Guidelines And Conflicts Of Interest
All members of the expert panel complied with the IDSA policy on conflicts of interest, which requires disclosure of any financial, intellectual, or other interest that might be construed as constituting an actual, potential, or apparent conflict. To provide thorough transparency, IDSA requires full disclosure of all relationships, regardless of relevancy to the guideline topic . Evaluation of such relationships as potential conflicts of interest is determined by a review process that includes assessment by the SPGC chair, the SPGC liaison to the development panel, and the BOD liaison to the SPGC, and, if necessary, the COI Task Force of the Board. This assessment of disclosed relationships for possible COI is based on the relative weight of the financial relationship and the relevance of the relationship . See Acknowledgments section for disclosures reported to IDSA.
Clostridium Difficile Causes And Risk Factors
C. diff exists all around us. It’s in the air, water, soil, and in the feces of humans and animals.
C. diff bacteria that are outside the body turn into spores that can live on surfaces for weeks or months. These spores are not “active,” but they can turn active after you swallow them and they get into your intestines. Some people have the bacteria in their intestines and never have any symptoms. But for others, the bacteria make toxins that attack the intestines.
A new strain of C. diff bacteria makes larger amounts of toxins. These types are hard to treat with medications.
C. diff bacteria spread in health care facilities, like hospitals or nursing homes, where workers are more likely to come into contact with it and then with patients or residents.
You can also become infected if you touch clothing, sheets, or other surfaces that have come in contact with feces and then touch your mouth or nose.
Older adults in health care facilities are most at risk, especially if they’re taking antibiotics. That’s because the human body contains thousands of different types of bacteria — some good, some bad. If the antibiotics kill enough healthy bacteria, the ones that cause C. diff could grow unchecked and make you sick.
The antibiotics that are most linked to a risk of C. diff infection are:
- Fluoroquinolones
You also have higher odds of getting C. diff if you have:
- A weakened immune system caused by cancer treatment or another health problem
What Is C Diff
C. diff is a contagious bacteria that can cause an infection in the colon. Anyone can become infected, although many infections typically develop in the days or weeks after taking broad-spectrum antibiotics such as:
- Cephalosporins, like Keflex or Rocephin
- Clindamycin
- Amoxicillin
In addition to killing the disease-causing bacteria responsible for infection, antibiotics can kill the helpful bacteria that the colon needs to keep a healthy biome. When good bacteria are killed,C. diff can start to grow and cause an infection.
C. diff is spread when the bacteria in feces gets on the hands of the infected individual and deposited onto other surfaces when touched. These bacteria then form spores outside the body and can live for months or even years on solid surfaces. When a person at high risk for infection touches these spores and ingests them, the spores can turn into active bacteria. These bacteria then release toxins, called toxin A and toxin B, which cause inflammation in the colon and the symptoms of C. diff.
Also Check: Ulcerative Colitis How Much Blood Is Too Much
Laboratory Test For C Difficile Infection
Positive C. difficile diagnosis was defined by a positive enzyme immunoassay test for stool C. difficile toxins A and/or B and were considered infected if they presented with concomitant symptoms of colitis . For each case with CDI, a control UC case with a negative stool C. difficile test and no prior history of CDI was matched by age and gender.
Demographic And Clinical Characteristics
Demographic characteristics included age, gender, smoking status and alcohol use. Clinical characteristics included the following. 1) Duration from UC diagnosis to CDAB testing, distribution of UC , UC severity , UC endoscopic severity , comorbid diabetes, history of colonic surgery, body mass index , complications , clinical manifestations , peripheral venous white blood cell count. 2) Potential risk factors: treatment of UC , recent hospital admission, recent antibiotic exposure, recent administration of proton pump inhibitors, recent parenteral nutrition, presence of active cytomegalovirus infection. We included not only patients with CMV colitis , but also with CMV infection. Diagnosis of CMV infection was defined as the presence of any of the following in blood: positive CMV IgM, CMV DNA by polymerase chain reaction, CMV pp65. 3) Treatment and outcome: subsequent surgery, medication for CDI, outcome and recurrence of CDI.
