Types Of Steroids For Uc
There are several types of steroids for UC. Some are oral and some are rectal. Below, youll find more detail on some of the more commonly prescribed steroids for UC:
- Prednisone . This is a pill taken once daily, typically in the morning. Prednisone has been used for over 60 years and may also be prescribed at a high dose intravenously .
- Budesonide . This steroid, taken in pill form, is quickly metabolized by the liver, which may reduce side effects.
- Budesonide MMX . These are extended relief tablets for active and mild to moderate UC.
- Rectal hydrocortisone. This suppository may be recommended to treat UC or swelling.
Because there are several types of steroids, and everyone will have a different reaction to them, its important to have a good relationship with your doctor during your UC treatment.
Long before having you start steroids, your doctor will be able to plan out tapering regimens that will work best for you and escalate or de-escalate your treatment depending on your bodys needs.
What Are Corticosteroids
Corticosteroids are anti-inflammatories, meaning they decrease levels of inflammation in the body. They are man-made versions of the hormone cortisol which is created by the human body in the adrenal glands . Taking corticosteroids causes the body to slow down production of, or stop making, cortisol. The body then receives the cortisol it needs from the corticosteroids.
They are a fast-acting medication and many people who take them to help with moderate to severe flare ups of their IBD notice an improvement in their symptoms within days.
As well as being an anti-inflammatory medication, they also work to suppress the immune system. This may cause you to become more susceptible to catching infections.
They are not used in maintenance therapy for IBD . Due to the potential side effects of corticosteroids they are usually only prescribed for short periods to help bring acute IBD flares under control.
Corticosteroids are used to treat a huge range of conditions as well as IBD. These include asthma, eczema, chronic obstructive pulmonary disease , lupus and multiple sclerosis.
Could My Symptoms Be Ibs
Irritable Bowel Syndrome is a different condition from IBD, although some of the symptoms are similar. Like Crohnâs and Colitis, IBS can cause abdominal pain, bloating and bouts of diarrhoea or constipation. However, it does not cause the type of inflammation typical of Colitis, and there is no blood loss with IBS.
Some people with Colitis may develop IBS-like symptoms, for example experiencing diarrhoea even when their Colitis is inactive. These symptoms may need slightly different treatment from their usual IBD symptoms. IBS is more common in people with IBD than in the general population.
If you develop diarrhoea with bleeding and abdominal pain, your doctor may suspect you have Colitis, particularly if you are a young adult or have a family history of Crohnâs or Colitis. You will need tests and physical examinations to confirm a diagnosis. See Tests and Investigations for IBD.
You may need to have tests repeated from time to time to check on your condition and how your treatment is working.
Some drug treatments may also require a series of blood tests and, occasionally, x-rays or scans to check for any potential side effects. Your specialist will avoid giving you any unnecessary tests or investigations.
You may need more regular colonoscopies when you have had Ulcerative Colitis for a long time to check for any signs of cancer.
Donât Miss: How To Check A Horse For Ulcers
You May Like: How To Fix Mouth Ulcers
Selective Glucocorticoid Receptor Agonists
Identification and development of SEGRAs is of particular interest because their therapeutic potential is uncertain . SEGRAs are also defined as dissociated GCs because they could allow anti-inflammatory activities and the avoidance of metabolic effects. SEGRAs allow the mediation of only repressive effects on various controlled target genes from the GR, and not those of gene activation, because they work by operating through one of two main pathways: transactivation or transrepression . The concept that the activating action is responsible for the metabolic effects, whereas immunosuppressive mechanisms are dependent upon the repressive effects, is controversial. Some SEGRA compounds have been shown to have anti-inflammatory properties with reduced collateral effects, such as Compound A , or ZK216348 N–4–2-hydroxy-2–4-methylpentanamide . Therefore, their efficacy in vivo for treatment of inflammatory diseases, such as colitis, asthma, and rheumatoid arthritis, is being evaluated .
Medical Management Of Ulcerative Colitis
Therapeutic decisions depend on disease activity and extent. Disease activity is best evaluated objectively using a clinical activity index . Patients with severe disease require hospital admission, whereas those with mild/moderate disease can generally be managed as outpatients.
Disease extent can broadly be divided into distal and more extensive disease. Topical management is appropriate for some patients with active disease. This is usually the case for those with proctitis and often the case if the disease extends into the sigmoid. For those with more extensive disease, oral or parenteral therapy are the mainstays of treatment, although some of these patients may get additional benefit from topical therapy.
