Fatty Acids In Diet Affect Ulcerative Colitis Risk
By Anne Harding, Reuters Health
3 Min Read
NEW YORK – People who eat lots of red meat, cook with certain types of oil, and use some kinds of polyunsaturated fatty acid -heavy margarines may be increasing their risk of a painful inflammatory bowel disease, a study in more than 200,000 Europeans shows.
These foods are high in linoleic acid and the study have found that people who were the heaviest consumers of this omega-6 PUFA were more than twice as likely to develop ulcerative colitis as those who consumed the least.
Dr. Andrew Hart of the University of East Anglia in Norwich, UK, and his colleagues also found that eating more eicosapentaenoic acid, an omega-3 fatty acid found in fish and fish oils, was associated with a lower risk of the disease.
While people need a certain amount of linoleic acid to survive, Hart noted in an interview with Reuters Health, excess amounts are taken up into the lining of the colon, and if theyre released, they can promote inflammation. Omega-3 fatty acid, he added, does the opposite. It basically dampens down inflammation, he explained.
To investigate the role of fatty acids and ulcerative colitis, a life-long disease characterized by inflammation of the lining of the large intestine, Hart and his colleagues looked at data from the European Prospective Investigation into Cancer and Nutrition trial, which includes over half a million people from 10 European countries.
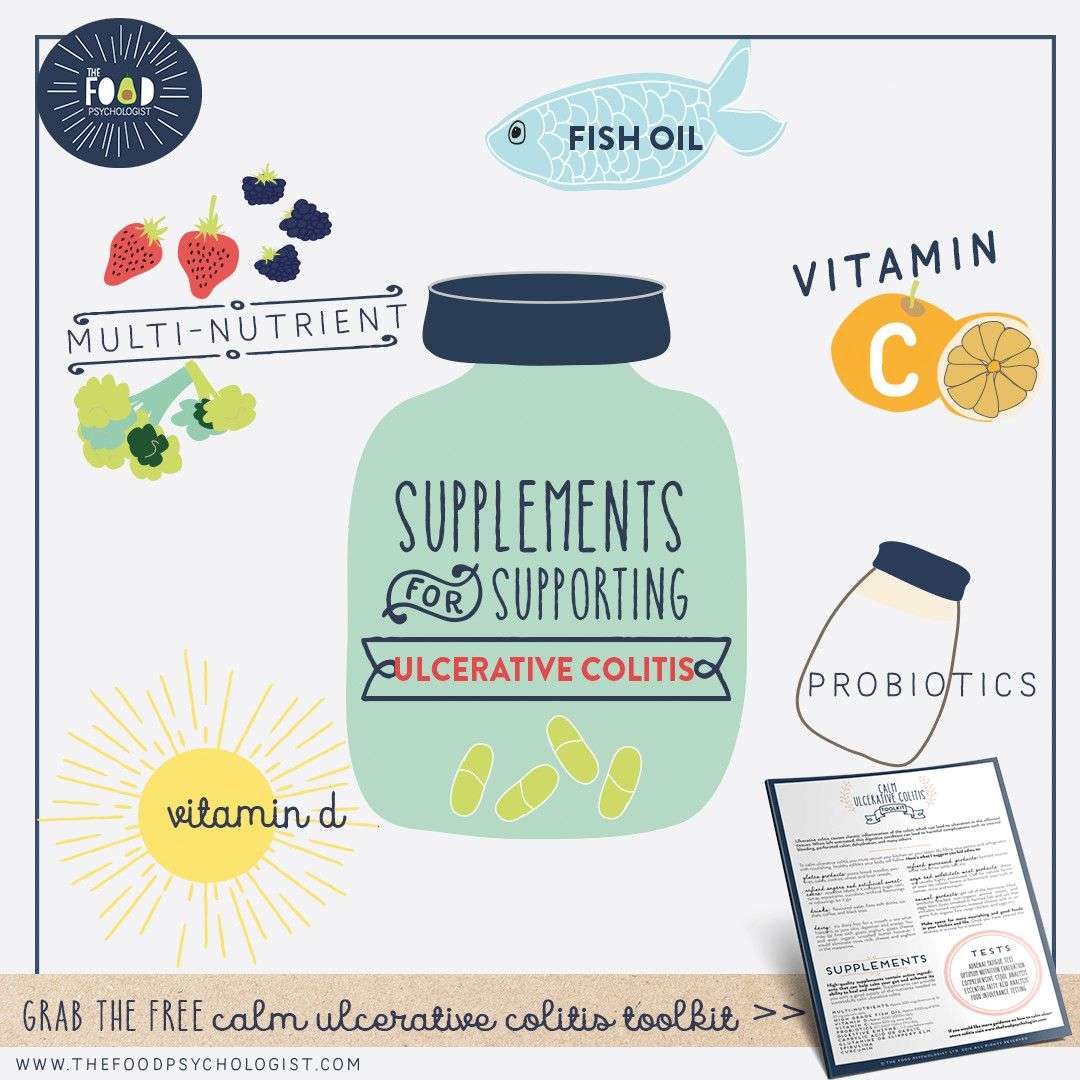
Supplements Being Studied For Ulcerative Colitis
Researchers are checking a number of supplements to see if they can help people with UC. In at least one study, omega-3 fatty acids found in fish oil reduced symptoms and prevented UC from returning. Other studies, however, have not had the same results.
Probiotics are “good” bacteria or other microorganisms that can be healthful. Several studies show they reduce ulcerative colitis symptoms. The thinking is that probiotics, like lactobacillus or live-culture yogurt, help to restore balance to the good bacteria that live inside the intestines.
A few studies have seen benefits from aloe vera when you take it in the form of a gel that you swallow, but more research is needed to confirm this.
Talk to your doctor about other supplements that are being studied to see if they can help you manage ulcerative colitis.
