Radiology Scans Or Diagnostic Imaging
Traditional upper GI endoscopy and colonoscopy are not be able to reach about two-thirds of the small intestine. Therefore, in addition to capsule endoscopy, various radiologic exams or diagnostic imaging may be performed to evaluate these parts of the intestines as well as to evaluate the actual wall of the bowel and surrounding areas outside the bowel.
X-rays
X-rays are the oldest way of imaging the inside of the body. X-rays are cost-effective and useful for detection of blockages in the small or large intestine.
Barium contrast studies
During a barium study, you will ingest a contrast material and have images taken with traditional X-ray technology. Barium is a chalky/milky liquid that you drink prior to the procedure. A series of X-rays are taken to observe the material flowing through the digestive system. These studies include:
Upper GI series examines the esophagus, stomach, and first part of the small bowel for patients with Crohns disease
Small bowel series and small bowel enteroclysis examines the entire small bowel. For a small bowel series, you will drink several cups of barium, and then have an X-ray taken every 1530 minutes as the barium travels down the small intestine and enters the large intestine. The time required varies but may take four to five hours. An enteroclysis is similar, except that the barium is placed directly into the small intestine through a tube introduced into the GI tract via the nose or mouth.
Cross-sectional imaging
What Are Common Tests For Ulcerative Colitis
Blood Tests
Even though blood tests alone cant diagnose ulcerative colitis, theyre an important tool in diagnosis and monitoring of the disease. These are only some of the blood tests used for UC. There are others your doctor may recommend.
These are used to detect infection, anemia , indicators of inflammation, and to identify deficiencies of vitamins or minerals.
Samples of stool may be tested for pathogenic bacteria and certain markers of inflammation. Your doctor will give you a container for collecting and storing the stool.
Imaging Tests
These are tests that take pictures of different parts of your body to provide a clearer view of your condition. They show your doctor areas of disease activity and possible complications. These are only some of the imaging tests used for UC. There are others your doctor may recommend.
A standard X-ray of your abdominal area can show narrowing, widening, or development of a perforation of the intestines or an intestinal blockagepossibly from inflammation or scarring. It may also be done to rule out certain UC complications.
This diagnostic test allows your doctor to evaluate your intestine by tracking the movement of a thick, chalky liquid called barium. The barium dye coats the lining of the bowelcreating a silhouette of your rectum, colon, and a portion of your intestine thats visible on an X-ray.
Biomarker Tests
Ways Biomarkers Can Help With UC Monitoring
Tests Before Treatment Initiation
In addition to the tests used for diagnosis, some specific tests are recommended before treatment initiation. The European Crohns and Colitis Organisation recommends that pretreatment laboratory testing include electrolyte, renal function, iron level, immunization status, and vitamin D tests. See Monitoring for tests used to monitor treatment.
Anti-JC Virus Antibodies
Testing for antibodies to JC virus is recommended in patients with CD natalizumab should be used for CD treatment only in patients negative for anti-JC virus antibodies.
Thiopurine Therapy-Related Testing
Pharmacogenetic testing before treatment initiation may be helpful to guide therapeutic decisions, particularly because treatment failure due to individual differences in medication response is not uncommon in IBD. Thiopurine drugs are commonly used in treating IBD.
The American Gastroenterological Association recommends either phenotype or genotype testing in adults beginning thiopurine therapy.TPMT and NUDT15 gene variants as well as reduced TPMT enzyme activity are associated with a greater risk of myelosuppression in response to treatment with thiopurines due to accumulation of active thiopurines. Phenotype testing should not be performed in patients already receiving treatment with thiopurines because results will be falsely low. In addition, the current TPMT phenotype may not reflect the future phenotype, particularly in patients who received blood transfusions within 30-60 days of testing.
Read Also: How Do You Know You Have A Stomach Ulcer
How Ulcerative Colitis Is Diagnosed
Ulcerative colitis has symptoms similar to many other digestive conditions, which can make diagnosis challenging. Because treatment is needed to induce remission and to prevent the disease from worsening, getting an accurate and timely diagnosis is important.
Gastroenterologists may use a variety of tests in order to understand whats going on with a patient who is suspected of having ulcerative colitis, but it is typically a colonoscopy with biopsies that is used to make the diagnosis.
