New Sizes Now Available
The Repose Foot Protector is now available in a range of sizes to support a variety of patient needs.
New sizes include the Repose Foot Protector Small and Repose Foot Protector Extra Small products.
To learn more about Repose Foot Protector please contact us using the button below.
- Low Air technology distributes weight evenly and doesnt lose its shape
- Designed to relieve pressure on soft tissue areas and provide comfort
- Lightweight for easier transport
- Repose can be cleaned and reused
- Can be used with other dynamic or static support surfaces
- Reduces impact of pressure, friction and shear
What Are The Risk Factors For Bedsores
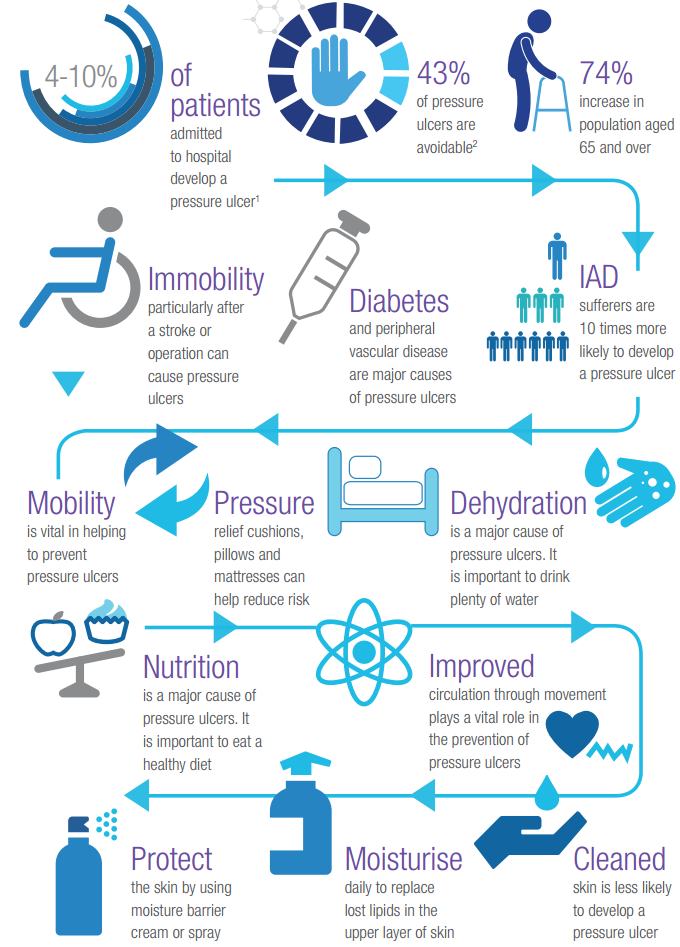
Being bedridden, unconscious, unable to sense pain, or immobile increases the risk that a bedsore will develop. The risk increases if the person is not turned, positioned correctly, or provided with proper nutrition and skin care. People with diabetes, circulation problems and malnutrition are at higher risk.
Preventing Pressure Ulcers In Hospitals
Each year, more than 2.5 million people in the United States develop pressure ulcers. These skin lesions bring pain, associated risk for serious infection, and increased health care utilization. The aim of this toolkit is to assist hospital staff in implementing effective pressure ulcer prevention practices through an interdisciplinary approach to care.
Prepared by: Dan Berlowitz, M.D., M.P.H. Bedford VA Hospital and Boston University School of Public Health Carol VanDeusen Lukas, Ed.D. VA Boston Healthcare System and Boston University School of Public Health Victoria Parker, Ed.M. D.B.A. Andrea Niederhauser, M.P.H. Jason Silver, M.P.H. and Caroline Logan, M.P.H. Boston University School of Public Health Elizabeth Ayello, Ph.D., RN, APRN, BC, CWOCN, FAPWCA, FAAN, Excelsior College School of Nursing, Albany, New York and Karen Zulkowski, D.N.S., RN, CWS, Montana State University-Bozeman.
Read Also: How To Get Remission In Ulcerative Colitis
How Can Friends And Family Help
Caregivers might sometimes provide too much help. For instance, they might turn someone over in bed although the person is actually still capable of turning over in bed themselves, perhaps with just a little assistance. It is better to only help as much as needed, so the person stays as independent as possible, helping to prevent pressure ulcers.
If you are caring for a family member at home or go to visit them in the hospital or at a nursing home, you can help them move short distances, for instance when taking a few steps to the table to sit down and eat.