Show Sources
Colonoscopy And Body Composition
The COLOVIEW mini-endoscopic system was used as previously described . Distal colon was examined along the first 34 cm. Scoring system consists in evaluation of ulceration numbers , vasculature features , mucosal granularity , erythema , pinpoints , fibrin deposition , length involved and overall vulnerability of the colon. Fat and lean body mass were measured with NMR the day before the sacrifice and expressed as% of animal body weight.
Read Also: Natural Home Remedies For Ulcers In Stomach In Tamil
How Can I Live With Chronic Ulcerative Colitis
If you are struggling with colitis or another type of irritable bowel disease, help is available at Gastroenterology Associates of Southwest Florida, PA. Our team provides compassionate, expert care to help patients suffering from these types of chronic conditions. Find out how we can help you live with chronic ulcerative colitis
Helper T Cell And Regulatory T Cell Characterization

Mesenteric lymph node cell suspensions were made to assess in AT mice Th1 and Th17 cells ex vivo as described previously . Th1 cells were CD4+IFN+ whereas Th17 cells were CD4+IL-17+. Additionally, anti-FoxP3 intranuclear staining was made in order to track the generation of so-called CD4+FoxP3+ regulatory T cells. All antibodies were purchased from eBiosciences.
You May Like: What Is Good For Mouth Ulcers
Warning Disclaimer Use For Publication
WARNING: Please DO NOT STOP MEDICATIONS without first consulting a physician since doing so could be hazardous to your health.
DISCLAIMER: All material available on eHealthMe.com is for informational purposes only, and is not a substitute for medical advice, diagnosis, or treatment provided by a qualified healthcare provider. All information is observation-only. Our phase IV clinical studies alone cannot establish cause-effect relationship. Different individuals may respond to medication in different ways. Every effort has been made to ensure that all information is accurate, up-to-date, and complete, but no guarantee is made to that effect. The use of the eHealthMe site and its content is at your own risk.
If you use this eHealthMe study on publication, please acknowledge it with a citation: study title, URL, accessed date.
