How To Recognize The 4 Stages Of Pressure Injuries
Pressure Injuries can develop quickly and often add a layer of complication to already complex medical conditions. Read more to learn how to identify and diagnose patients with stage I, II, III, and IV pressure injuries.
Have you ever heard the expression, âWhen youâre green, youâre growing. When youâre ripe, you rot.â? Well, picture what happens when you leave a piece of fruit, a peach for instance, in a bowl on the counter. Somehow, over the course of the week you forget about it, and when you return to eat it, you pick it up, only to find one side of the peach flattened and turned to mush, the skin bruised and perhaps broken in some spots.
Our skin can react in much the same way, with a condition known as pressure injuries . Pressure injuries can add another layer of complication onto already complex medical treatments, but the good news is, theyâre also relatively easy to spot and usually preventable, you just have to know what youâre looking for.
Posthoc Sensitivity Analysis Dressings Only
For the individual network, we also investigated, posthoc, our original assumption that topical agents could be used in place of dressings, by examining only the network of studies involving two or more dressings . There were no threearm trials remaining and the 30 studies compared 12 interventions in a total of 1627 participants experiencing 641 events, with 16 direct contrasts and 66 mixed treatment contrasts. The NMA rankings were similarly imprecise .
For the group network, 17 studies compared five interventions in a total of 798 participants experiencing 304 events, with five direct contrasts and 10 mixed treatment contrasts. This network was still sparse in terms of total participants, but, on average, there were more events per contrast. The posthoc sensitivity analysis had less overlap of rankograms than the full group network, and the mean rank was closer to a whole number one SUCRA value was 0 and another was 0.9. The mean ranks were: proteasemodulating 1.4 advanced 1.9 basic 3.1 antimicrobial 3.7: advancedantimicrobial 4.9. For the comparisons with basic dressing, effect estimates were similar to those in Table 4 but CIs were still wide.
Data Collection And Analysis
Two review authors independently performed study selection, risk of bias assessment and data extraction. We conducted network metaanalysis using frequentist megaregression methods for the efficacy outcome, probability of complete healing. We modelled the relative effectiveness of any two treatments as a function of each treatment relative to the reference treatment . We assumed that treatment effects were similar within dressings classes . We present estimates of effect with their 95% confidence intervals for individual treatments compared with every other, and we report ranking probabilities for each intervention . We assessed the certainty of the body of evidence using GRADE for each network comparison and for the network as whole.
