Common Triggers Of Ulcerative Colitis Flare
The symptoms of ulcerative colitis flare-up are not pleasant and often force people to retreat socially. They fear being too far away from a washroom. How long do colitis flare-ups last? Ulcerative colitis flare-up duration can be a few days or several weeks. Sometimes, it depends on the trigger.
Here are some common triggers of the disease:
- Hormone fluctuations during pregnancy
- Caffeine
- Stress
Understanding the triggers and knowing how to stop a colitis flare-up gives those who are diagnosed with the disease the confidence to enjoy normal activities, including a full social life.
Warning Signs Of A Flare
Flares often are acute, meaning they come on suddenly. They can last from days to weeks. Between flare-ups, you may experience weeks, months, or years of remission.
Symptoms of a flare may be different depending on the severity and location of the inflammation in the colon and rectum. Nevertheless, common symptoms include:
- Abdominal pain or cramps
- Fever
What Should I Ask My Doctor On Behalf Of My Child Or Teenager
Ask your healthcare provider the following questions in addition to the ones listed above:
- What vitamins should my child take?
- Will my other children have pediatric ulcerative colitis?
- Is my child at risk for other conditions?
- Can you recommend a psychiatrist or therapist to help my child with emotional issues related to pediatric ulcerative colitis?
- Is my child growing at a normal rate?
- What can I do to help my child cope at school?
A note from Cleveland Clinic
When you have ulcerative colitis, its essential to work closely with your healthcare team.
Take your medications as prescribed, even when you dont have symptoms. Skipping medications youre supposed to take can lead to flareups and make the disease harder to control. Your best shot at managing ulcerative colitis is to follow your treatment plan and talk to your healthcare provider regularly.
Don’t Miss: What To Avoid With An Ulcer
Can A Uc Flare Last Months
A flare-up can last a few days or a few weeks and then be followed by a remission that lasts for months or even years. How long a flare-up lasts depends on factors such as: Severity of the disease Triggers such as stress, infection, diet changes etc.
Avoiding Certain Pain Relievers

According to the Crohns and Colitis Foundation , the following over-the-counter or prescription pain relievers can cause intestinal ulcers:
- nonsteroidal anti-inflammatories, or NSAIDs, such as ibuprofen
- COX-2 inhibitors, including the brands Celebrex and Vioxx
The CCF recommend that people avoid taking these drugs unless they are necessary to treat a serious health issue, such as heart disease.
You May Like: How To Cure Gastritis And Ulcers Naturally
How Long Can A Flare Up Last During Colitis
carol34824
Hi..i was on this recently about my 18 year old son who was recently told may have colitis, but only thing was he wasnt loosing weight…now he is…how long can a flare up last….im worried sick for him as he is a talk healthy lad and now this is having a horrible affect…and Im helpless as a mother…please can someone give me some advice
1 like, 19 replies
3 years ago
Yes Mama, and I hope you get this.
I went through a 2 year flare after having my baby and I stopped the symptoms by taking purely herbal remedies. This allowed me to live normally and without so much pain and discomfort.
Hyperbiotics Pro-15 Advanced 1x nightly
Vimerson Health Turmeric and Ginger 2 daily
Nutra Champs Digestive enzymes 1 with each meal
Dr Tobias Triple Strength Omega 3 2 daily
Sleep and Restore 1x daily
Health Concerns Isatis Cooling 1:3x daily
The Isatis Cooling is actually bringing me out of the flare, where as the others just helped me manage it and live normally. I have only been taking it a week, but I’ve been on the other supplements for 3 months. It’s been a life changing relief.
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
Also Check: Can Ulcerative Colitis Cause Blood In Urine
Ulcerative Colitis Flare Symptoms
Flare-ups indicate that the disease is in an active state, which means the rectum and colon are becoming more inflamed or sores are worsening or spreading. Symptoms of flare-ups include:
- Experiencing frequent or urgent bowel movements
- Diarrhea, which may include blood or pus
- Stool thats bloody
- Vomiting
- Weight loss
The pattern of UC flare-ups is unpredictable. The disease is considered active when symptoms are present, and in remission when no symptoms are present. Some people may spend years in remission, while others may have more frequent flare-ups.