Coconut Water Can Replenish Electrolytes
After a bout of severe diarrhea, a common Crohns symptom, you may need a little more punch than just plain old water. In this instance, for an IBD like Crohns disease, its best to turn to products with added electrolytes. Coconut water a natural source of electrolytes can make a refreshing change, says Catsos. If you choose another electrolyte replacement beverage, she adds, try to avoid those sweetened with high fructose corn syrup or crystalline fructose, or those with artificial coloring. Talk to your doctor if youre concerned about dehydration.
Also Check: Signs Of A Bleeding Stomach Ulcer
It Can Be Challenging To Differentiate Between Crohns And Uc
Our summary of the two conditions is below. You can also read a more detailed explanation about the differences between Colitis and Crohns Disease here.
|
Our summary of the two conditions is below. You can also read a more detailed explanation about the differences between Colitis and Crohns Disease here.
Herbal Remedies And Supplements
There are lots of supplements that claim to treat Crohns and Colitis. But there isnt enough evidence to recommend any herbal remedies or supplements. This is because its difficult to know whether the supplement is directly affecting a persons Crohns or Colitis or whether something else is causing a change in symptoms. Also, everyone is different so what helps one person may not help another.Some people find that some herbal remedies, such as aloe vera or curcumin , help them manage their symptoms when they use them together with their prescribed medicines. There have been reports of cannabidiol , an ingredient in cannabis, helping with symptoms like diarrhoea, pain and loss of appetite. But we dont know enough about how it works or how much is a safe amount to take. It isnt currently recommended and isnt available on prescription for people with Crohns or Colitis.There have been claims in the media about the benefits of kefir a fermented milk drink that contains probiotics. But there isnt any medical evidence to show that it helps people with Crohns or Colitis.If you want to take herbal remedies, its important to speak to your IBD team or dietitian first. Dont stop taking your prescribed medicine without talking to your IBD team, even if your symptoms improve.
I think it is so important to remember that the relationship with food and IBD is so different for everyone!
Recommended Reading: Preventing Pressure Ulcers In Nursing Homes
Lifestyle Changes To Prevent Ulcerative Colitis
Dealing with colitis flare-up can be approached different ways. Some people have reported that herbal remedies help manage their symptoms. Probiotics, the spice turmeric, and the herb boswellia have been used to control ulcerative colitis. Studies have also shown that gingko biloba has been effective in treating colitis in rodents.
Since stress has been linked to the disease, exercises like yoga and meditation are often recommended to patients. At the same time, certain foods have a higher chance of aggravating ulcerative colitis, so obviously avoiding such food items is a good idea. Some examples of foods to stay away from are whole-grain bread, whole-grain pasta, beans, raw vegetables, and dried fruit. Keeping a diary of what you eat can often help you pinpoint the exact cause of a flare-up.
A diary or journal can also help when you are taking medications. For example, if you experience a flare-up while taking an over-the-counter medication, ask your doctor and/or pharmacist about a possible alternative.
Controlling ulcerative colitis flare-up can take time. Some people will have multiple triggers and wont be able to make all the necessary lifestyle adjustments all at once. Sometimes, just a few changes can make a huge difference though. The following simple steps have proven to help many people tame their flare-ups:
- Drinking small amounts of water throughout the day
- Reducing fatty foods
The Utility Of Pufas In The Management Of Ibd
The aetiology of IBD remains unclear but local mediators including arachidonic acid metabolites, cytokines and altered cell mediated immunity are likely to contribute to the disease. The rationale for the prescription of n-3 PUFA to promote a healthy gastrointestinal tract has been linked to their suggested anti-inflammatory properties. Different strategies have been adopted in various clinical trials to evaluate n-3 PUFA in patients with IBD. Inhibition of natural cytotoxicity, changes in interleukin 2 and arachidonic acid metabolites, e.g., LTB4 are the main chemotactic signals seen in the mucosa during a relapse. All are known to mediate the natural killer activity. A second hypothesis is based on the possible deficiency of essential fatty acids in IBD and its effect on cell membranes. A further possibility is that fish oil ameliorates oxidative stress in IBD.