Don’t Miss: What Is Ulcer Pain Like
Why My Diagnosis Was Delayed: The Danger Of False Negatives
My C. diff symptoms began shortly after taking the antibiotics. I understood this only in retrospect, because at the time, I thought the C. diff symptoms were still just colitis symptoms. Only later did I understand how to tell the difference, which I describe below.
Suspecting C. diff, my doctors tested me for itbut the test came back negative. Twice. I now believe that these were almost certainly false negatives. Inaccurate results are common with C. diff tests, and there is not currently a standardized laboratory method for diagnosing C. diff.
Lack of accurate detection is one of the reasons an infection can be deadly, so its crucial not only to know about the existence of C. diff and test for it, but to understand its symptoms. If you and your doctors strongly suspect you may have it but youve gotten a negative test result, you may want to be tested again.
The false negatives were part of what endangered my life during C. diff. Without confirmation that I had it, my doctors couldnt treat me for it. We had to assume my symptoms were due to my colitis flare, so doctors threw everything at the flareall the immunosuppressive medications they could muster. None of them worked. I was eventually hospitalized for severe weight loss, but my condition kept deteriorating and I kept losing weight.
Inclusion And Exclusion Criteria
Both inpatients and outpatients with UC who had positive results for C. difficile toxins A and B were identified from the registry and included for the study. Patients with Crohn’s disease or microscopic colitis with co-existing C. difficile infection were excluded. CDI patients without history of IBD or co-existing IBD were also excluded.
Read Also: Different Stages Of Pressure Ulcers
How Is Pseudomembranous Colitis Treated
The first thing your doctor may recommend is that you stop taking the antibiotic that led to the pseudomembranous colitis infection.
Pseudomembranous colitis is treated with antibiotics that target this infection. In most cases, doctors prescribe metronidazole , vancomycin or fidaxomicin for up to 14 days.
Pseudomembranous colitis recurs in as many as 20% of people who have been treated. If this occurs, your doctor will prescribe another dose of an antibiotic.
A newer treatment known as a fecal transplant uses stool from a healthy donor to help restore normal bacterial flora to your intestine, especially if the infection has returned after the first treatment.
What Is The Treatment For Clostridium Difficile Colitis
Treatment of C. difficile colitis includes:
- correction of dehydration and electrolyte deficiencies,
- discontinuing the antibiotic that caused the colitis, and
- using antibiotics to eradicate the C. difficile bacterium.
In patients with mild colitis, stopping the antibiotic that caused the infection may be enough to cause the colitis and diarrhea to subside. In most cases, however, antibiotics are needed to eradicate the C. difficile bacteria.
Antibiotics that are effective against C. difficile include metronidazole and vancomycin . People usually take these two antibiotics orally for 10 days. Both antibiotics are equally effective, but metronidazole is less expensive. Vancomycin is recommended in severe infections, primarily where it may be slightly more effective than metronidazole and, therefore, may be worth the additional expense. With either antibiotic, fever usually will resolve in 1-2 days, and diarrhea in 3-4 days. Several other antibiotics, some new and some older, have been used effectively against C. difficile recently, most notably fidaxomicin . Fidaxomicin may be slightly more effective than vancomycin, but its cost is high. It has the advantage of being associated with fewer recurrences.
You May Like: Venous Leg Ulcer Dressing Treatment
What Is New In C Diff
The prevalence of C. difficile infection has been increasing steadily particularly in the elderly. There have been reports from several hospitals of a newer, more virulent strain of C. difficile bacteria that produces large amounts of both toxins A and B and as well as a third toxin. This strain produces more severe colitis than the usual strains. Patients infected by this strain are more seriously ill, require surgery more frequently, and die from the infection more frequently than patients infected with the usual strains. Currently, the commercially available diagnostic tests cannot distinguish this strain from the usual strains.
