What Causes Leg Ulcers To Develop
Leg ulcers develop because there is an underlying health problem or issue that is causing your body to be unable to naturally heal the skin. These health problems cause a condition known as lymphedema, a buildup of fluid in the tissues, to develop. If the skin is unable to heal naturally due to the buildup of fluid, it can result in the further breakdown of the surrounding skin which will cause the wound to increase in size.
Healthcare providers know the following health problems can result in lymphedema caused leg ulcers:
- Arterial disease
How Can I Prevent Leg Ulcers
Leg ulcers commonly open up again after healing. These steps can lower the risk of getting a leg ulcer or a wound recurrence:
- Elevate your legs above your heart when youre sitting or sleeping.
- Maintain a healthy weight and stay physically active.
- Manage health conditions that affect blood circulation, including diabetes, high blood pressure, high cholesterol and Raynauds syndrome.
- Quit smoking and using tobacco products. Talk with your healthcare provider about ways to stop smoking.
- Use gentle cleansers, and apply moisturizing lotion to prevent dry skin.
- Wear compression stockings or bandages for an hour each day to improve blood flow to the legs.
Negative Pressure Wound Therapy
The viability of new skin grafting in chronic ulcers is a major concern due to bacterial infection, chronic inflammation, tissue edema, and low oxygen in CVLUs. Negative pressure wound therapy has been used to manage a variety of wounds by granulation tissue formation, wound drainage, and preparation for delayed ulcer closures or grafting. It facilitates the sustaining and incorporation of skin grafts or flaps onto the recipient wound bed. A combination of NPWT with irrigation of oxygen loaded fluid can raise the partial pressure of oxygen of the skin around the wounds effectively, enhance the transition of macrophages from type I to type II, and may promote the growth of granulation tissue, leading to a better recipient for skin grafting or epithelization.
However, an RCT study of 46 patients comparing NPWT with hydrocolloid dressings over 5 d following autologous grafting on CVLUs failed to show the benefit of NPWT associated with skin graft over traditional dressings. This could be due to the limited number of cases enrolled.
Don’t Miss: How Do You Treat A Foot Ulcer
How Do I Take Care Of My Ulcers
Your healthcare provider may teach you how to care for your ulcers at home. Some instructions may include:
- Wash the affected area with mild soap.
- Keep the wound clean and dry.
- Change the bandages as directed.
- Take prescribed medications as directed.
- Drink plenty of fluids. Ask your healthcare provider how much water you should drink every day.
- Follow a healthy diet, as recommended by your healthcare provider.
- Exercise regularly, under your healthcare providers care.
- Wear appropriate shoes.
Recommended Reading: Offloading The Diabetic Foot For Ulcer Prevention And Healing
What Causes Leg Ulcers
Causes of leg ulcers include:
- Chronic venous insufficiency: Chronic venous insufficiency occurs when faulty valves in leg veins allow blood to flow backward into the leg where it pools. If you develop high blood pressure in the leg veins, tiny blood vessels can burst, causing inflammation, itching and dry skin. Leg ulcers develop when the skin breaks open.
- Diabetes: High blood sugar levels from diabetes can cause fat deposits to form inside blood vessels, causing them to narrow. Reduced blood flow can cause nerve damage or diabetic neuropathy. With these nerve problems, you may not be able to feel a leg ulcer or know its there. Diabetes also slows the wound healing process.
- Peripheral artery disease : This condition causes plaque to build up in the arteries . The blood vessels in the leg become narrow, leading to poor blood circulation. The reduced blood flow slows the healing of leg ulcers. People with diabetes are more likely to develop PAD.
- High blood pressure: Chronic, poorly controlled high blood pressure can cause an extremely painful ulcer on the lower leg called a Martorell ulcer. High blood pressure causes the capillaries in the skin to become narrow, cutting off the blood supply to the skin. The skin can die, forming a leg ulcer.
Don’t Miss: Ulcerative Colitis Medication Not Working
Treating Leg Ulcers At Home
Ulcers on the leg can be very painful. Treating them at home can help reduce healing time and discomfort. Itâs very important to keep the wound clean, bandaged, and dry. This helps to curb the risk of infection given the extended healing time. Following your physicianâs directives for changing the bandages can help aid in healing.
Patients should be careful to properly maintain bandaged leg ulcers. If the skin around the wound gets too wet, this can cause the ulcer to expand into these healthy tissues. Expansion of these painful wounds may require more involved treatment protocols.
