Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
Living With Ulcerative Colitis
Ulcerative colitis, a disease that causes inflammation and sores in the digestive tract, affects everyone in a different way. About 10% of people get better after one attack, but it’s more likely that you’ll have flares that come and go throughout your life.
You may go weeks or years without any symptoms. That’s called remission. The longer you go without a flare, the better your overall health will be.
Your doctor will likely give you medicine to control inflammation and other symptoms.
If you don’t feel like your UC is under control, talk to your doctor. They may want to change your medicine dose or switch you to a different drug. If that doesn’t work, you may need surgery.
What Other Conditions Are Related To Ulcerative Colitis
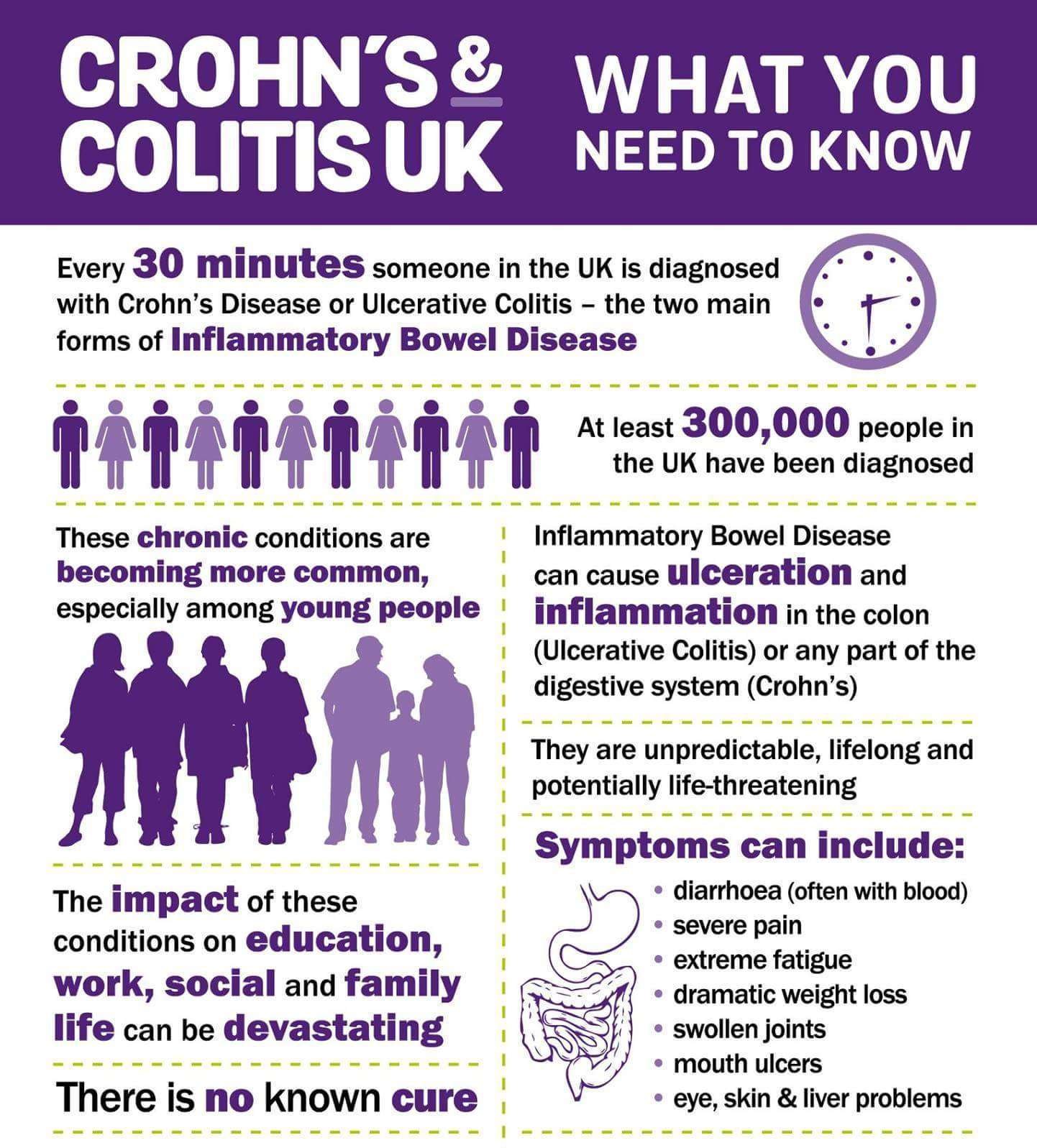
Ulcerative colitis is a type of inflammatory bowel disease , but it’s not the same as irritable bowel syndrome .