If someone needs to lie in bed for a long time, a nursing care plan is usually made together with nursing professionals. This may include information such as how many times a day a person needs to be repositioned. It is important for everyone to make sure that the plan is followed properly. This also includes regularly changing diapers or incontinence pads.
You should tell the nurses or doctors immediately about any red or sore areas of skin. They can then take a closer look at the affected area. It is always important to take pressure off that part of your body.
Where It Starts: The Hospital Bed
When preventing pressure sores in hospitals, hospital beds themselves are determining factors. This is where XSENSORs ForeSite Intelligent Surface system comes in.
The system works using either a mattress overlay or an integrated mattress for hospital beds, embedded with thousands of sensor cells that continuously monitor patient body surface pressures. A bedside monitor displays real-time pressure images and clearly identifies parts of the body under sustained elevated pressure. A turn clock tracks the time between patient repositioning, and alerts staff to adjust their rotation.
This, ultimately, leads to every medical professionals goal: quality patient care and positive patient outcomes. With the support of XSENSORs technology, medical staff can focus on patient care where it is most needed, putting their energy into essential clinical activities, and not into preventative efforts that are unnecessary such as waking sleeping patients to rotate them, if they arent truly at risk of developing pressure sores.
Through providing caregivers with consistent information, XSENSORs ForeSite IS increases the integrity in continuity of care, helps avoid pressure ulcers from forming and may improve healing time for existing wounds to also reduce the length of hospital stays due to pressure ulcers.
The system comes with:
Don’t Miss: How To Soothe Mouth Ulcers
How Pressure Ulcers Develop
Pressure ulcers can develop when a large amount of pressure is applied to an area of skin over a short period of time. They can also occur when less pressure is applied over a longer period of time.
The extra pressure disrupts the flow of blood through the skin. Without a blood supply, the affected skin becomes starved of oxygen and nutrients, and begins to break down, leading to an ulcer forming.
Pressure ulcers tend to affect people with health conditions that make it difficult to move, especially those confined to lying in a bed or sitting for prolonged periods of time.
Conditions that affect the flow of blood through the body, such as type 2 diabetes, can also make a person more vulnerable to pressure ulcers.
Learn more about the causes of pressure ulcers.
Pep Prevention Emergency Project Preventive Measures For Pressure Ulcers
PEP was a patient care innovation project, which has developed a new process to effectively prevent pressure ulcers among patients in the risk zone. When initiatives are already implemented in the emergency room the entire hospital is affected since patients are often admitted from there to the various hospital wards. This also applies to other care services, such as assisted living facilities. The process is now implemented atthe hospital.
The emergency department at Karolinska University Hospital, Huddinge, run the project in collaboration with Mölnlycke. The process involves most services at the hospital, as well as five ambulance companies.
Project manager: Jenny Delin.
Also Check: Ulcerative Proctitis Vs Ulcerative Colitis
The Repose Foot/heel Protector
Repose foot protectors are designed specifically to minimise the risk of pressure damage to heels. They come in the form of splints made of Platilon, a polyurethane material with unique stretch, thermal and vapour-permeable properties. They are most effective when the patient is recumbent, semirecumbent or upright while on bed-rest, as the heels are supported above a void and therefore close to zero pressure, while the malleoli are protected by air-filled compartments.
The foot protectors are inflated using a hand-help pump. A valve ensures they are inflated to the correct pressure with no chance of over-inflation. This provides a pressure-reducing splint where the weight of the lower leg is redistributed over a wider area.
If You Use A Wheelchair
Make sure your wheelchair is the right size for you.
- Have your doctor or physical therapist check the fit once or twice a year.
- If you gain weight, ask your doctor or physical therapist to check how you fit your wheelchair.
- If you feel pressure anywhere, have your doctor or physical therapist check your wheelchair.
Sit on a foam or gel seat cushion that fits your wheelchair. Natural sheepskin pads are also helpful to reduce pressure on the skin. DO NOT sit on a donut-shaped cushions.
You or your caregiver should shift your weight in your wheelchair every 15 to 20 minutes. This will take pressure off certain areas and maintain blood flow:
- Lean forward
- Lean to one side, then lean to the other side
If you transfer yourself , lift your body up with your arms. DO NOT drag yourself. If you are having trouble transferring into your wheelchair, ask a physical therapist to teach you the proper technique.
If your caregiver transfers you, make sure they know the proper way to move you.
