Spoon Up Some Applesauce
Applesauce may be good for an ulcerative colitis diet, according to the University of Wisconsin Health. However, while apples are rich in vitamins and minerals like potassium, their high fiber content can make them difficult to digest, especially during a flare-up, says the Foundation. Go for unsweetened applesauce, or make your own by peeling and cooking apples . Flavor it with your own mix of spices just be sure to skip the sugar.
Track The Good And The Bad
There’s no single diet that will help everyone with UC. The condition can also change over time, so your plan will need to be flexible, too. The key is to find what works for you.
To stay organized, keep a food diary. Use your smartphone or a small notebook to record what you eat and drink and how they make you feel, both good and bad. It takes a bit of time and patience, but it will help you track your condition and fine-tune your diet plan.
When you prepare your meals, don’t forget that a well-balanced diet gives you enough protein, whole grains, and fresh fruits and vegetables.
You might not be able to eat everything in the grocery store or on the menus at the restaurants you like. But try to focus on the ones that you can enjoy without triggering your symptoms. Some simple tweaks in your meal prep can make it easier to eat some foods, like steaming veggies or switching to low-fat dairy.
Some people follow a low-residue diet or low-fiber diet every so often, getting about 10-15 grams of fiber a day. That can help you go to the bathroom less often.
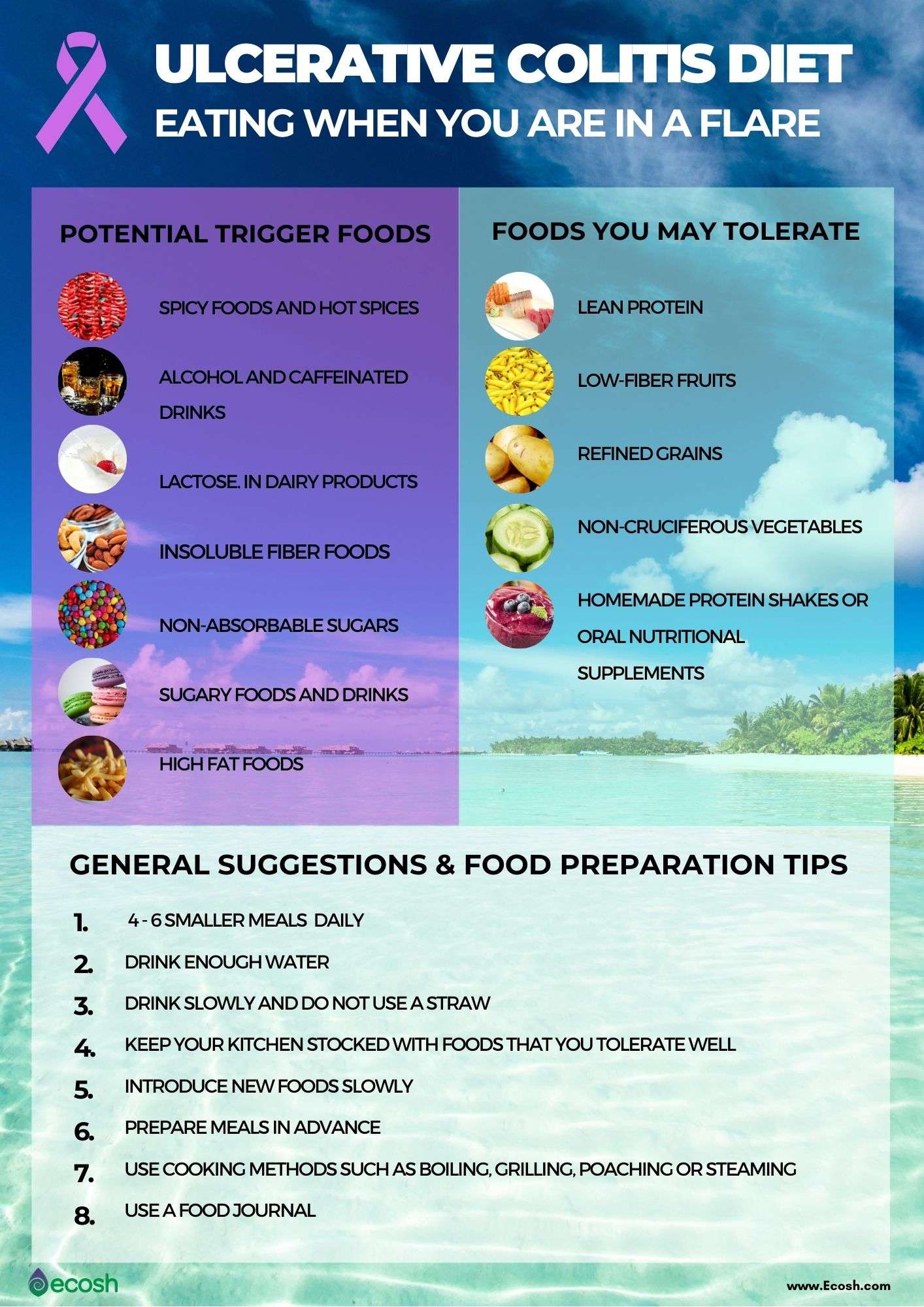
Watch out for items that can be troublemakers if you have UC, including:
- Alcohol
Do Any Medications Have Nutritional Side Effects
Moderate to severe flares of IBD are often treated with corticosteroids , cholestyramine and 5-ASA compounds . These medications have nutritional side effects that should be addressed. If you use any of these medications, talk to your doctor or registered dietitian for treatment advice.