How To Reduce Flare
While flare-ups often dont have a single, identifiable cause, several factors may contribute to them or make them worse, including:
- Missing your UC medications or taking the wrong dose
- Taking non-steroidal anti-inflammatory drugs or antibiotics
- Smoking
- Stress
- Certain foods
If flares occur even when a patient takes their medications as prescribed, it may be a sign that a change in medication type, dosage or frequency is needed.
Read Also: Best Way To Treat Mouth Ulcers
Comparison Of Symptoms Reported In Focus Groups To Symptoms From Pooled Disease Activity Indices
The lists were directly compared to determine which symptoms were present in both the focus group list and in the common indices list which symptoms were only present in the indices and which symptoms were reported by patients to be important, but were not measured by any of the common disease activity indices.
When To Seek Medical Advice
You should see your GP as soon as possible if you have symptoms of ulcerative colitis and you haven’t been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms. If necessary, they can refer you to hospital for further tests.
Read more about diagnosing ulcerative colitis.
If you’ve been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact your GP or care team for advice. You may need to be admitted to hospital.
If you can’t contact your GP or care team, call NHS 24 111 service or contact your local out-of-hours service.
Also Check: How To Cure Ulcerative Proctitis
How Long Do Flares Last
Flares occur at different times and may last for days or weeks. They can happen anywhere from weeks to years apart, depending on the person and the effectiveness of treatment.
Your doctor will work with you to treat your flare and help return your UC to a more manageable state.
The Crohns & Colitis Foundation recommends waiting to become pregnant until UC has been in remission for at least 3 months.
If you conceive during a flare-up, you may have more symptoms during pregnancy.
Youre likely to have a healthy pregnancy if you have UC, but youll still have a higher chance of complications than someone without the condition. Particularly if your UC is active, you may have a greater risk for:
- miscarriage
In general, UC medications can be taken during pregnancy.
Talk with your doctor about any possible changes to your medications while pregnant.
Ideally, having a conversation with your doctor prior to getting pregnant can allow them to prepare a UC treatment plan in advance that can be revised, if and as needed, during your pregnancy.
How Is Inflammatory Bowel Disease Diagnosed
Your doctor will give you a physical exam and listen to you describe your symptoms. To help diagnose the problem your doctor may order a number of tests, including blood tests and stool samples. Your doctor may also order one or more procedures to help them view your colon. Lower GI endoscopy procedures include colonoscopy and flexible sigmoidoscopy. During these procedures, your doctor uses a narrow, flexible tube to look directly inside your large intestine. Upper GI endoscopy allows a look at your stomach and small intestine for ulcers. For this type of endoscopy, you may swallow a small camera . If not, your doctor inserts a scope into your GI tract through your mouth.
Your doctor may also order other imaging tests such as X-rays, a CT scan, or an MRI.
Recommended Reading: How Do I Know If I Have A Peptic Ulcer
Your Uc Flare Management Plan
Your doctor may help you deal with a flare by changing your medications or offering new ones. Treatment of flares can include mesalamine products and usually a steroid, such as prednisone,” says Desi.
There are also some things you can do at home to temper a flare. These include:
During an ulcerative colitis flare, its recommended that you schedule regular visits to see your doctor, at least once every three months until the symptoms go away. After the flare has subsided, physicians recommend one or two checkups a year to manage the disease.
When an ulcerative colitis flare strikes, you have options for getting your life back on track. Its important to learn what you can about maintaining your health and work with your doctor to find the best ways to safely control UC. And remember to always let your doctor know when new or persistent symptoms arise.
What To Look For
The key is to pay attention to your specific symptoms. The more you’re aware of them, the better able you are to spot changes.
And there are lots of ways your symptoms can change. You might get new ones. Or the ones you have may get worse, last longer, or come on more often.
Usually, a flare-up brings at least:
- An urgent need to poop
- Blood or mucus in your stool
- Cramps in your lower belly
If it spreads to more areas of the colon, everything gets more intense. You have more diarrhea. Cramps get more severe. You have more mucus, pus, and blood in your stool. Pain in your belly gets worse and more widespread, especially up the left side. It can also affect your desire to eat and cause you to lose weight.
And some of those symptoms may just be signs of a stronger flare-up. You’ll need to see your doctor to find out for sure. Read more on ulcerative colitis symptoms to look for.