In a randomised crossover trial from four units which involved 18 patients with ulcerative colitis fish oil supplements reduced LTB4 levels in a rectal dialysate. Histology improved and patients weight increased.
Conversely, a small Canadian trial of 11 patients found that addition of fish oil was of clinical benefit in UC but did not reduce mucosal LTB4. However, over a six month period serum LTB4 was insignificant while there was a simultaneous fall in NK cell cytotoxicity.
Don’t Miss: Cold Laser Therapy For Ulcerative Colitis
Drinking In Moderation Is Fine If You Have Uc
If you like to have a glass of wine or beer with family and friends over a heated fall football match or a festive holiday dinner, you probably dont need to worry about your UC symptoms flaring. Theres no evidence that alcohol increases UC flares, Dr. Hong says . If boozing is a trigger for you, stick to alcohol-free versions of your top tipples.
Diet Progression Following Flares For Ulcerative Colitis And Crohns Disease
- Continue to follow a low residue diet and slowly add back a variety of foods.
- Begin with well-tolerated liquids and advance to soft solids, then solids .
- Introduce one or two items every few days and avoid any foods that cause symptoms.
- Add fiber to diet as tolerated. Well-tolerated fiber sources include tender cooked vegetables, canned or cooked fruits, and starches like cooked cereals and whole wheat noodles and tortillas.
- Between flares, eat a wide variety of foods as tolerated. This includes fruits, vegetables, whole grains, lean protein, and low-fat and nonfat dairy products.
- Increase your calorie and protein intake following a flare. Abdominal pain, diarrhea and decreased appetite may have caused poor food intake. Steroids used to treat flares also can increase protein needs.
Suggestions for first foods after a flare include:
- Diluted juices
Read Also: Best Ulcerative Colitis Diet Book
Also Check: Is Colitis And Ulcerative Colitis The Same Thing
Characteristics Of Included Studies
Jump to:
|
A doubleblind, placebocontrolled randomised study. Parallel group. |
|
|
Participants |
18 outpatients with ulcerative colitis. EFA group : median age 54 . Placebo group : median age 41 . All had distal proctocolitis. Clinical score EFA group: 8 and placebo group: 8 . Excluded were patients currently being treated with systematic steroids, who were pregnant or had a documented immune deficiency disorder. Patients were maintained on their existing longterm medication with sulphasalazine or mesalazine. |
|
Interventions |
Active group: EFA . Placebo group: sunflower oil . Oral route of administration. All oil supplements included 3% tocopherol . A 6 month treatment period. |
|
Outcomes |
Sigmoidoscopic score, histological score, NK cytotoxicity and flow cytometry. Assessments were done at monthly intervals. |
|
Notes |
|
A doubleblind, placebocontrolled, crossover study. |
|
|
Participants |
17 patients , aged 31 to 74 years , with mild to moderate ulcerative colitis. Distribution of disease: pancolitis , distal colitis and proctitis . Oral steroids and sulfasalazine were allowed if the patient had taken them for more than 4 weeks. |
|
Interventions |
Active group: MaxEPA . Placebo group: Corn oil . An 8 month treatment period . Oral route of administration. |
|
Disease activity, clinical and laboratory evaluation, histology and mucosal LTB4 levels. Assessments were done at monthly intervals. |
|
|
Notes |
Quality score = 5. 11 patients completed the study and represented the focus of the report. |
|
Risk of bias |
Tips For Meal Prepping
Now that you have a sense of what to eat for ulcerative colitis, its time to get in the kitchen. Meal prepping some simple ingredients can make your life easier and prevent a UC flare. Here are some simple strategies:
- Buy pre-chopped fruits and veggies. Having produce in your fridge that dont require any preparation will make you more likely to add them to your plate at mealtime.
- Go frozen. Frozen fruits, veggies, and whole grains are generally as nutritious as fresh produce. Buy frozen fruit for smoothies, frozen veggies for soups and casseroles, and frozen grains to heat up in the microwave as a side dish.