Although the disorders share some of the same symptoms, such as abdominal pain and diarrhea, inflammation and ulcers do not occur with IBS.
Another disease often mentioned alongside ulcerative colitis is Crohns disease. Ulcerative colitis and Crohns are different types of IBDs that affect the digestive tract in different ways.
There are some common symptoms between the two conditions, but the overall pattern of symptoms tends to be different for each.
While diarrhea and rectal bleeding are more common in ulcerative colitis, Crohns disease more often causes severe abdominal pain, nausea, weight loss, and vomiting.
Ulcerative colitis is limited to the lining of the large intestine , whereas Crohns disease can affect the entire digestive tract from your mouth to your anus and isnt limited to the inner part of the intestines.
Learn More About the Differences Between UC and Crohns
Don’t Miss: How Can Ulcers Be Treated
What Should You Eat When You Have Ulcerative Colitis
When it comes to food, theres no known dietary cause of ulcerative colitis, but different foods may aggravate or help limit symptoms of the disease.
Youre more likely to need to change your diet during periods of active disease , when eating soft, bland foods can help limit symptoms like cramping and diarrhea.
During flares, you may also want to avoid or limit high-fiber and high-fat foods, as well as caffeine, alcohol, dairy products, and spicy foods.
If youre losing nutrients and water in your diet due to diarrhea, you may need to focus on increasing your fluid intake and getting enough calories, protein, vitamins, and minerals from foods or supplements.
Learn More About Diet and Ulcerative Colitis
Figuring Out Which Foods Trigger Flare
As the NIDDK explains, although ulcerative colitis isnt caused by diet or nutrition, certain foods can trigger the symptoms or make them worse in some people. The tricky part is figuring out which ones.
Common ulcerative colitis triggers include dairy, high-fiber foods like fruit, vegetables, and whole grains, spicy foods, alcohol, and caffeine, according to the Mayo Clinic. That said, its really individual. Sam has always loved food and says that when it comes to what she can eat now, I have not figured that aspect out. And its not for lack of trying. I feel like I’ve done everything! she tells SELF, explaining that she tries to avoid various food groups like dairy that can trigger symptoms. It doesn’t mean I don’t ever eat them, but I try to avoid them, she says. I’m definitely still experimenting.
Stacey Bader Curry, 48, was diagnosed with ulcerative colitis in March 2020 and is concerned about giving up foods she loves, as well as alcohol and coffee. I’m trying to focus on what I can eat and not what I can’t eat, she says.
To figure out whether certain foods might be triggering your symptoms, the NIDDK recommends keeping a food diary where you record everything you eat and any flare-ups to help you work out what your dietary triggers could be.
Don’t Miss: Causes Of Ulcers In Horses
Warnings About Aloe Vera Consumption
Those with ulcerative colitis should be cautious about consuming aloe vera juice, commonly available in stores. Aloe vera has a laxative effect and may be problematic for those already experiencing diarrhea.
Aloe vera products are not regulated by the Food and Drug Administration . Given this, it can be hard to tell if products claiming to contain aloe vera actually do contain aloe vera, or instead contain aloe latex, which has strong laxative properties.
- Curcumin: Curcumin is an active ingredient found in the spice turmeric. It is believed to contain anti-inflammatory properties and, because of this, may be beneficial for those living with ulcerative colitis. A 2020 review examined the results of seven studies involving 380 patients with ulcerative colitis. They found that when curcumin therapy was combined with mesalamine , a medication prescribed in the treatment of ulcerative colitis, that patients were three times more likely to experience a clinical response. The same study found that those on curcumin therapy also experienced minimal side effects.
How Does Blood In The Stools Appear
According to the Canadian Institute of Intestinal Research, most people with UC experience varying levels of hematochezia, which refers to blood in the stools. The blood will usually be clearly visible in the stool â which has a semi-solid consistency â or on the surface. The blood color can range from bright red to maroon, with or without blood clots. This symptom often accompanies lower abdominal pain and the urgent need to defecate.
Blood from the rectum and large intestine is usually bright red. If blood is a darker color, it may be coming from higher up the gastrointestinal tract.
People with UC may have slow, steady bleeding when they do not have a bowel movement. They may also experience bloody diarrhea and constipation.
Some individuals with severe UC may notice blood in their stools more than 10 times a day.
People with UC will also usually have mucus in the stools but may not be able to see it. The mucus helps protect the inner lining of the intestines, as well as helping with bowel movements.
According to the Crohnâs and Colitis Foundation, people need immediate medical attention if they experience rectal bleeding with blood clots in stools.