You May Like: What Causes Mouth Ulcers On Gums
How Is Ulcerative Colitis Handled
Treatment for UC is determined by the severity of the illness and sometimes includes each medicines and life-style modifications.
Medications
Most folks require a mix of medicines to suppress and/or modulate the immune system:
Surgery
If youve stopped responding to medicines or theyre simply not efficient anymore, surgical procedure is an choice. You can bear a proctocolectomy, which removes the colon and rectum, adopted by reconstructive surgical procedure.
Lifestyle and dietary modifications
Managing stress and feelings is essential to stopping and reducing flare-ups. Regular train and consuming a nutritious diet are vital as properly. Your physician could encourage you to comply with a eating regimen thats low in fats and has average quantities of soluble fiber and nutritional vitamins.
How To Prevent Ulcerative Colitis Flare
What are actionable steps you can take to make your symptom-free stretches last as long as possible? and stress management are probably the two biggest things as far as prevention goes, says Cohen. Parsley Health providers and health coaches often work with members who have ulcerative colitis to find a diet that helps them minimize flares and a stress management routine. Below, well dive into some specific ways to optimize your diet with natural remedies and make adjustments to your lifestyle while living with ulcerative colitis.
Recommended Reading: Can You Drink Coffee With Ulcerative Colitis
How I Got My Ulcerative Colitis Under Control
Leigh Stein, 33, was diagnosed with ulcerative colitis when she was 23 years old. The diagnosis was overwhelming and couldn’t have come at a worse time. Feeling sick and weighed down with graduate school finals, Stein, who lives in Pittsburgh, eventually landed in the hospital. Slowly she found the right medication and lifestyle changes to get the disease under control. Back on her feet and in remission, she now gives back, volunteering for the Crohn’s and Colitis Foundation of America . For Stein, reaching out to others is healthy and healing, as is running half-marathons and taking part in other fundraisers for ulcerative colitis research.
I was diagnosed with ulcerative colitis in 1999. I was in graduate school when I began feeling sick. I was losing weight, and all of a sudden food did not agree with me. I was constantly running to the bathroomsometimes 20 to 25 times a day.
I knew I needed help so I went to see a gastroenterologist. When my gastroenterologist figured out what was going on, he wanted to admit me to the hospital as soon as possible. I explained that I wanted to finish my last semester of graduate school and that finals were less than one week away. I struggled through finals week and as soon as I finished my last one, I was admitted to the hospital the next day. I dont think I realized how sick I was.
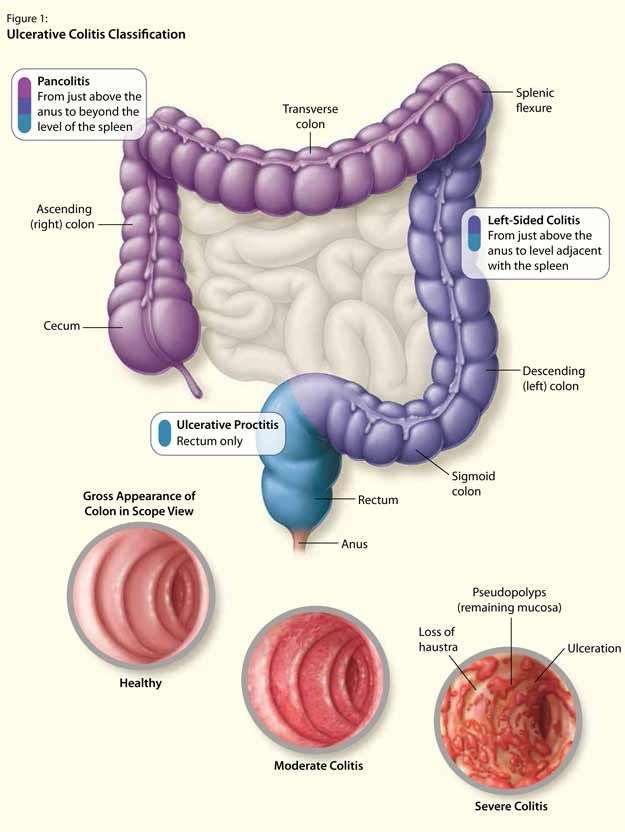
How Is Ulcerative Colitis Labeled
UC is classed as delicate, average or extreme:
- Mild: Rectal bleeding and fewer than 4 bowel actions per day
- Moderate: Rectal bleeding with greater than 4 bowel actions per day
- Severe: Rectal bleeding with greater than 4 bowel actions per day and systemic sickness with protein loss
QUESTION
Ulcerative colitis impacts the colon. The colon can be known as theSee Answer
Read Also: How Do You Know If You Have Ulcerative Colitis
How Does Pediatric Ulcerative Colitis Affect My Childs Mental/emotional Health
Like many conditions, ulcerative colitis can have a negative psychological effect, especially on children. They can experience physical, emotional, social and family problems. Because of the medications and/or general stress from the situation, your child may experience:
- Mood swings.