You May Like: Dr Reckeweg Medicine For Ulcerative Colitis
Why Heelift Boots Create A Cooler Drier Microclimate
There are a few features of Heelift® Brand Boots that help create the desired cooler, drier microclimate that prevents pressure ulcer development. As the above cut-away shows, HEELIFT® completely offloads the heel, allowing heat and moisture to escape so long as the patient is turned regularly. Additionally, the ventilation holes found in the HEELIFT® AFO, HEELIFT® Glide, and HEELIFT® Classic further help the flow of heat and moisture.
You May Like: How Do You Cure Ulcerative Colitis
Factors That Influence Sacral Ulcer Management
While wound management is a key part of sacral ulcer management, treating patients holistically is the key to success. Apart from ischemia, other factors that impede normal healing include poor nutrition, infection, edema, persistent moisture, fecal and urinary soiling, and shearing forces. One can look for, prevent, or minimize each of these risk factors. Of course, the patient should be frequently repositioned to avoid further tissue damage and to promote healing.
When selecting a dressing, the wound should be kept moist but not contain excessive amounts of exudate. Wound care professionals should consider the type of ulcer and any comorbid conditions that could complicate treatment . Arterial wounds generally require a moisture-retaining dressing, while wounds that arise from venous insufficiency usually require a dressing that absorbs excess moisture. All surfaces of the wound, including any tunnels, should be packed with the appropriate dressing.
Also Check: What Is The Medication For Ulcerative Colitis
Read Also: Pepto Bismol And Ulcerative Colitis
Background To The Indication And Devices
Pressure ulcers are localised injuries to the skin and/or underlying tissue as a result of pressure, or pressure in combination with shear . Pressure ulcers can range in severity and can be classified into the following categories or stages :
-
Stage 1 Intact skin with non-blanchable erythema of a localised area. Discoloration of the skin, warmth, oedema, hardness or pain may also be present.
-
Stage 2 Partial thickness loss of dermis presenting as a shallow open ulcer with a red/pink wound bed, without slough or bruising. It may also present as an intact or open/ruptured serum-filled blister.
-
Stage 3 Full thickness tissue loss. Subcutaneous fat may be visible, but bone, tendon or muscle are not exposed. Some slough may be present. It may include undermining and tunnelling.
-
Stage 4 Full thickness tissue loss with exposed bone, tendon or muscle. Slough or eschar may be present. It often includes undermining and tunnelling.
Pressure ulcers can have a significant impact on a patients quality of life, both physically and psychologically. They can also lead to further health complications such as infection, extended hospital stays, restricted rehabilitation and restricted treatment options for other medical conditions .
All patients are at risk of pressure ulcers. However, Mepilex Border dressings have been indicated for use in people identified as either at risk or at high risk of developing a pressure ulcer.
Guy reports that risk factors for pressure ulcers include:
Prevention Of Heel Pressure Ulcers In An Orthopaedic Unit
18 June, 2002
VOL: 98, ISSUE: 25, PAGE NO: 53
Anne Wilson, RGN, BSc, is tissue viability nurse, Royal Alexandra Hospital, Paisley
The development of hospital-acquired pressure ulcers on the heel is a well-acknowledged problem . In fact, after the sacrum the heels are the second most common anatomical site for the development of ulcers , and their incidence has increased steadily over the past few decades .
Although tissue breakdown is a complex multifactorial process, the focus with pressure ulcer development in the heels is on extrinsic factors such as pressure, shear and friction, with the most plausible explanation being the failure to relieve pressure. While many advances, such as pressure-relieving mattresses and beds, have greatly reduced the incidence of sacral ulcers . Krasner recognised that, even with pressure reduction, most support surfaces do not adequately relieve heel pressure.
Pressure ulcers may form when heel pressure on the mattress exceeds the capillary closing pressure and the heel position is not changed frequently enough . The heel is at increased risk of ulceration as it has a relatively low resting blood perfusion level if subjected to lower pressures than 32mmHg .
Cheney suggests this problem is compounded by orthopaedic surgical procedures requiring long periods in the operating room and in recuperation. To prevent the development of heel ulcers, therefore, predisposing factors must be identified, minimised and/or relieved .
You May Like: History Of Ulcerative Colitis Icd 10
Reduce Friction And Shear
Friction is the rubbing of skin on an external surface, usually bed sheets. Friction to the most commonly affected areas can be reduced with protective devices. Heel and elbow cradles are typically made of egg-crate material and Velcro on.
Skin protecting dressings, such as films and thin hydrocolloid bandages can protect the skin from repeated friction but wont help reduce pressure.
The most important thing you can do to prevent injury from the friction is to make sure you dont create any yourself when youre repositioning your loved one. Use a draw sheet to help you lift your loved one off the bed when you lift and reposition.
