/or anorexia . Thus, for patients with an existing diagnosis of chronic GI disease, the clinician will need to assess whether symptoms are related to a disease flare or COVID-19.
vashon island restaurants on the water
- Additional shared or linked blogs.
- Invites to industry events .
- Even entire buyouts of companies.
Are Nutritional Needs Different For People With Ibd What Are The Specific Nutritional Needs For People With Crohn’s Disease And Ulcerative Colitis
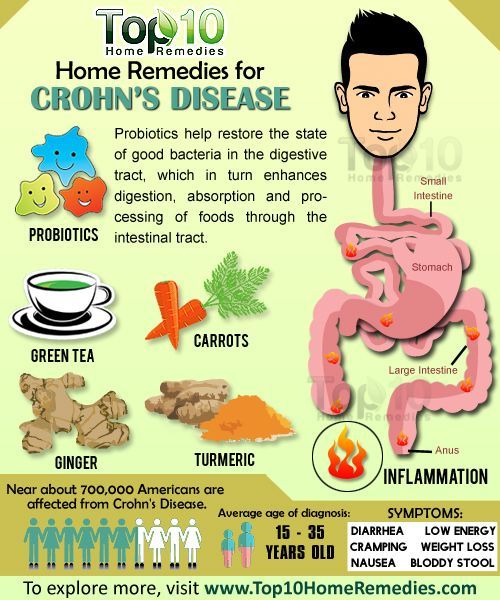
Nutritional needs are specific to the individual and differ with disease state, body size and age. A nutritionist can help you estimate your individual needs. Calorie and protein needs are similar for Crohn’s disease and ulcerative colitis. In both diseases, needs increase during inflammation and immediately after to restore losses. The following are general statements about nutritional needs that may apply to you.
Also Check: Calcium Alginate For Pressure Ulcers
It Can Be Challenging To Differentiate Between Crohn’s And Ulcerative Colitis
Our summary of the two conditions is below. You can also read a more detailed explanation about the differences between Colitis and Crohn’s Disease here.
|
|
Our summary of the two conditions is below. You can also read a more detailed explanation about the differences between Colitis and Crohn’s Disease here.
Diet Progression Following Flares For Ulcerative Colitis And Crohn’s Disease
- Continue to follow a low residue diet and slowly add back a variety of foods.
- Begin with well-tolerated liquids and advance to soft solids, then solids .
- Introduce one or two items every few days and avoid any foods that cause symptoms.
- Add fiber to diet as tolerated. Well-tolerated fiber sources include tender cooked vegetables, canned or cooked fruits, and starches like cooked cereals and whole wheat noodles and tortillas.
- Between flares, eat a wide variety of foods as tolerated. This includes fruits, vegetables, whole grains, lean protein, and low-fat and nonfat dairy products.
- Increase your calorie and protein intake following a flare. Abdominal pain, diarrhea and decreased appetite may have caused poor food intake. Steroids used to treat flares also can increase protein needs.
Suggestions for first foods after a flare include:
Don’t Miss: Food To Avoid For Ulcer Patient
Crohns Disease And Ulcerative Colitis And Diet
Diet and food allergies do not cause IBD, and long-term special diets are not effective in treating IBD. However, adjusting your diet can help manage some of your symptoms, and can help IBD medications work better. A person with IBD has to pay close attention to their diet, since they may have malnutrition.
Are Any Special Minerals Recommended
In most IBD patients, there is no obvious lack of minerals. However, iron deficiency is fairly common in people with ulcerative colitis and Crohn’s colitis and less common in those with small intestine disease. It results from blood loss following inflammation and ulceration of the colon. Blood iron levels are easily measured, and if a deficiency is found , oral iron tablets or liquid may be given. The usual dose is 300 mg, taken one to three times a day-depending on the extent of the deficiency and the patient’s tolerance. Oral iron turns the stool black, which can be mistaken for intestinal bleeding.