You May Like: Venous Stasis Ulcer Treatment Dressings
Risk Of Bias In Included Studies
Risk of bias for all included studies is summarised in Figure 3. In order to represent ‘very high’ risk of bias, we have used two columns so very high risk of bias occurs when the cell is red in the final column .
Risk of bias summary: review authors’ judgements about each risk of bias item for each included study
We judged only one of the 51 studies to be at low risk of bias and ten to have unclear risk of bias . We judged 14 studies to be at very high risk of bias, that is, to have high risk of bias for two or more domains . We assessed the rest of the studies at high risk of bias. We grouped the low and unclear categories together.
*Studies marked with an asterisk were not included in the individual network.
Pressure Ulcer And Non
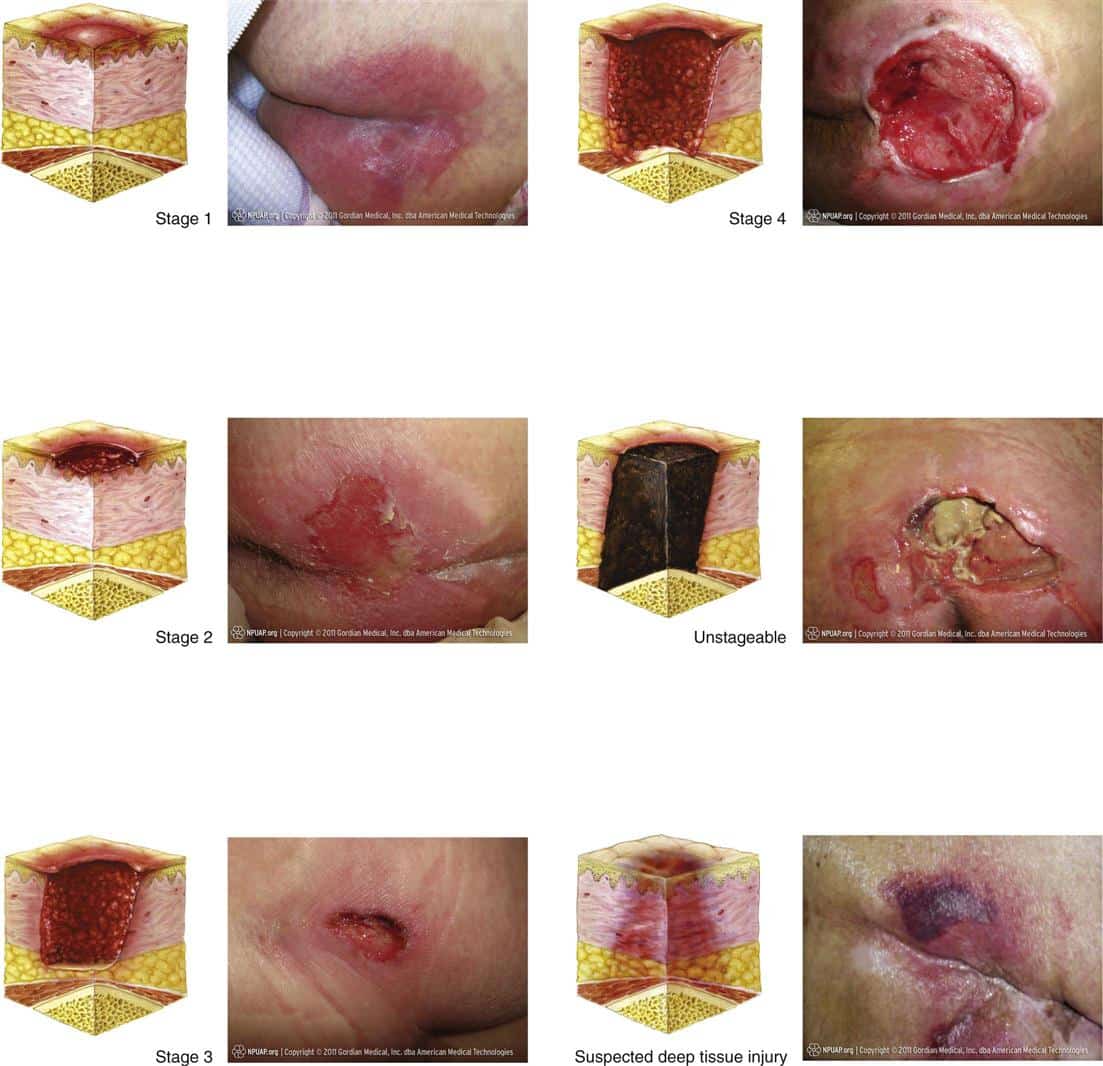
Pressure ulcer and non-pressure chronic ulcer diagnostic codes are located in ICD-10-CM chapter 12, Disease of the skin and subcutaneous tissue. The concept of laterality is pertinant, and should be included in the clinical documentation for skin ulcers.ICD-10-CM codes for Pressure ulcers, located in Category L89, are combination codes that identify the site, stage, and the laterality of the ulcer. Possible stages are 1-4 and unstageable.
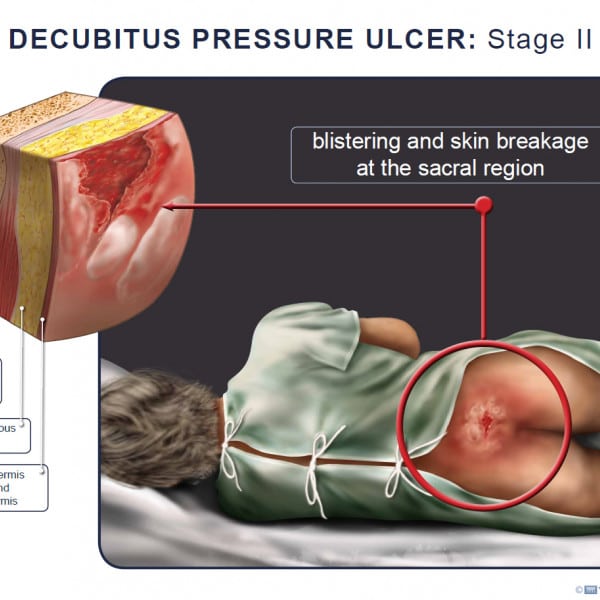
Stage 1: Skin changes limited to persistent focal edemaStage 2: An abrasion, blister, and partial thickness skin loss involving the dermis and epidermisStage 3: Full thickness skin loss involving damage and necrosis of subcutaneous tissueStage 4: Necrosis of soft tissues through the underlying muscle, tendon, or bone
Unstageable: Based on clinical documentation the stage cannot be determined clinically or for ulcers documented as deep tissue injury without evidence of trauma.An instructional note in ICD-10 states to code also any associated gangrene .Non-pressure chronic ulcers are similar to pressure ulcers in that they require documentation of the site, severity, and laterality. Category L97 and L98 are for Non-pressure ulcers, and have an instructional note to code first any associated underlying condition, such as:
Associated gangreneAtherosclerosis of the lower extremitiesChronic venous hypertensionThe severity of the ulcers is described as:Limited to breakdown of skinWith fat layer exposedWith necrosis of muscleWith necrosis of bone
You May Like: Tofacitinib Acute Severe Ulcerative Colitis
Pressure Ulcers: Prevention Evaluation And Management
DANIEL BLUESTEIN, MD, MS, Eastern Virginia Medical School, Norfolk, Virginia
ASHKAN JAVAHERI, MD, Stanford University School of Medicine, Stanford, California, and Veterans Affairs Palo, Alto Health Care System, Palo Alto, California
Am Fam Physician. 2008 Nov 15 78:1186-1194.