- Prednisone causes decreased absorption of calcium and phosphorus from the small intestine. It also causes increased losses of calcium, zinc, potassium and vitamin C. With continual use of high doses of prednisone, the result may be bone loss and development of bone disease. People on prednisone may need up to 1200 milligrams a day. Protein needs also are increased for people taking prednisone because it increases protein breakdown in the body.
- Cholestyramine decreases absorption of fat-soluble vitamins , as well as folate, vitamin B-12, calcium and iron.
- Sulfasalazine interferes with folate absorption. People taking this drug also should take a 1 milligram folate supplement each day.
Also Check: How Do You Heal An Ulcer
Is Beer Good For Ulcerative Colitis
With UC, you should drink plenty of fluids and water to stay hydrated. But alcohol isn’t a good choice for that because it’s a diuretic, which means it dehydrates your body. Like coffee, alcohol stimulates your bowels and can worsen diarrhea. Carbonated alcoholic drinks like beer can also make you gassy.
Vitamin D For Ulcerative Colitis
People with inflammatory bowel diseases are often deficient in vitamin D and low vitamin D levels are associated with disease severity in the research. It is thought that vitamin D has an important role to play in immunity, helping to modulate the inflammatory response. To support bone health, as well as improve outcomes in ulcerative colitis, I recommend taking vitamin D daily. Ask your doctor how much vitamin D they think you should take in order to get your blood levels up over 75 nmol/L. In the absence of that advice, 2000IU Vitamin D3 daily is a safe and conservative dose and vegan options are now available.
Also Check: Treating Ulcers In Horses With Omeprazole
What Foods Should I Avoid
Certain foods can exacerbate UC flares, but everyone has different trigger foods. For some, it might be a juicy burger and for others, it could be their morning latte.
In general, inflammatory foods, like fast food, processed food, alcohol, and sugary drinks contribute to the development of flares, says Dr. Singh. Freuman adds that saturated fat, specifically, can be an issue for certain people. Foods that contain significant amounts of saturated fat include:
- Coconut oil
- Whole-milk dairy, such as cheese, cream, butter, and full-fat yogurt
- Fried foods
- Red meat
Lactose is the sugar present in milk and dairy products, and lactase is the enzyme people need to break down those sugars during digestion. If someone is lactose-intolerant, it means they dont produce enough lactase to break down the sugars, which can cause cramps, bloating, diarrhea, and gas.
To complicate matters, UC is sometimes coupled with lactose intolerance. But lactose intolerant dairy lovers, take heart: Its often possible to still consume dairy with lower lactose content, like cottage cheese and yogurt. Because these products contain live cultures that produce their own lactase, your body doesnt have to do all the work to break down lactose5.
Thats a win-win, since dairy foods provide important nutrients, like calcium and vitamin D, to your diet. In fact, avoiding them completely is not recommended unless 100% necessary.
Ulcerative Colitis Symptoms And Causes
Ulcerative colitis is thought to develop when a person at genetic risk is exposed to certain environmental stressors.
These environmental stressors either change the ratio of gut bacteria or alter the way the immune system responds to bacteria .
As a result, the immune system attacks the intestinal lining causing inflammation and other symptoms, including:
Read Also: What To Eat When You Have Gastric Ulcer
Finding The Right Uc Diet For You
For those living with ulcerative colitis, choosing the right foods to eat may feel overwhelming. If you are worried you may not be getting enough of one or more nutrients, speak with your gastroenterologist. They may test your blood for nutrient levels to find out whether you are deficient. If you are deficient in any nutrient, your doctor may recommend a safe and effective dietary supplement.
You can also request a referral to a registered dietitian who can work with you to get the most out of the nutrients in the foods youre able to eat. Working with a registered dietitian or nutritionist can also help you navigate life events, such as parties, dining out, vacations, and more. Understanding what triggers your flare-ups life stress or specific foods is important information that a food journal can help you decipher.