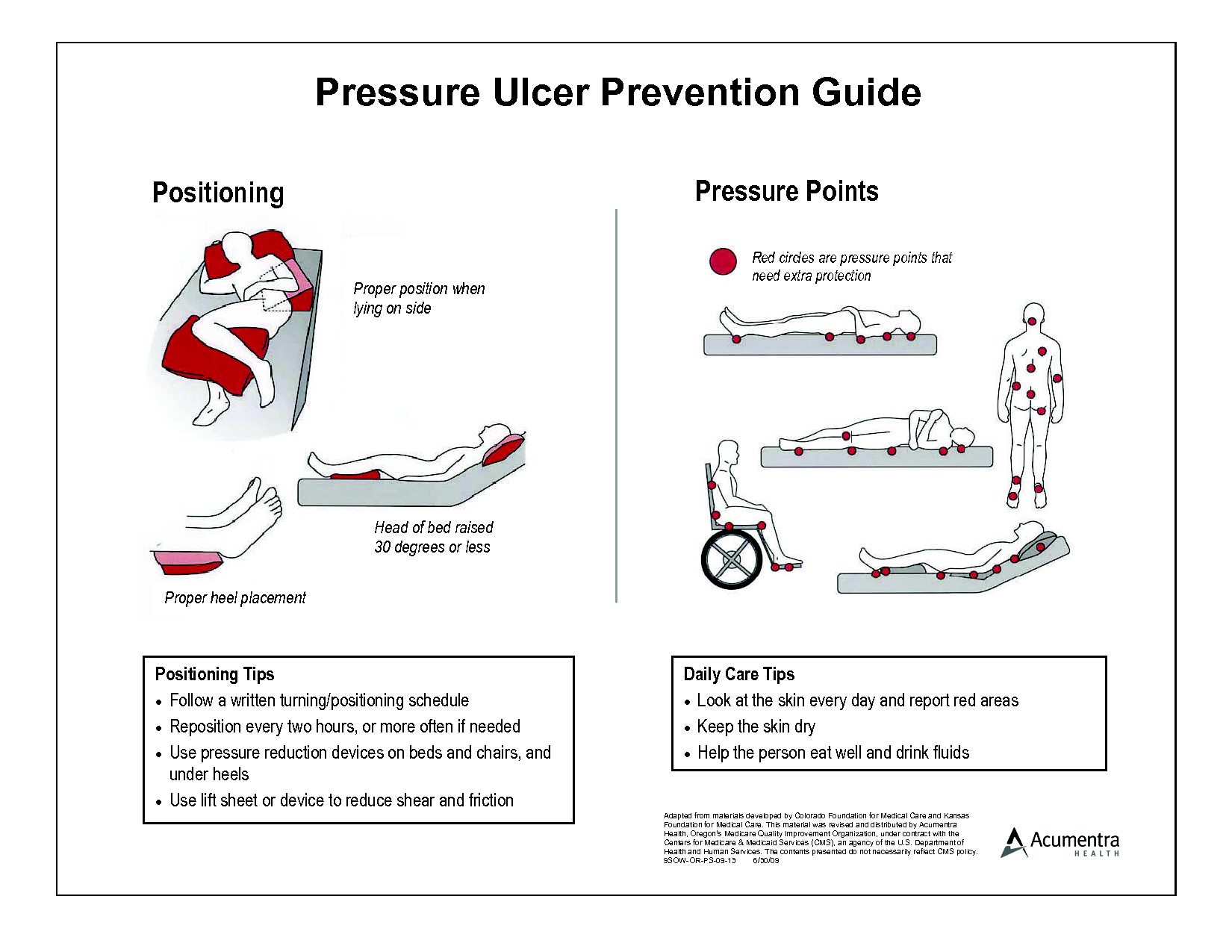
Shear is created when the deeper fatty tissues and blood vessels are damaged by a combination of friction and gravity. The best way to avoid this type of injury is to avoid a semi-Fowler and upright position in bed. A semi-fowler position is where the head is raised less than 30 degrees and upright positions more than 30 degrees.
Now, you obviously cant avoid these positions all of the time. Many patients need to be semi-Fowler to help ease shortness of breath or prevent gastric reflux and all patients need to be in an upright position to eat safely.
To minimize the risk of shear injury in a semi-Fowler or upright position, take precautions to prevent your loved one from sliding down in bed. You can do this by raising the foot of the bed and propping the knees up with pillows.