Pressure ulcers, also called decubitus ulcers, bedsores, or pressure sores, range in severity from reddening of the skin to severe, deep craters with exposed muscle or bone. Pressure ulcers significantly threaten the well-being of patients with limited mobility. Although 70 percent of ulcers occur in persons older than 65 years,1 younger patients with neurologic impairment or severe illness are also susceptible. Prevalence rates range from 4.7 to 32.1 percent in hospital settings2 and from 8.5 to 22 percent in nursing homes.3
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Compared with standard hospital mattresses, pressure-reducing devices decrease the incidence of pressure ulcers.
| Clinical recommendation |
|---|
|
There is no evidence to support the routine use of nutritional supplementation and a high-protein diet to promote the healing of pressure ulcers. |
|
Heel ulcers with stable, dry eschar do not need debridement if there is no edema, erythema, fluctuance, or drainage. |
|
Ulcer wounds should not be cleaned with skin cleansers or antiseptic agents because they destroy granulation tissue. |
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Living With Pressure Sores
Living with pressure sores requires a plan to move and turn frequently. Good hygiene will always be required. Pressure sores should be kept covered with a bandage or dressing. Sometimes gauze is used. The gauze must be changed once a day. Newer materials include a see-through film and a hydrocolloid dressing. A hydrocolloid dressing is a bandage made of a gel. It molds to the pressure sore and promotes healing and skin growth. These dressings can stay on for several days at a time.
Dead tissue in the sore can interfere with healing and lead to infection. Dead tissue looks like a scab. To remove dead tissue, rinse the sore every time you change the bandage. Special dressings can help your body dissolve the dead tissue on its own. The dressing must be left in place for several days. Another way to remove dead tissue is to put wet gauze bandages on the sore. Allow them to dry. The dead tissue sticks to the gauze until it is removed. For severe pressure sores, dead tissue must be removed surgically by your doctor.
Removing dead tissue and cleaning the sore can hurt. Your doctor can suggest a pain medicine. Take it 30 to 60 minutes before changing the dressing.
Healthy eating helps sores heal. Make sure youre eating the proper number of calories and protein every day. Nutrients are important too, including vitamin C and zinc. Ask your doctor for advice on a healthy diet. Be sure to tell them if youve lost or gained weight recently.
Also Check: Ulcerative Colitis And Apple Cider Vinegar
Stage 4 Pressure Injury: Full
In stage 4, full-thickness skin and tissue loss has occurred, with exposed fascia, muscle, tendon, ligament, cartilage, or bone in the ulcer. Rolled wound edges and eschar may be present. Undermining and/or tunnelling can often occur . As with stage 3 injuries, the depth and extent of damage may vary by anatomical location. For visual reference, see illustrations of pressure injuries from the NPUAP here.
There are a few other pressure injury definitions two are important here.
Stages Of Pressure Ulcers And Treatment
Pressure ulcers can progress in four stages based on the level of tissue damage. These stages help doctors determine the best course of treatment for a speedy recovery.
If caught very early and treated properly, these sores can heal in a matter of days. If left untreated, severe bedsores may require years to heal.