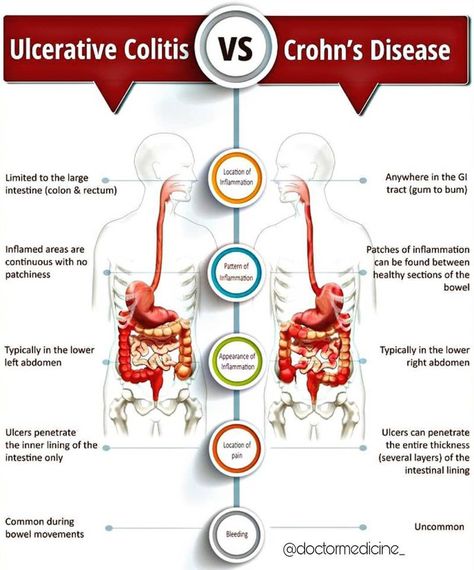
How Is Ibd Diagnosed
The path to receiving a Crohns disease or ulcerative colitis diagnosis can be overwhelming. We can help you understand the process of diagnosing inflammatory bowel disease , and the common tests and procedures your healthcare team may recommend so that you are educated and prepared.
No single test can confirm a Crohns or colitis diagnosis. Your healthcare team will evaluate your current medical history and use information obtained from diagnostic testing to exclude other potential causes of your symptoms, since gastrointestinal symptoms are common and can have a variety of causes. Getting the right diagnosis may take time, but here is some helpful information and tips to better understand the testing and diagnostic process.
Video Length00:02:50
Understanding Diagnostic and Prognostic IBD Testing Learn some of the common diagnostic tests for diagnosing and monitoring IBD as well as the goals and challenges of predicting future complications through prognostic testing.
Radiology/diagnostic imaging | Prognostic testing
Don’t Miss: What Does Having An Ulcer Feel Like
What Imaging Tests Are Used In The Diagnosis Of Ulcerative Colitis
If your laboratory reports are suggestive of inflammatory bowel disease , they will refer you to a gastroenterologist. A gastroenterologist is a doctor who specializes in treating digestive system disorders. The gastroenterologist will recommend that you undergo tests, such as sigmoidoscopy and colonoscopy. Each of the procedures requires you to take laxatives a night before to empty your colon.
Sigmoidoscopy
- This procedure helps the doctor know the extent of inflammation and ulcers, if any, in the lower colon.
- The procedure usually takes about 15-20 minutes and you can go home the same day.
- If you have been given medicines that make you sleepy, you need to stay for a few hours at the clinic or hospital until the doctor allows you to go home.
Colonoscopy
X-rays or computed tomography scan
- If your doctor wants to check if you have developed any complications of ulcerative colitis, they may order additional tests, such as a CT scan or X-ray of your abdomen. A CT scan uses strong radiation to get detailed images of the colon and other organs of your abdomen.
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
Also Check: Diet For Diabetic With Stomach Ulcer
Initial Testing And Evaluation
Your doctor will conduct a physical exam and ask you questions about your general health, diet, family history, home environment, and your daily activities.
Your doctor may then recommend a series of diagnostic tests. In addition to diagnosing ulcerative colitis, these tests are also performed to rule out infection.
Mri Scans And Mr Enterography
An MRI scan uses a magnetic field and radio waves to create two- and three-dimensional images of the body. MRI scans are especially helpful when doctors need to visualize soft tissues, such as the lining of the intestines. They may reveal small tears or ulcers, as well as irritation or bleeding.
To get a better look at the gastrointestinal tract, the doctor may ask you to drink a contrast agent just before the MRI. This is called MR enterography.
Don’t Miss: Pressure Relieving Mattress For Pressure Ulcers
Recognizing The Symptoms Of Ulcerative Colitis
How Can Stool Tests Detect Signals Of Inflammation
Stool tests can also detect certain proteins that can signal the presence of active inflammation in the digestive tract.3 These proteins are called calprotectin and lactoferrin. If the results of a stool test show an elevated level of these proteins, it suggests that there is inflammation that may be caused by IBD. To find out more, healthcare providers will usually suggest further diagnostic testing to determine the specific cause.
Also Check: What Do Diabetic Ulcers On The Feet Look Like
Daisys Story: Blood Tests
My symptoms worsened as I went through various tests to work out their cause. One of the first tests was a blood test, which doctors ordered when they believed my symptoms were happening due to a parasite. When the results came back, the doctors told me I had clear signs of inflammation.