Doctors are witnessing increasing difficulty in treating C. difficile colitis. Firstly, resistance to metronidazole is on the rise. Secondly, colitis is taking longer to resolve and may require higher doses of vancomycin. Thirdly C. difficile colitis relapse is common. More troublesome still, many patients experience multiple relapses, often requiring prolonged antibiotic treatment.
There Are Various Causes Of Colitis And Each Has Different Treatments
Robert Burakoff, MD, MPH, is board-certified in gastroentrology. He is the vice chair for ambulatory services for the department of medicine at Weill Cornell Medical College in New York, where he is also a professor. He was the founding editor and co-editor in chief of Inflammatory Bowel Diseases.
Colitis, which is inflammation in the large intestine, is a symptom of a disease or condition. It can be caused either by conditions that are chronic or those that come on suddenly .
Some of the causes of colitis include inflammatory bowel disease , microscopic colitis, ischemic colitis, pseudomembranous colitis , and allergic colitis.
Treating colitis will mean dealing with the underlying condition thats causing it. Because the causes are so different, there is no one treatment that will be used for every type of colitis.
This article will discuss how each type of colitis is treated. In most cases, treatments will include medications and/or changes to diet. For some conditions, certain types of surgery might also be used.
You May Like: Signs Of Ulcers In Humans
Is C Diff Contagious
Like other bacteria, Clostridium difficile is contagious. Healthy adults typically wont get sick if they come into contact with it. Some people can be C. diff carriers and transport the germ in or on their body without knowing. People with inflammatory bowel disease are at an increased risk of getting a C. diff infection due to frequent inflammation in the gastrointestinal tract and antibiotic use.
C. diff is a potentially harmful bacteria that is common in the environment. The good bacteria in the gut will usually keep you safe from C. diff. However, when your natural gut bacteria is disrupted from illness or antibiotic use, the healthy bacteria are not available to fight off infection and symptoms occur.
The symptoms of a C. diff infection can mirror an IBD flare-up. People experiencing an IBD flare-up should check with their health care provider to rule out a C. diff infection.
What Causes Clostridium Difficile Colitis
Antibiotic-associated colitis is an infection of the colon caused by C. difficile that occurs primarily among individuals who have been using antibiotics. C. difficile infections are commonly acquired during hospital stays, infecting approximately 1% of patients admitted to hospitals in the United States. C. difficile may also be acquired in the community, however.
It is the most common infection acquired by patients while they are in the hospital. More than half a million C. difficile infections occur in hospitals in the US each year, with about 300,000 occurring while in the hospital or shortly after hospitalization. After a stay of only 2 days in a hospital, 10% of patients will develop an infection with C. difficile. C. difficile also may be acquired outside of hospitals in the community. It is estimated that about 200,000 infections with C. difficile occur in the community unrelated to hospitalization each year in the U.S.
Don’t Miss: Compression For Venous Leg Ulcers
What Are The Risk Factors For C Diff Infection
People are seven to 10 times more likely to get C. diff while taking antibiotics, according to the Centers for Disease Control and Prevention .
A stay in a hospital or nursing home can also increase your chances of catching C. diff. The bacteria are capable of lingering in the environment for months, creating a vulnerable setting for the spread of C. diff to multiple hospital occupants and health care workers. As a MyCrohnsAndColitisTeam member described, My daughter got C. diff while in the hospital. It causes similar symptoms to IBD. Then she flared up at the same time. Let’s just say it was pretty ugly. I think they gave her IV Flagyl.