You May Like: What Do You Take For An Ulcer
Appendix 1 Pressure Ulcer Grading
One of the most widely recognised systems for categorising pressure ulcers is that of the National Pressure Ulcer Advisory Panel . Their international classification recognises four categories or stages of pressure ulcer and two categories of unclassifiable pressure injury, in which wound depth and/or extent, or both, cannot be accurately determined unclassifiable pressure ulcers are generally severe and would be grouped clinically with Stage 3 or Stage 4 ulcers :
The two additional categories of unclassifiable wounds are:
- Unstageable/unclassified Obscured fullthickness skin and tissue loss: Fullthickness skin and tissue loss in which the extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar. If slough or eschar is removed, a Stage 3 or Stage 4 pressure injury will be revealed. Stable eschar on the heel or ischemic limb should not be softened or removed.
Severity Of Pressure Ulcers
Healthcare professionals use several grading systems to describe the severity of pressure ulcers most common is the EPUAP grading system. Pressure sores are categorised into four stages corresponding to the depth of damage. It must however be emphasised that when an eschar is present, accurate staging is not possible.
Donât Miss: What Causes A Bleeding Ulcer In Stomach
Read Also: Best H2 Blocker For Ulcer
Appendix 2 Glossary Of Nma Terms
Armspecific outcomes/armlevel data: raw outcome data or risk) for each arm of the trial .
Assumptions for NMA: in common with all metaanalysis, the true treatment effect across trials is assumed to be described by a fixedeffect or randomeffects model. Additionally, transitivity is assumed and, concurrently, exchangeability and consistency.
Baseline risk: the absolute risk of the outcome in the ‘control’ group. This is affected by the presence of prognostic factors. Some authors have used the baseline risk as a proxy effect modifier, but in general the effect estimate is independent of the baseline risk on the other hand, the absolute risk difference depends on baseline risk.
Bayesian approach: the explicit quantitative use of external evidence in the design, monitoring, analysis, interpretation of a healthcare evaluation. In the Bayesian paradigm, prior beliefs about parameters in the models are specified and factored into the estimation. Posterior distributions of model parameters are then derived from the prior information and the observed data. In NMA, it is common to use noninformative priors for effect estimates.
Coherence/consistency: the direct effect estimate is the same as the sum of the indirect effect estimates.
Contrast/comparison/studylevel data: outcome data for the comparison .
Credible interval : the 95% credible interval is the range within which the mean value lies with posterior probability of 95%.
Studylevel data: see contrast.
Analysis
Quality Of The Evidence
We have explored the application of a new approach to GRADE analysis, alongside NMA in STATA . We applied the GRADE approach separately to effect estimates for different contrasts and to the ranking of interventions, but the two aspects are closely interrelated and, in this review, are a consequence of the sparse network and the high risk of bias through much of the network. The effect estimates were exemplified by contrasts of interventions versus saline gauze.
Across the network as a whole, the evidence was of very low certainty. There was overall high risk of bias and overlap of the ranking probability distributions, and no clearcut results. The evidence was of such poor quality that we consider it inappropriate to focus on which treatments had the highest probabilities of healing .
Don’t Miss: Sample Meal Plan For Ulcerative Colitis
Stage 4 Bedsore Prevention
The best way to prevent a stage 4 bedsore is by being proactive. If your loved one is at risk for bedsores, you can help them take the following precautions.
To prevent stage 4 bedsores, you can:
- Avoid buttons on clothes and wrinkles in bedding
- Avoid doughnut cushions, as they can add pressure to surrounding areas
- Change bedding and clothing on a regular basis
- Check skin daily
You May Like: Ulcerative Colitis Surgery Recovery Time
Deep Tissue Pressure Injury: Persistent Non
A deep tissue pressure injury presents as a localized area of persistent deep red, maroon, or purple discoloration that does not turn white when pressure is applied, or a separation revealing a dark wound bed or blood-filled blister. Pain and temperature change will often precede skin color changes. Discoloration may appear differently in darkly pigmented skin.
For more information on pressure injuries and preventive medicine, turn to MD at Home, the premier healthcare resource for primary care and geriatric medicine for homebound patients in the Chicagoland area.
Also Check: Chances To Win Social Security Disability With Ulcerative Colitis
Summary Of Main Results
We have successfully conducted a network metaanalysis of dressings and topical agents for healing pressure ulcers. Alongside the analysis we have applied a new method of GRADE assessment , which allows us to view the results in the light of our certainty in their findings. Using this approach, we found the majority of the evidence to be of low or very low certainty, and was mainly downgraded for risk of bias and imprecision . This level of uncertainty within the totality of the dataset impacts on all subsequent interpretation of its outputs.