Read Also: What Are Some Symptoms Of An Ulcer
Elective Colorectal Cancer Surgery
Patients with Crohns disease and ulcerative colitis have a higher risk for colorectal cancer than the general population, so elective surgery may be recommended to eliminate that risk.
Colorectal cancer risk factors
-
The risk of CRC increases after living with IBD for 8 to 10 years
-
The risk increases the longer a person lives with IBD
-
The greatest risk is for people with IBD affecting their colon
-
Patients who have a family history of primary sclerosing cholangitis are also at higher risk of developing colorectal cancer
In most cases, colorectal cancer starts as a polyp, or a small lump growing from the wall of the intestine. Polyps typically start out benign but become cancerous over time. But in patients with IBD, abnormal and potentially precancerous tissue, called dysplasia, may lay flat against the wall of the intestine and can even be found in areas of the intestinal wall that appear normal during a colonoscopy.
How Is Ulcerative Colitis Diagnosed
To diagnose ulcerative colitis in children, teenagers and adults, your healthcare provider has to rule out other illnesses. After a physical exam, your provider may order:
- Blood tests: Your blood can show signs of infection or anemia. Anemia is a low level of iron in your blood. It can mean you have bleeding in the colon or rectum.
- Stool samples: Signs of infection, parasites , and inflammation can show up in your poop.
- Imaging tests: Your healthcare provider may need a picture of your colon and rectum. You may have tests including a magnetic resonance imaging scan or computed tomography scan.
- Endoscopic tests: An endoscope is a thin, flexible tube with a tiny camera. Specialized doctors can slide the endoscope in through the anus to check the health of the rectum and colon. Common endoscopic tests include colonoscopy and sigmoidoscopy.
You May Like: Surgical Management Of Ulcerative Colitis Ppt
What If I Get Sick
The main symptoms of COVID-19 are a fever, dry cough, and shortness of breath. It can also cause:
- Fatigue
- Loss of taste or smell
- Sore throat
- Skin rash
If you notice a change in how youâre feeling, call your doctor.
Most importantly, if you think you might have COVID-19, isolate yourself from other people. Call your doctor or follow the advice where you live to learn what to do next and how long youâll need to stay away for other people.
Free COVID testing is available in most communities. Some locations require an appointment while others are drive-up. Check with your local health department about testing availability.
The Difference Between Ulcerative Colitis And Crohn’s Disease
Crohn’s disease is also an inflammatory bowel disease . The 2 diseases affect the digestive tract differently:
- Ulcerative colitis only affects the large bowel , and inflammation is only in the surface layers of the bowel lining. It causes ulcers to form in the lining of the bowel.
- Crohn’s disease can affect any part of the digestive tract, from the mouth to the anus , but usually just the last section of the small bowel and/or the colon. Inflammation can extend into the entire thickness of the bowel wall.
Don’t Miss: Different Types Of Ulcerative Colitis
Ulcerative Colitis Questions To Ask Your Doctor
Whether youâre worried your symptoms are UC, or you already have the condition and want more information, here are questions to ask your doctor:
- Are my symptoms a sign of ulcerative colitis or another condition?
- Are there different kinds of UC? Do they have different symptoms?
- What tests will I need?
- If I have ulcerative colitis, what will my treatment plan be?
- Will changing my diet or lifestyle help ease my symptoms?
- How serious is my ulcerative colitis?
- If I take medication for ulcerative colitis, will there be side effects?
- Should I take nutritional supplements like probiotics?
- How often will I need to come in for checkups?
- What should I do if my symptoms suddenly get worse?
- How do I know if my ulcerative colitis is getting worse?
- How do I know if I should change my ulcerative colitis medication?
- Should I consider surgery? What does surgery involve?
- What is my risk of getting colon cancer?
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
Also Check: How To Stop An Ulcerative Colitis Flare
True Stories: Living With Ulcerative Colitis
Ulcerative colitis affects about 900,000 people in the United States. In any single year, about 20 percent of these people have moderate disease activity and 1 to 2 percent have severe disease activity, according to the Crohns and Colitis Foundation of America.
Its an unpredictable disease. Symptoms tend to come and go, and sometimes they progress over time. Some patients go for years without symptoms, while others experience frequent flare-ups. Symptoms vary depending on the extent of the inflammation, as well. Because of this, its important for people with UC to keep track of how it affects them on an ongoing basis.
Here are the stories of four peoples experiences with UC.
years ago.
How do you manage your symptoms?