I began taking some medications to ease my symptoms, and after these blood test results came back, the doctors referred me for further tests.
Association With Clinical Phenotypes And Prognostic Indicators
In UC, very few studies have assessed acute phase markers in predicting outcome of disease or association with clinical phenotypes. In severe UC, after three days of intensive treatment patients with frequent stools , or 3-8 stools/d and CRP > 45 mg/L should be identified, as most of them will need to undergo colectomy. It is commonly accepted that the presence of ANCA in UC is not related to the duration and age of onset. Previous studies agree that in patients affected with CD, the presence of atypical pANCAs in serum characterizes an UC-like clinical phenotype.
It is OK to experience a bout of occasional abdominal cramps and diarrhea. However, if you have been experiencing these symptoms frequently, consult your doctor. It may be a sign of inflammatory bowel disease , such as ulcerative colitis.
Your doctor will diagnose ulcerative colitis after looking at several factors, including your medical history, a physical exam and a series of medical tests. They will ask if anyone in your family has ulcerative colitis. They will also ask you about other signs and symptoms of ulcerative colitis, including
In children, the condition can also affect their rate of growth.
You May Like: Corneal Ulcer Dog Home Remedy
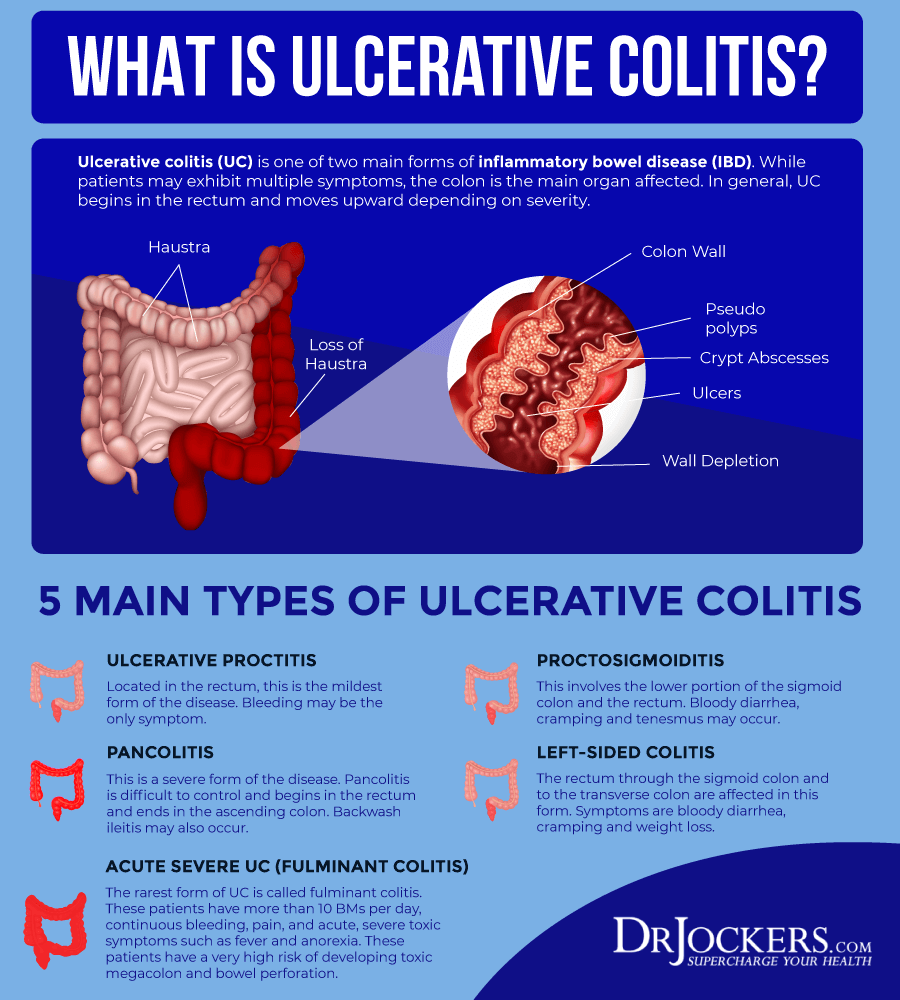
Who Gets Ulcerative Colitis And What Causes It
Colitis can develop at any age, but usually first appears in people aged 15 to 30.