Wearing compression socks daily can help support lower extremity blood circulation, speeding up the healing process. The compression can also help reduce pain and swelling. Keeping active and elevating the ulcer above the heart can also aid in healing because it promotes good circulation.
One out of twenty diabetes patients experience neuropathic ulcers each year. Neuropathic ulcers call for even more treatment interventions to encourage healing. Since they are most often caused by uncontrolled blood sugar, adhering to a diabetes maintenance plan is key. These ulcers are frequently located on the foot instead of the lower leg. As a result, avoiding pressure on the wound requires that the patient avoid walking and other activity unless absolutely necessary.
Stage : Collating Summarising And Reporting The Results
Full texts that are retained will undergo study quality assessment and critical appraisal in order to determine the applicability of findings to clinical practice. We will use the Critical Skills Appraisal Programme . Retained articles will be examined for any qualitative or quantitative descriptions. Findings will be presented in a table that outlines the study type, year the study was undertaken, sample size, study location and patient characteristics.
In order to assess the first research question, we will examine each study against two types of HL: general HL and VLU-specific HL . Findings and critical appraisal of the included articles will be provided in a summary of findings and reported in CASP evidence profile table. This table will indicate whether the paper suggested the majority of their sample lacked HL . We anticipate that there will be a highly heterogeneous definition of HL in these papers, meaning that authors will be required to use their judgements as to whether or not the paper is relevant, as a degree of simplification will be needed. All entries will be checked by two authors. The lead author will resolve disagreements independently.
You May Like: Eye Drops For Eye Ulcer
Cryopreserved Human Placental Membrane Grafts
Viable cryopreserved human placental membrane is an effective therapy for CVLUs refractory to standard of care. Adjunctive therapy with human viable wound matrix provides superior healing rates in refractory CVLUs. A retrospective review describes patients with chronic wounds that had failed standard of care treatments for more than 4 wk and were subsequently treated with weekly use of vCHPM grafts. All ulcers reached full closure in 4-5 wk with no complication. After using hVWM of cryopreserved placental tissue, 53% of CVLUs refractory to standard therapy healed completely. CVLUs were reduced in size by half more with hVWM than standard therapy . The mean rate of reduction in ulcer area was more significant after hVWM than with standard therapy .
Does Cleaning Venous Leg Ulcers Help Them To Heal
Background
Leg ulcers are open skin wounds that develop below the knee, usually because blood flow is poor in the lower leg. This can occur because of blockages, for example when small blood clots form in the veins. It can also happen when the valves in the veins that prevent blood from flowing backwards stop working properly. Poor blood flow damages the skin and tissue, and creates venous leg ulcers.
Ulcers are unsightly and may become painful or infected. On average, ulcers take from six to nine months to heal. However, some ulcers can take years to heal, and a small number never do. Once ulcers have healed, they can reoccur.
The main treatment for venous leg ulcers is to use bandages or stockings that compress the leg , to increase blood flow in the veins. It is also thought to be important to clean the wound. Different types of cleaning solutions can be used, including: normal saline water antiseptics detergents or disinfectants .
Cleaning solutions can be applied to the ulcer using a swab , a syringe with a needle, or a spray canister. Ulcers can also be bathed in the cleaning solution, using a basin or bucket, or during a shower. Cleaning can cause discomfort, and may be painful.
What did we want to find out?
We wanted to find out:
â whether cleaning venous leg ulcers helps them to become smaller and heal
â whether some cleaning solutions, or methods of applying solutions, are more effective than others
â how much cleaning wounds costs and
Our methods
Read Also: What Is Infusion Therapy For Ulcerative Colitis
What Causes Venous Ulcers
Your veins contain tiny valves that keep blood circulating throughout your body. These valves snap open and shut to move blood against the force of gravity back to your heart. In some people, venous diseases affect valve functioning. Other medical conditions, like diabetes, can also put you at risk for leg and foot ulcers.
Diagnosis And Treatment Of Venous Ulcers
LAUREN COLLINS, MD, and SAMINA SERAJ, MD, Thomas Jefferson University Hospital, Philadelphia, Pennslyvania
Am Fam Physician. 2010 Apr 15 81:989-996.
Patient information: See related handout on venous ulcers, written by the authors of this article.