My first treatment was with suppositories, which I found extremely uncomfortable, hard to put in, and hard to hold. For the next year and a half or so I was treated with rounds of prednisone and mesalamine . This was awful. I had terrible ups and downs with prednisone, and every time I started to feel better I would feel sick again. I finally switched doctors to Dr. Picha Moolsintong in St. Louis, who actually listened to me and treated my case and not just my disease. I am still on azathioprine and escitalopram , which have been working very well.
What other treatments have worked for you?
What advice would you give to other people with UC?
How long ago were you diagnosed?
How difficult has it been to live with UC?
What helped you?
Types Of Ulcerative Colitis
The type of ulcerative colitis you have depends on where it is in your body:
- Ulcerative proctitis is usually the mildest form. Itâs only in the rectum, the part of your colon closest to your anus. Rectal bleeding may be the only sign of the disease.
- Proctosigmoiditis happens in your rectum and the lower end of your colon . Youâll have bloody diarrhea, belly cramps, and pain. Youâll have the urge to poop, but you wonât be able to.
- Left-sided colitis causes cramps on that side of your belly. Youâll also have bloody diarrhea, and you might lose weight without trying. Youâll have inflammation from your rectum up through the left side of your colon.
- Pancolitis often affects your entire colon. It can cause severe bouts of bloody diarrhea, belly cramps, pain, fatigue, and major weight loss.
- Acute severe ulcerative colitis is rare. It affects your entire colon and causes severe pain, heavy diarrhea, bleeding, and fever.
Don’t Miss: Ulcerated Nodular Basal Cell Carcinoma
How Many People Have Ulcerative Colitis
Get the free app for Members
Get the free app for Doctors
Should I Stop Taking My Medicine
The short answer is, âNo.â If you stop taking your medicine because youâre worried about your immune system, your symptoms may flare. Some medicines take months to leave your system anyway. So stopping them now wouldnât change your risk of COVID-19 now. And you definitely donât want to have to go to a hospital now because of a flare.
It may be a good idea to avoid steroids if you can. But you shouldnât stop taking them suddenly. As a general rule, donât change any of your medications without first talking to your doctor.
Don’t Miss: Is Ulcerative Colitis Considered An Autoimmune Disease
Enhancing Healthcare Team Outcomes
Ulcerative colitis is a systemic disorder with no cure. The disorder has numerous extraintestinal involvement in addition to the colon. Thus, it is best managed by an interprofessional team. All patients with the disorder need lifelong monitoring. Because of the risk of colorectal cancer, surveillance colonoscopy should occur every 1-2 years. Further, since patients are often treated with biological agents, they need to undergo screening for melanoma and nonmelanoma skin cancer.
The pharmacists should assist the team by educating the patient on the importance of medication compliance to avoid relapse. The nurse should encourage regular vaccinations, hand washing, and cancer screening. A dietary consult should be obtained to educate the patient on foods to eat and what not to eat, especially if they have a stoma. In addition, a stoma nurse should be involved in the teaching of stoma care.
An infectious disease nurse should monitor the patient in the outpatient setting to ensure that they are not immunocompromised. Social workers should be involved to ensure that the patient has ample support and finances so that the treatments are not missed. Patients with risk factors for osteoporosis need screening for bone mineral density periodically. Patients should be encouraged to undergo annual vaccination against influenza and pneumococcus. Finally, many patients with ulcerative colitis develop depression and anxiety and should be referred to a mental health counselor.
Outcomes
More Than 200 Genes Identified
While no single underlying cause for IBD has been identified, genetics certainly play a role.
Jeffrey C. Barrett, Ph.D. who is a senior group leader from the Wellcome Trust Sanger Institute in Cambridge in the United Kingdom explains in an article published in the Journal of Autoimmunity that identical twins had nearly 10 times the rate of Crohns disease and nearly four times the rate of ulcerative colitis as non-identical twins.
This support the importance of genetics in IBD risk, he says. But it is not straightforward.
More than variations in the DNA code have now been linked to IBD, and this number is continuing to rise as molecular biology technology is becoming ever more sophisticated.
What are all these genetic data telling us about IBD?
Certain biological processes or pathways keep on cropping up. These include genes involved in the innate immune response including some genes responsible for keeping the lining of our gut intact as well as those involved in the activation and regulation of the adaptive immune response.
Perhaps these findings come as no surprise the classic hallmark of IBD is a dysregulated immune response. However, without detailed knowledge of how these pathways are disrupted, treatments will mostly focus on symptoms, rather than the underlying causes of the condition.
Yet genetics can only explain a proportion of the risk associated with developing IBD.
article in The Lancet thathighlights how IBD rates have evolved across the globe.
Also Check: Symptoms Of Ulcer In Female