Experts are not sure why UC or Crohns disease occurs in some people. It may be due to a combination of genetic, environmental and infectious factors that cause a fault in the immune system leading to inflammation of the bowel.
You May Like: Whey Protein And Ulcerative Colitis
Testing For Ulcerative Colitis
Often, symptoms alone can provide doctors with the information they need to diagnose ulcerative colitis. Your doctor will perform a physical examination and take a complete medical history that includes a careful review of your symptoms. For this reason, it is important to be candid and specific with your doctor about the problems you are having.
There is no one specific laboratory test, X-ray or scope to diagnose ulcerative colitis, however, to help confirm the condition and rule out other problems, your doctor may send you to have one or more of the following tests:
Recommended Reading: How To Determine If You Have A Stomach Ulcer
Don’t Delay Seeking Help
We know its not always easy talking about your bowel habits, but the sooner you get diagnosed, the easier your condition will be to treat.
Some important things to remember:
I always knew something wasnt right. Its not normal to bleed or feel like that. Initially, I felt scared and didnt want to tell anyone but being diagnosed helped me come to terms with it and get on with life.
ArizonaLiving with Indeterminate Colitis
Is There An Ulcerative Diet Listing Foods To Avoid And Foods That Relieve Symptoms
Proper nutrition is important for a person with ulcerative colitis. Foods do not cause ulcerative colitis, but certain food groups can cause symptoms to flare. Often it is a process of trial and error to find what foods need to be avoided. Although specific foods do not cause the disease, some types of food may trigger discomfort and diarrhea. Keep a food diary to help find foods that cause problems.
Counseling and education are important for both the patient and family a better understanding of how ulcerative colitis affects the body will allow the patient and physician to work together to control the symptoms.
Don’t Miss: Ulcerative Colitis And Lower Back Pain
What Else Should I Know
People with ulcerative colitis are at risk for colon cancer, which is related to chronic inflammation. So they should get a colonoscopy every 1-2 years, starting about 10 years after diagnosis.
Kids and teens with ulcerative colitis may feel different and not be able to do the things their friends can do, especially during flare-ups. Some struggle with a poor self-image, depression, or anxiety. They may not take their medicine or follow their diet. It’s important to talk to the doctor or a mental health provider if you’re concerned about your child’s mood, behavior, or school performance.
Parents can help teens take on more responsibility for their health as they get older. Encourage teens to take their medicine, take care of themselves, and manage stress in positive ways. Yoga, meditation, breathing and relaxation techniques, music, art, dance, writing, or talking to a friend can help.
You also can find more information and support online at:
Ulcerative Colitis Diagnosis And Testing
The path to receiving a chronic disease diagnosis can be overwhelming and even frightening at times. The best thing you can do during this time is be educated and prepared. We can help you understand the process of diagnosing ulcerative colitis and learn about common procedures your healthcare team may recommend.
An ulcerative colitis diagnosis is based on several factors, including your medical history, a physical exam, and a series of medical tests. The tests your doctor recommends will help your healthcare team determine if you have ulcerative colitis and which type of ulcerative colitis you have.
Recommended Reading: What To Eat If You Have A Bleeding Ulcer
What Happens During These Ulcerative Colitis Tests
If youve ever found yourself with nothing but a thin hospital gown separating you from a room full of medical professionals ready to look in your colon, you probably know it can feel a little weird. But lets not scare those who havent been there yet. Its really not that bad. In the case of a colonoscopy, youll likely be sedated, and wont be aware of anything anyway.
That said, youll be asked to lay on your side with your knees tucked up by your chest. Your doctor will then insert the scope into your rectum and pump air or carbon dioxide as they move through, which inflates the colon so they can see the lining better. The camera sends images to an external monitor, where the doctor will look for any issues. Other tools can also be inserted to take a biopsy or remove abnormal tissue, such as polyps, according to the Mayo Clinic.
The exam itself can take anywhere from 15 minutes to 30 minutes to an hour for a colonoscopy. If you have a colonoscopy, youll have to stick around for an hour or so as the sedative wears off and have someone drive you home. As you recover, you might feel some abdominal cramping and the urge to pass gas. Our advice? Just let it go, everyone else in recovery is doing it too.
Also Check: How Long Do Stomach Ulcers Last