Read Also: What Can You Eat With Ulcerative Colitis
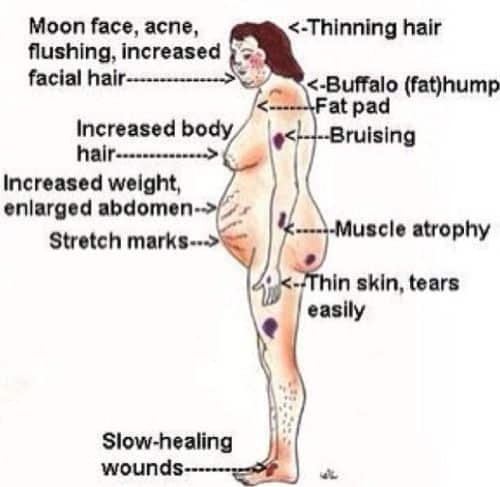
Side Effects Of Steroids For Ulcerative Colitis
QMy nephew, who has recently been hospitalized for treatment of ulcerative colitis, is coming to.
usually are prescribed intravenous steroid treatment and then are carefully observed for any of t.
Taking steroids for ulcerative colitis can have several negative side effects, but the form of administration greatly affects the chances of these side effects occurring. Corticosteroids can be taken orally or rectally, with oral steroids being the most likely to cause adverse side effects.
Complications associated with ulcerative colitis include an increased risk of colorectal cancer, secondary osteoporosis, venous thromboembolism and toxic.
This information sheet is designed to answer common questions you may have if you have been given steroids to treat your Crohns Disease or Ulcerative Colitis , the two main forms of Inflammatory Bowel Disease .
Steroids corticosteroids.
arthritis, asthma, ulcerative colitis, temporal arteritis, psoriasis and even bad cases of poison ivy. But as with any powerful remedy, corticosteroids come with a down.
Side effects are common with this type of medication. Below is a partial list of those most commonly experience many of these will go away after steroid use has.
Prednisone is used to treat allergic disorders, ulcerative colitis, psoriasis and arthritis. Learn about side effects, interactions and indications.
Medicines That Interact With Them
Corticosteroids can interact with other medicines, and the effects of either medicine can be altered as a result.
There is less chance of this happening with steroid injections or sprays, although it can occasionally happen if they’re used at high doses and for a long time.
Some of the more common interactions are listed below, but this is not a complete list. If you want to check your medicines are safe to take with corticosteroids, ask your GP or pharmacist, or read the patient information leaflet that comes with your medicine.
Also Check: Patient Education On Pressure Ulcer Prevention
Multicentre Uk Audit Of Steroid Use
Our group conducted a prospective multicentre audit of corticosteroid use in previous 12 months among 1176 patients with IBD in 2016. Steroid dependency or excess were defined as per BSG and ECCO guidelines. Corticosteroid exposure was noted in 30% of patients with 14.9% meeting criteria for steroid dependency/excess and 49.1% patients were judged to have inappropriate steroid dependency. The decision to commence steroids was made in primary care in 17% patients 91.3% of these cases classed as avoidable steroid excess vs. 42% of cases initiated in secondary care. In CD, an established IBD multidisciplinary team was protective , whereas treatment with 5-ASA was associated with dependency or excess . Treatment at a centre with dedicated IBD clinics was protective in UC .
In a follow-up study with 2385 patients across 19 centres, we noted a 14.8% rate of steroid excess or dependency, 50.7% of which was deemed avoidable. Seven centres that had introduced quality improvement achieved reduction in steroid exposure and excess , an effect that remained true on multivariate analysis. Treatment at a centre with an IBD MDT was associated with a lower risk of steroid excess/dependency and in UC use of a thiopurine without a biologic for more than 3 months was independently associated with an increased risk of steroid excess.
How Long Should A Person Take Steroids
Steroids are not a long-term treatment option, due to possible side effects.
Doctors often prescribe steroids for people with UC on a short-term basis to help bring a flare-up under control and help the UC go into remission. A person may also take steroids on a short-term basis while waiting for other treatments to take effect.
Healthcare professionals often prescribe steroids for a period of 8 weeks, with the dose gradually reducing during this time. It is important a person completes the full course and does not stop taking steroids suddenly, even if symptoms improve.
Due to the possibility of numerous side effects, doctors often choose other medications before prescribing steroids for UC.
A person may try topical or oral 5-ASAs before trying steroids.
If a person and their doctor decide to reduce or stop taking steroids and symptoms continue, the individual may take immunosuppressants such as azathioprine or mercaptopurine along with steroids.
In cases of severe UC that does not improve with steroids or immunosuppressants, biological treatments like infliximab or adalimumab may help.
Recommended Reading: Signs You Have A Stomach Ulcer
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
Crohns & Colitis Uk Local Networks
Our Local Networks of volunteers across the UK organise events and provide opportunities to get to know other people in an informal setting, as well as to get involved with educational, awareness-raising and fundraising activities. You may find just being with other people and realising that you are not alone can be reassuring. Families and relatives may also find it useful to meet other people with Crohn’s or Colitis. All events are open to members of Crohns & Colitis UK.