- Pick up ready-made proteins. Stock up on simple options, like a rotisserie chicken or canned beans.
- Make a big batch of soup. Not only is soup soothing, its also an easy way to add a ton of veggies to your diet and is super easy to make in big batches.
- Stock up on healthy fats. Load up your cabinet with nuts, oils, and seeds for snacking, cooking, or adding texture to a recipe.
Read Also: Cheap Ulcer Treatment For Horses
Diet Design And Safety Evaluation
In many studies, dietary oils are manipulated in order to modify ratios of n-6:n-3 PUFA. Often, high proportion of FO introduction leads to an increase in LC n-3 PUFA by increasing EPA and DHA intake while LC n-6 PUFA intake is reduced. Thus, the anti-inflammatory effects of FO may result from reduced cell content in LC n-6 PUFA like linoleic acid or arachidonic acid rather than the effect of EPA and DHA per se. Herein, in order to avoid this as a confounding factor, our diet described in Table was designed to maintain LC n-6 PUFA and balanced for essential FA content in the control and experimental diets as analyzed and shown in Table . When wild type mice received this diet for 8 weeks no safety issue was noticed, all animals ate and grew normally. Immune cell subsets analysis by flow-cytometry in primary and secondary lymphoid tissues did not show any perturbation of myeloid cells, B and T lymphocyte development and function . Therefore we decided next to test this diet in a colitis protocol established earlier for colitis prevention . It was given to Rag2/ immune-deficient mice over a 4 week period before inducing IBD by AT of naïve T cells. AT mouse model of colitis was chosen because it is a well established animal model for IBD sharing a number of clinical, genetic and immunological features with the human disease . The animals were kept under the same diet and followed for an extra 4 week period .
Table 1 Composition of the control and experimental diets
How Is Colitis Treated
Medications and surgeries have both helped colitis patients. However, no medication can cure the disease. Colitis typically undergoes several changes during the illness where the patient may experience remission of symptoms where they feel better or flare-ups that cause them to relapse. One of the best ways to manage these ups and downs is to closely monitor the diet to control disease symptoms.
You May Like: Vegetarian Diet For Ulcerative Colitis
List Of Foods To Eat To Keep Colitis From Flaring Up
Colitis is an inflammatory bowel disease. There are several types of colitis, depending on the location of the inflammation. Symptoms vary but commonly include abdominal cramps, bloating, constipation and diarrhea. Theres really no nutritional therapy for colitis, nor is there a cure. But learning to strike a balance between getting the nutrients you need and avoiding the foods that seem to trigger your symptoms can help you manage the condition.
Video of the Day
Read Also: Can You Take Tylenol With Ulcerative Colitis
What Foods Can Trigger A Colitis Flare Up
Food doesnt cause colitis, but it can cause disease symptoms to flare up. While there are medications that can help with symptoms, its important to develop a diet that is right for you to keep your flare-ups to a minimum.
Unfortunately, there is no single diet that we can recommend. Every person is different and over time the disease can change so that the diet stops working even if it was previously keeping you on track. So, where can you start to even figure out what foods trigger a colitis flare-up?
We recommend that patients living with this uncomfortable disease start with a food diary as part of their treatment plan. Staying away from processed foods while preparing whole grains, fresh fruit and vegetables, and lean proteins is a good idea. You may simply need to tweak what youre eating. For example, instead of eating a raw salad, try steamed vegetables. Ease up on spicy foods. Instead of high-fat dairy products, consider a milk substitute such as almond milk. If fiber is causing an increase in symptoms, try lessening your fiber intake to 10 to 15 grams a day. That could potentially help you visit the restroom a little less.
While these are good suggestions, unless youre tracking your specific food intake against how youre feeling, it can be hard to know exactly what will work. Weve seen the following foods consistently cause flare-ups in many patients:
Don’t Miss: Hindgut Ulcers In Horses Treatment