Other risk factors for C. diff include:
- Older age
- Weakened immune system, including from immunosuppressants
- Previous C. diff infection or known exposure
- Frequent antibiotic use
- Recent stay in a hospital, health care facility, or nursing home
How Does C Diff Cause Colitis
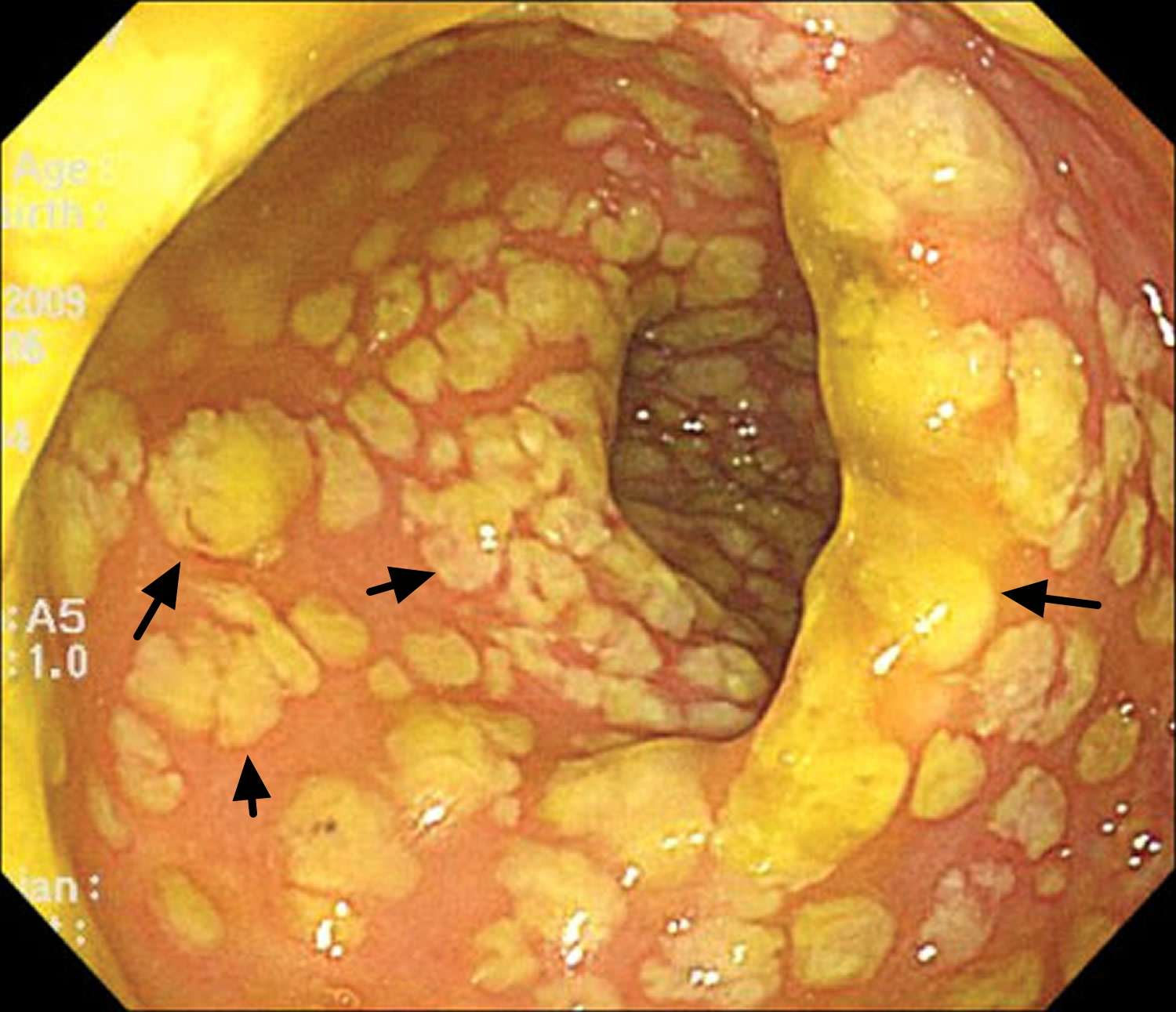
C. difficile spores lie dormant inside the colon until a person takes an antibiotic. The antibiotic disrupts the other bacteria that normally are living in the colon and preventing C. difficile from transforming into its active, disease-causing bacterial form. As a result, C. difficile transforms into its infectious form and then produces toxins that inflame and damage the colon. The inflammation results in an influx of white blood cells to the colon. The severity of the colitis can vary. In the more severe cases, the toxins kill the tissue of the inner lining of the colon, and the tissue falls off. The tissue that falls off is mixed with white blood cells and gives the appearance of a white, membranous patch covering the inner lining of the colon. This severe form of C. difficile colitis is called pseudomembranous colitis because the patches appear like membranes, but they are not true membranes.