The good news is that for people with UC who establish a healthy and safe diet plan, sticking to it often helps them feel better and manage symptoms. Feeling pretty good today, wrote one MyCrohnsAndColitisTeam member. Ive gone lactose- and gluten-free, and symptoms have reduced a lot. Also gave up caffeine. Living on avocado!
You are not alone in your path to finding a safe and healthy diet with ulcerative colitis. When you join MyCrohnsAndColitisTeam, you gain a supportive community of more than 138,000 people living with IBD.
Which Nutrients Are Important In Crohn’s And Colitis
Vitamins and mineralsYour body needs vitamins and minerals to work and stay healthy. Your Crohns or Colitis may stop you absorbing enough vitamins and minerals from your food. Vitamins and minerals that you may not absorb properly include iron, vitamin B12, vitamin D and calcium.Eating a healthy, balanced diet may help improve the level of vitamins and minerals in your body. If blood tests show you have low levels of vitamins and minerals, your doctor or specialist nurse may recommend you take supplements to restore your vitamin and mineral levels.Speak to your doctor, specialist nurse or dietitian if you think you may have low levels of any of these nutrients.
IronHaving low levels of iron is common in people with Crohns or Colitis. Possible causes include a lack of iron in the diet, blood loss and problems absorbing iron from food. Lack of iron can lead to anaemia, where there are fewer red blood cells to carry oxygen around the body.Common symptoms of anaemia include:
- feeling tired and lacking in energy
- feeling short of breath
- fast or irregular heartbeat
- pale skin.
Its important to speak to a dietitian before cutting down on fibre so you dont miss out on the health benefits. For example, they may suggest that some people cut down on fibre for a short time during a flare-up, before slowly adding it back in to the diet.Fibre-rich foods include:
- wind
- stomach rumbling and pain
- diarrhoea loose and runny stools.
- sipping a cold drink
Don’t Miss: Ways To Prevent Pressure Ulcers In Hospitals
What Can I Eat For Breakfast With Colitis
A few stomach-friendly breakfast ideas:
- 1 cup of low-fat cottage cheese with a fruit cup.
- 2 scrambled eggs with ½ cup of unsweetened applesauce.
- 1 cup of oatmeal with a peeled peach.
- Smoothie made with 1 cup of low-fat Greek yogurt, 1 cup of unsweetened almond milk, 1 cup of frozen peaches, and ½ banana.
Nutrition And Ulcerative Colitis
There is no special diet for people with Ulcerative Colitis . This means that research has not shown any particular foods to either help or worsen disease activity.
However, ensuring good nutrition is an important part of managing UC.
People with UC are at risk for developing malnutrition and nutrient deficiencies. Poor nutrition makes it more difficult for your body to heal and fight infection. Malnutrition may also cause you to feel tired.
There are several reasons why people with UC may be at risk for poor nutrition, including:
|
So, people with UC should follow a balanced diet and be sure to get enough calories, protein, vitamins, minerals, and fluid. No specific foods must be avoided, but some people may notice that certain foods cause discomfort. If this is true for you, avoid these foods. Nutrition needs vary from person to person, so it is best to meet with a Registered Dietitian who can help you individualize your diet.
Calories and Protein
Vitamins and minerals
Low Fiber/Low Residue: Is it necessary?
What about the special diet I read about?
Special Situations
Lactose intolerance
Strictures, partial obstruction, or narrowed areas of bowel
Additional Resources
Don’t Miss: Is Soy Sauce Ok For Ulcerative Colitis
Ulcerative Colitis: This Is Why You’re Here Right
- Why did you get Ulcerative Colitis? The short answer is that scientists still don’t know. Genetics are a major risk factor, but some people without a family history develop the condition
- Ulcerative Colitis is caused by an autoimmune response from your body
- Your symptoms may include:
- GI: loose and urgent bowel movements, bloody stool, abdominal pain and cramps, persistent diarrhea
- Non-GI: appetite loss, weight loss, nausea, low energy, anemia
- There are flares and periods of remission throughout disease course UC is different from other types of colitis because tiny ulcers form, causing long term inflammation
What Should I Eat During A Flare
Youre feeling good, taking your medication, eating generally anti-inflammatory foods, and all of suddenbamyou start to feel those telltale flare symptoms. What should you do now? Adjusting your diet may help you over the hump.
If you are in a flare, you may want to eat foods that are gentle on your digestive tract, while the inflammation calms down, says Dr. Singh.
Practically speaking, you can do this in a few ways. For instance, Freuman works with her clients to tailor a well-rounded diet to avoid their specific triggers and address their needs. This may include:
Its best to work with a professional when making changes to your diet, as they can ensure that you are getting the nutrients that you need, help you assess your trigger foods, and address any underlying history of disordered eating or dietary changes that could trigger those behaviors.