Recommended Reading: Diet For People With Ulcers
Corticosteroids In The Management Of Inflammatory Bowel Disease
1 Department of Gastroenterology, Section of Inflammatory Bowel Diseases, The Northern Care Alliance NHS Foundation Trust, Manchester, United Kingdom
2 Department of Gastroenterology, Leeds Teaching Hospital NHS Trust, Leeds, United Kingdom
3 Manchester Academic Health Sciences, Faculty of Biology, Medicine & Health, University of Manchester, United Kingdom
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.
Don’t Miss: Is Ulcerative Colitis And Colitis The Same Thing
What Are The Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms often get worse over time. In the beginning, you may notice:
- Diarrhea or urgent bowel movements.
- Abdominal cramping.
- Loss of fluids and nutrients.
Symptoms are similar in pediatric ulcerative colitis and may also include delayed or poor growth. Some ulcerative colitis symptoms in children can mimic other conditions, so it is important to report all symptoms to your pediatrician.
Read Also: Ulcerative Colitis And Apple Cider Vinegar
Does Apriso Cause Any Long
Its possible for some side effects of Apriso to be long term. These are side effects that either continue for a long time or start after youve taken Apriso for a long time.
- liver failure, in people who already have liver problems
For details about kidney problems and Apriso, see Side effects explained below. And for more information about liver failure, see Warnings for Apriso below.
If you have questions about long-term side effects of Apriso, talk with your doctor or pharmacist.
Read Also: Can Ulcers Cause Bloody Stool
Oral Vs Rectal Treatments
Most physicians prescribe ulcerative colitis patients oral versions of 5-ASAs or corticosteroids, since this is a patient-preferred delivery method of medication. However, even if they have a specially designed release mechanism, they might not reach and treat the area where the disease is most active.
For example, when you apply sunscreen to your skin, you need to make sure that you cover every exposed part to protect it from the sun. Similarly, when applying these treatments to your rectum and lower colon, you need to make sure that the product covers all of the inflamed areas.
Oral tablets might not be the optimal way to reach the end of the colon, where stool and the fact that ulcerative colitis patients have diarrhea, might interfere with its effectiveness. Unfortunately, this is also the area in the colon where a flare usually starts. The best way to reach this particular area is by inserting the drug directly into the rectum.
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
Read Also: How Do You Check For A Stomach Ulcer
What Are The Types Of Systemic Steroids
There are many types of steroids your doctor can prescribe for your UC, and different ways to take them. The most common is orally, or by mouth.
Options you take by mouth:
- Prednisone is one of the most common corticosteroid choices. You take it as a pill.
- Budesonide is a modified steroid your body absorbs through the small intestine and colon. Your liver processes it much faster than prednisone. That means your risk of side effects is lower. This drug is a capsule.
- Budesonide-MMX is the same as budesonide, but it has a special coating on it. The coating keeps the medication inside the capsule until it gets to your colon. This helps more of the medication go straight to the colon. This option is best for treating inflammation in the colon only, which is what happens in ulcerative colitis.
Doctors usually recommend you take oral steroids in the morning so theyâre less likely to affect your sleep. Oral options typically improve your symptoms within 1-4 weeks. Theyâre not recommended for use longer than 8 weeks.
Your doctor may give you steroids you can take rectally. These are not systemic steroids, but they go to work right in the areas where the inflammation is for mild to moderate UC:
Most people see their symptoms start to improve after 1 or 2 weeks.
For severe flares of UC, you may need hydrocortisone delivered into a vein through an IV in the hospital. This usually relieves symptoms within 4-10 days. Your doctor will then switch you to oral steroids.
How Do I Take Budesonide For Inflammatory Bowel Disease
Your IBD team will give you detailed information on your dosage of budesonide for your inflammatory bowel disease and how often you should take it. You can also read the patient information leaflet included in every medicine packet.
Oral budesonide for crohns disease and ulcerative colitis
You will usually take budesonide tablets, capsules or granules once a day, in the morning, half an hour before breakfast.
You should swallow budesonide capsules or tablets with a glass of water, and must not chew them as this could stop them working properly. Budesonide granules can be mixed into a small amount of food to make them easier to swallow, but they must not be chewed.
Oral budesonide is usually prescribed as an eight week course of treatment, and your IBD team may ask you to reduce your dose gradually towards the end of your treatment. It is important you dont suddenly stop taking budesonide, even if you feel better, as this could make you very unwell.
Topical budesonide for UC
Budesonide enemas are usually used once a day for between four and eight weeks. Budesonide rectal foam is usually used once a day for between six and eight weeks.
Steroid treatment card
Read Also: Is Ulcerative Colitis The Same As Diverticulitis