Not everybody infected with C. difficile develops colitis. Many infants and young children, and even some adults, are carriers of C. difficile. C. difficile does not cause colitis in these people probably because
You May Like: What Can You Eat If You Have Ulcerative Colitis
Which Antibiotics Cause Clostridium Difficile Colitis
- vancomycin , and
- aminoglycosides .
In fact, metronidazole and vancomycin are two antibiotics that are used for treating C. difficile colitis however, there are rare reports of C. difficile colitis occurring several days after stopping metronidazole.
While most C. difficile colitis in the US is caused by antibiotics, C. difficile colitis also can occur in patients without exposure to antibiotics. For example, patients with ulcerative colitis and Crohn’s disease have been known to develop C. difficile colitis without exposure to antibiotics.
Since many antibiotics can cause C. difficile infection, all antibiotics should be used prudently. Self-administration or using antibiotics without an accurate diagnosis or a proper reason should be discouraged. On the other hand, benefits of properly prescribed antibiotics for the right reasons usually far outweigh the risk of developing C. difficile colitis.
Antibiotics can sometimes cause diarrhea that is not due to C. difficile infection. The reason for the diarrhea is not clear. The practical implication is that not all diarrhea associated with antibiotics should be considered to be due to C. difficile and treated as such.
History
Laboratory tests
Flexible sigmoidoscopy and colonoscopy
X-rays
Ileostomy And C Difficile Infection
Clostridioides difficile is a common cause of infectious colitis, and a less recognized cause of enteritis. There have been several reported cases of C. difficile enteritis in patients who have an end ileostomy after a total colectomy. Like colitis caused by C. difficile, C. difficile enteritis can have a wide range of clinical manifestations, ranging from diarrhea to septic shock, although the most common presenting symptom is increased ileostomy output. Risk factors include recent antibiotic use, proton pump inhibitor use, inflammatory bowel disease, and immunosuppression. Diagnosis and treatment are the same as for C. difficile colitis, as diagnosis is confirmed with stool toxin assays and first line treatment is oral vancomycin. C. difficile enteritis is a rare disease that can have a fatal outcome, and thus providers must have a high index of suspicion to reduce morbidity and mortality.
You May Like: Can You Eat Oatmeal With Ulcerative Colitis
Inflammatory Markers And Response To Antibiotic Treatment
While PCT did not discriminate between those with and without a positive stool test for C. difficile, it did differentiate those patients who would or would not respond to antibiotic therapy alone. Of the 27 patients with UC and a positive C. difficile assay, five were treated concurrently for a UC flare and CDI. The remaining 22 were started solely antibiotics to cover C. difficilethat is, the treating physicians initial impressions were that the presentation of these patients was solely due to CDI. 19 of these patients were treated with standard-dose oral vancomycin, while three of them received metronidazole. Of these 22 patients, 14 responded completely to treatment, and needed no changes in therapy for their UC, while eight did not respond to treatment, and were subsequently treated for a UC flare with symptom improvement. The median PCT for the CDI-R group was 105.3 , while for the CDI-NR group it was 40.3 , P =0.036 for the log-transformed PCT values. The area under the receiver operator characteristic curve for this comparison was 0.71 . Neither initial antibiotic choice nor mode of laboratory diagnosis differentiated CDI-R from CDI-NR.