Other mineral deficiencies include potassium and magnesium. People may develop potassium deficiencies with diarrhea or vomiting, or as a result of prednisone therapy. Potassium supplements are available in tablet and other forms. Oral supplements of magnesium oxide may prove necessary for people who have magnesium deficiency caused by chronic diarrhea or extensive small intestinal disease, or those who have had substantial lengths of intestine removed through surgery.
Trace elements are nutrients that are absorbed in the body in minute quantities. Still, they are essential for some important biologic functions. Deficiencies in trace elements are noted in people with advanced Crohn’s disease-mainly those with poor nutritional intake and extensive small intestine disease.
Also Check: Do Ulcers Give You Diarrhea
Rule Number 3 Eliminate Gluten And Dairy Generally
Gluten, or more specifically gliadin, stimulates zonulin production that in turn increases intestinal permeability, AKA Leaky Gut.
This increased gut permeability makes us more susceptible to an autoimmune response.
This post isnt meant to be a science lesson, but you can check this study out if you want to learn a little more about the process itself.
Noteworthily, several studies have also found that the casein protein in dairy behaves similarly to gluten / gliadin in our guts, and may also promote leaky gut.
This would explain why coeliacs often show cross-reactivity to many dairy products.
And to be very plain for a second, pretty much everyone whos been diagnosed with ulcerative colitis or Crohns disease has experienced gluten and/or casein being problematic at least on occasion.
^ That very basic fact is important.
Its important to add though, that not all dairy is created equal.
In fact, certain types of fermented dairy have actually been shown to improve serum zonulin levels and may help to improve leaky gut. See here.
And we could also muddy the water even more and say that other lectins and lectin-like proteins can also cause issues..
But, Im here to give you the broad brush strokes and attempt to simplify things.
So to keep it basic
Stay away from dairy and gluten and youll be off to a good start.
Recommended Reading: Signs You Have A Stomach Ulcer
What Foods Should You Eat With Ulcerative Colitis
If you have Ulcerative Colitis, very minor changes to what you eat can make a BIG difference in your symptoms. Consider keeping food logs or adjusting foods that trigger your symptoms. You may also want to work with your doctor or dietitian to work through an elimination diet. Generally, you should try to:
In terms of specific food recommendations, go with these:
| Food Type |
|---|
|
|
During a flare up, you many find it more comfortable to eat bland, soft food, otherwise limiting spicy foods. During periods of remission, you should eat all of your usual items with the omission of known offenders.
Don’t Miss: What Causes An Ulcer In Your Eye
Crohns Disease And Body Pain
Crohns Disease pain originates from inflammation in the digestive tract and can spread systemically throughout your body.
Most people . Additionally, some people may also experience pain in peripheral parts of the body such as their joints and eyes.
Each person perceives pain differently, and thus describes their pain in different ways. We list common pain descriptors below:
- A Charley Horse in your gut
While not all people with Crohns Disease will experience pain in other areas, almost all people with Crohns Disease will experience GI pain at some point in their life especially if the condition is not treated.
Recommended Reading: Diet If You Have An Ulcer
What To Eat On A Crohns Diet During Remission:
What you should eat on a crohns diet plan is very individual but lets get acquainted with what it takes to be on a Crohns diet plan when your disease is not active:
-
Eat a variety of vegetables and fruits
-
Get enough calcium
-
Drink plenty of fluids
Your Crohns diet plan can even be more liberal when your symptoms subside but remember to:
-
Go slowly Gradually add more foods back into your diet. Shift to whole grains and those colorful veggies and fruits. Start with small amounts of these foods. If your symptoms act up, add that item to your potential list of trigger foods. You can try eating that food at a later time.
-
Eat 5 or 6 small meals per day Go easy on your GI tract. Large meals can flare your symptoms and make you feel bloated.
-
Stay well hydrated Sip on water throughout the day. As you add back in fiber, getting enough to drink is important. Fiber without adequate fluid intake can lead to constipation.
-
Avoid your trigger foods. Focus on the foods you can eat and enjoy. Create a list of substitutions for your trigger foods.
Also Check: What Over The Counter Medicine For Ulcers