Venous ulcers, or stasis ulcers, account for 80 percent of lower extremity ulcerations.1 Less common etiologies for lower extremity ulcerations include arterial insufficiency prolonged pressure diabetic neuropathy and systemic illness such as rheumatoid arthritis, vasculitis, osteomyelitis, and skin malignancy.2 The overall prevalence of venous ulcers in the United States is approximately 1 percent.1 Venous ulcers are more common in women and older persons.36 The primary risk factors are older age, obesity, previous leg injuries, deep venous thrombosis, and phlebitis.7
Venous ulcers are often recurrent, and open ulcers can persist from weeks to many years.810 Severe complications include cellulitis, osteomyelitis, and malignant change.3 Although the overall prevalence is relatively low, the refractory nature of these ulcers increase the risk of morbidity and mortality, and have a significant impact on patient quality of life.11,12 The financial burden of venous ulcers is estimated to be $2 billion per year in the United States.13,14
You May Like: Psc Liver Disease Ulcerative Colitis
Recommended Reading: What Are The Signs Of An Ulcer In Your Stomach
What Are Leg Ulcers
Leg ulcers are sores that develop on broken or injured skin. Usually, they are more prominent right above the ankles, on the inner side of your legs.
Other than skin injuries, leg ulcers may also develop as a result of an underlying medical condition. The diseases which may lead to the development of leg ulcers are discussed briefly below.
The Case For Compression Compliance

As you know, the standard treatment for venous wounds is compression. Your own experiences may tell you that compression can help reduce the risk of recurring venous leg ulcers, and research backs that up.
Heres a statistic to drive that home to your patients: Studies found that for every additional day per week that people wore a Class 2 or 3 compression garment, the odds of recurrence were cut by almost 50%.5 Typically, the higher the degree of compression, the lower the recurrence rates.4
However, compression is required as an ongoing, lifelong management strategy, and a patients adherence to that compression is crucial for success. Learn more about how to help patients comply with their compression therapy.
You May Like: Garlic Powder And Ulcerative Colitis
Faq: How Do You Treat Venous Leg Ulcers
Q. 1 What are the signs of venous leg ulcers?
Ans: There are many signs of venous leg ulcers. The most common symptom is pain and soreness around a vein in the lower leg. There may also be redness or swelling of the skin where the vein is located.
Other symptoms include heaviness or tiredness of the legs, especially after sitting for long periods of time or standing on your feet for an extended period of time feeling like you need to pop your ankles and move your foot up and down and having varicose veins that are visible on your skin.
Q. 2 How is a venous leg ulcer diagnosed?
Ans: Venous leg ulcers diagnosis doctors do by the following:
- A physical examination of the wound
- A blood test to measure the amount of oxygen in the blood
- An ultrasound scan to detect any abnormalities in the veins of the legs
- A duplex ultrasound scan to detect any abnormalities in the veins of the legs and examine for deep vein thrombosis
- Compression therapy of leg or limb, such as bandages and elastic stockings.
Q. 3 Is there a cure for venous leg ulcers?
Ans: There are many treatments for venous leg ulcers, and it is recommended to try them all before giving up. The most important thing is to keep the wound clean, dry and free from bacteria.
We should also avoid wearing any tight clothing or socks, which can put pressure on the wound and make it worse.
Q. 4 What do venous leg ulcers look like on a skin biopsy?
Q. 5 Are there any home remedies for treating venous leg ulcers?
Also Read This:
Definition And Etiology Of Venous Leg Ulcers
VLU can be defined as a full-thickness defect of the skin frequently seen in the ankle region that fails to heal spontaneously and is sustained by chronic venous disease . In more recent guidelines, a VLU is defined by best practice and uses the standard definition of an open skin lesion of the leg or foot that occurs in an area affected by venous hypertension .
Diagram representation of chronic venous disorder pathophysiology. GAG: glycosaminoglycans, MCP-1: monocyte chemoattractant protein, MIP-1: macrophage inflammatory protein, ICAM-1: intercellular adhesion molecule, VCAM-1: vascular cell adhesion molecule, NO: nitric oxide, Fe2+/Fe3+: ferrous/ferric ions, ROS: reactive oxygen species, NOS: nitrogen oxidative species, TAM: Tyro Axl MerTK receptor family tyrosine kinase, TLR: toll like receptors .