This review includes 51 RCTs involving a total of 2964 participants, comparing 39 different dressings or topical agents for the healing of pressure ulcers. Most of the studies were in older participants, but four included participants with spinal cord injuries and one was in younger people said to be chronically ill or physically disabled. Seventeen studies included participants mainly with Stage 2 pressure ulcers and 15 mainly had Stage 3 pressure ulcers 13 studies investigated treatment of ulcers with a mean duration of less than three months.
We treated each topical agent as a separate intervention, but initially grouped dressings by class as described in the BNF 2016 . The network involved 39 studies in 2116 participants, encompassing 21 different interventions in 27 direct contrasts and these informed 210 mixed treatment contrasts.
Causes Of Pressure Ulcers
Pressure ulcers are caused by sustained pressure being placed on a particular part of the body.
This pressure interrupts the blood supply to the affected area of skin. Blood contains oxygen and other nutrients that are needed to help keep tissue healthy. Without a constant blood supply, tissue is damaged and will eventually die.
The lack of blood supply also means that the skin no longer receives infection-fighting white blood cells. Once an ulcer has developed, it can become infected by bacteria.
People with normal mobility do not develop pressure ulcers, as their body automatically makes hundreds of regular movements that prevent pressure building up on any part of their body.
For example, you may think that you are lying still when asleep, but you may shift position up to 20 times a night.
Pressure ulcers can be caused by:
- pressure from a hard surface such as a bed or wheelchair
- pressure that is placed on the skin through involuntary muscle movements such as muscle spasms
- moisture which can break down the outer layer of the skin
The time it takes for a pressure ulcer to form will depend on:
- the amount of pressure
- how vulnerable a person’s skin is to damage
Grade 3 or 4 pressure ulcers can develop quickly. For example, in susceptible people, a full-thickness pressure ulcer can sometimes develop in just 1 or 2 hours. However, in some cases, the damage will only become apparent a few days after the injury has occurred.
You May Like: Icd 10 Code Sacral Decubitus Ulcer
Search Methods For Identification Of Studies
Four existing Cochrane Reviews were relevant to this NMA , and the protocol for this NMA complemented the protocols for these four reviews . We automatically included trials from these reviews in this NMA if they reported complete healing outcomes we planned to use the extracted data from these reviews where possible, supplementing if necessary which was required as some reviews had not been completed.
We conducted searches to identify relevant trials not covered by the four Cochrane Reviews as well as recently published trials. We crosschecked the identified trials against those in the 2014 NICE guideline and the 2013 US Agency for Healthcare Research and Quality guideline on treating pressure ulcers to further locate any additional trials we also checked the references of 24 systematic reviews identified by our search.
Electronic searches
We searched the following electronic databases to identify reports of relevant randomised clinical trials:
- the Cochrane Wounds Specialised Register
- the Cochrane Central Register of Controlled Trials
- Ovid MEDILINE
- EBSCO CINAHL Plus .
We also searched the following clinical trials registries:
- ClinicalTrials.gov
- WHO International Clinical Trials Registry Platform
- EU Clinical Trials Register .
Searching other resources
Wound Care: Pressure Ulcer Best Practices
Pressure ulcers, otherwise known as decubitus ulcers, comprise a significant portion of wounds requiring specialized care and presenting additional costs, so prevention is critically important. A pressure ulcer is any lesion caused by unrelieved pressure resulting in damage of underlying tissue. Pressure ulcers usually occur over bony prominences and are graded or staged to classify the degree of tissue damage observed. Stage 1 pressure ulcers are defined as nonblanchable erythema of intact skin the heralding lesion of skin ulceration. Stage 2 is defined as partial thickness skin loss involving epidermis and/or dermis Stage 3 as full thickness skin loss involving damage or necrosis of subcutaneous tissue that may extend down to, but not through, underlying fascia and Stage 4 as full thickness skin loss with extensive destruction, tissue necrosis or damage to muscle, bone or supporting structures.
The Wound, Ostomy and Continence Nurses Society says that pressure ulcer prevention is best accomplished by identifying patients who are at risk for the development of pressure ulcers and initiating early preventive measures. According to the WOCN, This requires an understanding of risk factors, the utilization of research-based risk assessment tools, knowledge of appropriate preventive strategies and access to essential medical equipment such as therapeutic support surfaces.
Related Content:
Also Check: Irritable Bowel Syndrome Ulcerative Colitis