- Worry about appearance and physical stamina.
- Vulnerability because their body doesnt function normally.
- Poor concentration.
- Misunderstandings with friends and family.
Children need mutual support from all family members. Its helpful for the entire family to learn about the disease and try to be empathetic. Seek out a psychiatrist and therapist to help your child manage such challenges of their ulcerative colitis.
Limit Your Fiber Intake

Fiber contributes to bowel regularity and bowel health, but too much fiber can also trigger UC flare-ups.
Try to stick to foods that have no more than 2 grams of fiber per serving. Low fiber foods include:
- refined carbohydrates such as white rice, white pasta, and white bread
- fish
- some cooked fruits
- juice with no pulp
Instead of eating raw vegetables, steam, bake, or roast your vegetables. Cooking vegetables results in some fiber loss.
Recommended Reading: Side Effects Of Ulcerative Colitis
How Is Ulcerative Colitis Classified
UC is classified as mild, moderate or severe:
- Mild: Rectal bleeding and fewer than 4 bowel movements per day
- Moderate: Rectal bleeding with more than 4 bowel movements per day
- Severe: Rectal bleeding with more than 4 bowel movements per day and systemic illness with protein loss
Who Gets Ulcerative Colitis
Anyone at any age, including young children, can get ulcerative colitis. Your chance of getting it is slightly higher if you:
- Have a close relative with inflammatory bowel disease .
- Are between 15 and 30 years old, or older than 60.
- Are Jewish.
- Use frequent nonsteroidal anti-inflammatory drugs like ibuprofen .
Read Also: Stage 2 Pressure Ulcer Treatment Dressing
What Causes Ulcerative Colitis
The exact cause of ulcerative colitis is unknown. Factors that can contribute to the disease include:
- Genetics: People who have first-degree relatives with UC are at increased risk of UC.
- Immune response: Autoimmune disorders can cause your immune system to attack the cells in your body instead of defending them.
- Environmental factors:
- Diet
- Certain medications
- Consumption of milk may exacerbate the disease if you are lactose-intolerant.
Living With Inflammatory Bowel Disease
If you have inflammatory bowel disease, you are at an increased risk of colon cancer. Talk to your doctor about when to start screening for colon cancer and how often to have screening.
Crohns disease and ulcerative colitis keep coming back and their symptoms can be unpredictable. This can cause patients who have these illnesses to become depressed. If you feel depressed, talk with your family doctor. An antidepressant medicine could help you feel better.
You May Like: What Are The Symptoms Of An Ulcer In Your Stomach
Oral Vs Rectal Treatments
Most physicians prescribe ulcerative colitis patients oral versions of 5-ASAs or corticosteroids, since this is a patient-preferred delivery method of medication. However, even if they have a specially designed release mechanism, they might not reach and treat the area where the disease is most active.
For example, when you apply sunscreen to your skin, you need to make sure that you cover every exposed part to protect it from the sun. Similarly, when applying these treatments to your rectum and lower colon, you need to make sure that the product covers all of the inflamed areas.
Oral tablets might not be the optimal way to reach the end of the colon, where stool and the fact that ulcerative colitis patients have diarrhea, might interfere with its effectiveness. Unfortunately, this is also the area in the colon where a flare usually starts. The best way to reach this particular area is by inserting the drug directly into the rectum.
The medication released from a suppository will travel upward and usually reach about 15 cm inside from the anus. An enema will reach farther, about 60 cm. Those with ulcerative colitis usually insert these formulations before bedtime, and this way the medication is retained as long as possible. Stool does not typically interfere with the drug, since the bowel area is typically relatively empty right before bed.