Read Also: Signs Of Having An Ulcer
What Foods Should You Eat With Ulcerative Colitis
If you have Ulcerative Colitis, very minor changes to what you eat can make a BIG difference in your symptoms. Consider keeping food logs or adjusting foods that trigger your symptoms. You may also want to work with your doctor or dietitian to work through an elimination diet. Generally, you should try to:
In terms of specific food recommendations, go with these:
| Food Type |
|---|
What You Should Know:
- Inflammatory Bowel Disease is a term for two specific and separate diseases: Crohns Disease and Ulcerative Colitis. Crohn’s disease is a disease of unknown cause that can involve any portion of the digestive tract. Ulcerative colitis is an inflammatory disease of the colon or large intestine, which is often accompanied by bloody diarrhea.
- Sometimes surgery and/or medications are needed to treat these diseases.
- Inflammation in the colon can cause the colon to empty frequently, causing diarrhea.
- Stress or certain foods can exacerbate symptoms.
- There is no need to avoid foods unless they worsen your symptoms. It is best to restrict as few foods as possible to increase the chances that you are getting a balanced, nutritious diet.
- Many people with IBD are at increased risk for nutrient deficiencies and may require a vitamin/mineral supplement.
Read Also: Stomach Ulcer Blood In Stool
Foods To Avoid With Ulcerative Colitis
- Added sugars and hyper-processed foods
Our North American love affair with low fibre, high sugar and high fat hyper-processed food is associated with our risk of ulcerative colitis. It is this type of eating that is thought to drive gut dysbiosis or the overgrowth of more pro-inflammatory gut bacteria that can harm gut barrier integrity leading to leaky gut and inflammation. In laboratory studies, this type of diet can decrease the number or acetate and butyrate producing bacteria and increase the risk of colitis.
Another issue with hyper-processed foods is that they contain emulsifiers like xanthan gum and carrageenan which may alter gut barrier integrity. While their true impact on gut health is still hotly debated, in one double-blinded trial, people with ulcerative colitis on a carrageenan free diet had lower relapse rates than those given two capsules of carrageenan. For me, this would not be the first place I look when adjusting someones diet instead, it would be a refinement only after taking more global steps towards a more whole foods, plant-based approach.
- Meat, particularly red meat
If you arent a huge fan of red meat, ditch it entirely. If you truly love red meat, try to limit yourself to one 3-4 ounce portion every week or two, no more.
- Dairy
Dairy could be impacting symptoms for a few reasons:
- Omega 6-rich cooking oils like soy, corn and safflower oils
Eating When You Are In Remission
While theres no cure for UC, you may experience periods of remission. During this time, youll be symptom-free and your UC wont interfere with your daily life.
Theres no definitive way to avoid flare-ups forever, but you can prolong your remission periods by maintaining a diverse and nutrient-rich diet that does not include trigger foods.
To stay symptom-free, it may be helpful to follow one of the diets that other individuals with UC find successful, as well as introduce new foods slowly and stay hydrated.
However, its important to consult with your doctor or dietician before making any changes to your diet.
Some foods that may help keep you feeling good and hydrated during remission
Recommended Reading: Pressure Ulcers Are Most Likely To Develop
Dietary Advice For Ulcerative Colitis
Please note, this page is printable by selecting the normal print options on your computer.
What is Ulcerative Colitis?
Ulcerative Colitis is a form of Inflammatory Bowel Disease . IBD is a term used to cover a number of inflammatory conditions of the gastrointestinal tract. UC causes inflammation in the large bowel and can affect the rectum, part of, or the entire colon. If you have UC this diet sheet may help you.
Can diet help?
Diet is not a cause of UC however diet can help to relieve symptoms such as diarrhoea during a flare up and maintain good health including healthy bones. You may find as time goes by you begin to notice that certain foods aggravate your symptoms of UC and so they are best avoided. However, do not remove whole food groups as this could mean you lose some vital nutrients. The main food groups are demonstrated below in the Eatwell Guide.
What foods are beneficial for UC during a flare up?
Soluble FibreDietary fibre can be categorised into two forms, soluble and insoluble. Soluble fibre is partially digested in the large intestine to form a glue like substance, which helps to produce soft/formed stools, without causing inflammation. Examples of foods rich in soluble fibre are:
- Oats e.g. Porridge oats/Ready Brek ®, oatcakes
- The body of fruits and vegetables e.g. peeled apples and pears, tinned fruit, peeled root vegetables such as carrots, parsnips, turnip
What foods may worsen UC during a flare up?
Dairy foods
Spicy foods and fatty foods