Are Pressure Ulcers Preventable
Many clinicians believe all pressure ulcers are preventable, while admitting that some may be harder than others to prevent and require more aggressiveintervention. But the truth is some pressure ulcers may not be preventable. Why? Think back to basic anatomy and the organ systems: The skin is the largest organ of the body. If your patient is in multisystem organ failure with his kidneys, liver, and heart all failing, his skin is likely to fail, too.
Whether or not you view pressure ulcers as preventable, make sure to accurately document the patients condition and all interventions taken to prevent them.
Also Check: 8 Foods To Eat During An Ulcerative Colitis Flare
Why Is Microclimate Important
In a recent study published in the Journal of Tissue Viability, Amit Gefen PhD. Dept. of Biomedical Engineering wrote, There is increasing evidence that thermodynamic conditions within and around skin tissue strongly influence the susceptibility of skin to SPUs Successful pressure ulcer prevention depends upon a complex balance between two sets of parameters the external loads applied to the skin and soft tissues, and the intrinsic ability of the skin and soft tissues to withstand prolonged or excessive loading. If the intrinsic resilience of the skin and soft tissues deteriorates, pressure damage is more likely to occur. Hence, a full understanding of a patients conditions, and immediate environment, including anything that may cause the patients skin to increase in temperature or moisture should be considered.
What Is A Pressure Ulcer?
A pressure ulcer is an injury to the skin as a result of sustained pressure applied to the skin over time . The pressure results in reduced blood flow and eventually causes skin breakdown and the development of an open wound. If the conditions leading to the sore are not rapidly corrected, the localized skin damage may spread to deeper tissue layers, affecting muscle, tendon, and bone. If not adequately treated, open ulcers can become a source of pain, disability, and infection.
Why is Prevention Important?
Customers Were Also Interested In
Getting Personal About Pressure Ulcers
Imagine that an illness or trauma puts a beloved aunt in the hospital. Although shes getting better thanks to prescribed drugs and treatments, she developsa pressure ulcer. How do you think youd feel?
Ive heard nurse colleagues justify a patients pressure ulcer as a natural part of acute illness and hospitalization. We saved the patients life, they reason. A pressure ulcer is the least of his worries. I can only assume these nurses have never had a family member develop a pressure ulcer while hospitalized.If they had, Im sure theyd take a different view. Far from expecting an ulcer to form because its a natural part of illness, chances are they would try to ensure that all measures were taken to prevent oneand if one developed, theyd consider it completely unacceptable and a sign of poor nursing care.
Even Superman can get them
In 2004, pressure ulcers got a lot of publicity when Christopher Reeve, the actor who played Superman in two movies, died from sepsis caused by a pressureulcer. The public found his case compelling because of the irony that the ventilator-dependent quadriplegic would die from something so seeminglybanal as a pressure ulcer.
If Reeve, whose wealth enabled him to receive state-of-the-art medical care, could succumb to a pressure ulcer, how can healthcare providers prevent pressure ulcers in those who are much less affluentespecially those whose medical coverage is limited after hospital discharge?
You May Like: How To Treat Mouth Ulcers
Xsensor Technology Helps To Mitigate Pressure Sore Risks
When it comes to hospital staysespecially extended staysthe topic of pressure injuries is more relevant than any hospital administrator would like. Pressure sores and pressure ulcers are intensely common, with over 2.5 million patients in the United States developing hospital acquired pressure ulcers , and an unfortunate 60,000 pressure sore-induced deaths or injuries annually.
So how can we work to mitigate their risk and improve patient outcomes? By continuously monitoring skin, keeping an eye on areas of high pressure, and working to predict spots that are vulnerable to developing sores in the first place.
At XSENSOR, weve developed software and sensors that equip healthcare workers to make informed decisions that help prevent pressure ulcers. Our guide to preventing pressure sores in hospitals is the first step to increasing risk assessment abilities and preventing pressure ulcers for your patients.
The Implications Of Pressure Injuries
Its no secret that pressure injuries can become incredibly serious, from deep tissue damage all the way to sepsis, resulting in death. Developing pressure sores can lead to skin damage and infection, causing injuries that are, in many cases, preventable. They also place a significant legal strain on hospitals. According to the Agency for Healthcare Research and Quality, there are more than 17,000 lawsuits filed related to pressure ulcers a year, and the pressure ulcers themselves cost between $9.1 billion and $11.6 billion a year in fees.
With unnecessary patient suffering and legal issues both at stake, its important to create a culture of urgency within hospitals to reduce pressure sore cases among patients. By becoming quickly aware of the issues and monitoring skin from the beginning, this is much easier to do.
Don’t Miss: Air Mattress For Pressure Ulcer Prevention