A clear understanding of inflammatory pathways allows for detailed understanding of the pathophysiology and for areas of research for treatment targets. In addition, there are significant metabolic changes that occur in the VLU cell and tissues, which affect cell function and potential for healing and also present systemically, indicating that metabolic changes are dynamic and opportunity for novel therapeutic targets .
Read Also: How To Heal Mouth Ulcers Quick
Treating An Infected Ulcer
An ulcer sometimes produces a large amount of discharge and becomes more painful. There may also be redness around the ulcer. However redness may be harder to see on black or brown skin.
These symptoms and feeling unwell are signs of infection. You should contact your GP or leg ulcer specialist as soon as possible.
If your ulcer becomes infected, it should be cleaned and dressed as usual.
You should also elevate your leg most of the time. You’ll be prescribed a 7-day course of antibiotics.
The aim of antibiotic treatment is to clear the infection. But antibiotics do not heal ulcers and should only be used in short courses to treat infected ulcers.
Learn Why Wounds Recur And How To Help Patients Manage This Chronic Disease
When it comes to healing venous leg ulcers, one of the biggest challenges and frustrations for both patients and caregivers is the tendency for the wounds to recur. They may seem to be healed, but then develop again months or years later, whether treated conservatively or with surgery.¹
Why? Because the underlying chronic venous insufficiency is there for life, explains Cristine Ray, Medline Clinical Nurse Specialist-Acute Care. In other words, Theres no magic wand for preventing leg ulcers from recurring, she says.
Its hard to determine exact statistics on how many venous ulcers recur, because there are many variables. But one multi-study analysis shows a rate as high as 40% recurring within the year and nearly 60% within three years.²
of patients with a venous ulcer have a recurrence within three years²
But there are ways to help reduce this risk.
Reducing the chance that a chronic venous leg ulcer recurs has a lot to do with the individual patients and patient compliance. What are they capable of, able and willing to do outside of your care? And what do they need to know to help drive better outcomes?
To start, its important to understand some of the risk factors for recurrence.
Don’t Miss: Stage 2 Pressure Ulcer Sacrum
Stage : Consultationpatient And Public Involvement
This ScR is the first phase in a multistage research programme aimed at developing a feasibility exercise programme as an adjunct to compression intervention for patients with VLUs. During the consultation phase, we will discuss with people with VLUs and their families and caregivers from an established Consumer Wounds Group whether the results of the ScR reflect their needs. The consultation process will take place at the time of a regular consumer group meeting. Data will be gathered using a group interview and Delphi methods. We will map the evidence and identify research gaps and report on compression and exercise treatments by investigating HL, which translates to lower abilities to adhere to self-management in the form of compression and exercise.
What Is The Best Way To Heal A Leg Ulcer
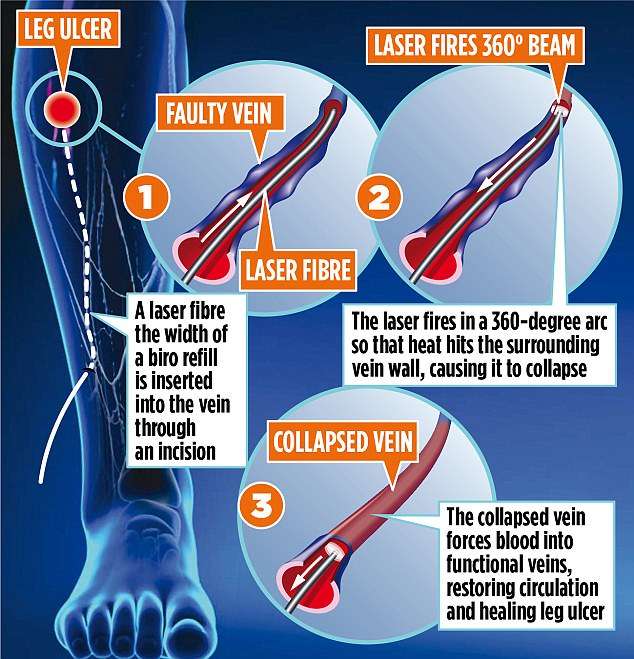
Latest research confirms that the fastest way to heal the commonest type of leg ulcer is Early endovenous ablation of superficial venous reflux, in addition to compression therapy and wound dressings.
This method reduces the time to healing of venous leg ulcers, increases ulcer-free time and is highly likely to be cost-effective .
Also Check: Ulcerative Colitis Treatment In India