Find New Stress Management Techniques
Stress can trigger a colitis flare-up, so practice stress management techniques to reduce as much external stress on your body as possible.
Why does stress affect irritable bowel diseases so easily? Cortisol can increase inflammation in your body, and learning to manage stress can help you reduce that inflammatory response.
Reduce your stress levels through:
- Practicing deep breathing
- Prioritizing self-care
Self-care includes getting enough sleep each night, following a well-balanced diet, and setting aside time for your favorite activities each day.
Dont Miss: Can You Get An Ulcer In Your Intestines
Probiotic For Ulcerative Colitis Flare
Probiotic supplements have been shown to help maintain longer periods of remission and also reduce the risk of a flare-up.
A probiotic supplement was prescribed to Ulcerative colitis patients who were not responding to conventional medical approaches. This led to a remission/response rate of 77% of the patients prescribed the probiotic with no adverse reactions reported.
Read Also: Why Do I Get Mouth Ulcers
What Is A Flare
When you have ulcerative colitis, your physician will try to find the right medications to control your symptoms. However, since there is no cure, the systemic disease is always there. When the symptoms arent present, you are in remission. If the symptoms return, especially if they are worse than before, it is a flare. This is why it is important to continue taking any medications your doctor prescribes, even if you feel better. If you stop taking your medication, then you can increase your chance of experiencing a flare and progression of the disease. Infections, stress, and taking antibiotics or NSAIDs can also make you more susceptible to a flare.
Also Check: How To Stop Ulcerative Colitis Pain
Eating When You Are In Remission
While theres no cure for UC, you may experience periods of remission. During this time, youll be symptom-free and your UC wont interfere with your daily life.
Theres no definitive way to avoid flare-ups forever, but you can prolong your remission periods by maintaining a diverse and nutrient-rich diet that does not include trigger foods.
To stay symptom-free, it may be helpful to follow one of the diets that other individuals with UC find successful, as well as introduce new foods slowly and stay hydrated.
However, its important to consult with your doctor or dietician before making any changes to your diet.
Some foods that may help keep you feeling good and hydrated during remission
Look For Ways To Ward Off A Flare
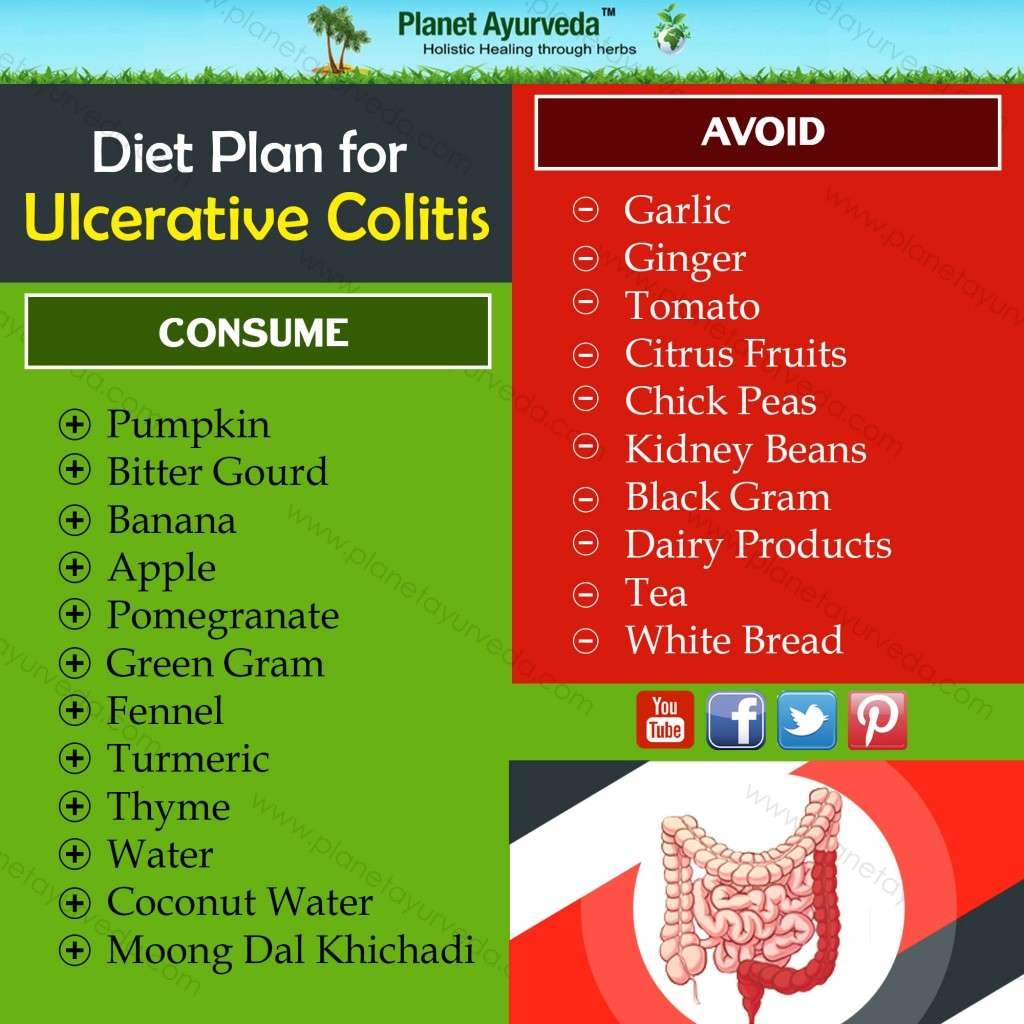
Your loved ones symptoms may be in remission now, but you can help ward off a future flare by being on the lookout for potential triggers. For example, help them avoid certain foods, such as:
- Nuts and seeds, which can irritate the GI tract
- Carbonated drinks, which can increase gas
- Popcorn, since kernels can be hard on the digestive tract
- Dairy, if theyre lactose intolerant
Encourage your loved one to keep a diary of what they eat and drink, noting the foods that are especially problematic. Dont want to keep a physical record? Theres an app available.
Also Check: What To Do For Ulcerative Colitis Flare Up
Key Points About Ulcerative Colitis
What’s Life Like For People With Uc
Life with UC varies from person to person depending on your specific disease and symptoms. But it’s not uncommon for people to battle daily digestive issues, tiredness, and more. You may also have to deal with people who don’t really understand your condition and can’t fully grasp what you’re going through, since you may, on the outside, look totally healthy .
But as you adjust to life with UC, you’ll learn more and more ways to make your life easierwhether that’s sitting in an aisle seat at the movies so you can make quick trips to the restroom, avoiding trigger foods, or putting together a self-care routine for when flare-ups strike.
But if UC is relatively new to you, or you’re exhausted and in constant pain, we understand how daunting it can be to search for good care and try new treatments. So, start small: First educate yourself about UC, then work toward building confidence in who you are as a person living with this chronic disease.
Also Check: What Causes Severe Ulcerative Colitis
How These Tips Actually Help
In the middle of a flare-up, know that these tips can help you in more ways than you think even if they dont seem like it at the moment.
You May Also Like
Tips & Tricks You Need To Help Gain And Maintain Weight
5 Ways to Prevent Recurring Kidney Stones
What the Gut?! Signs You Have an Unhealthy Gut Or Worse
Living With Ulcerative Colitis? Here Are 9 Ways to Ensure a Healthy Pregnancy
Peaches Are Fuzzy, Full of Nutrients And Beneficial to Your Health
What Causes Ulcerative Colitis In A Child
Healthcare providers don’t know what causes this condition. It may be triggered by a virus or bacteria. This interacts with your childs immune system and causes an inflammatory reaction in the intestinal wall.
Children with ulcerative colitis often have problems with their immune system. But healthcare providers don’t know if these issues are a cause or a result of the disease.
Theres no cure for this condition, except to take out your childs colon with surgery. However, the symptoms can be managed medically.
Read Also: What Foods Should I Eat With Ulcerative Colitis
More Tips To Ease Ulcerative Colitis Symptoms
The best way to shorten a flare, of course, is to get treated by your doctor. But there are steps you can take at home too.
When you have a flare, try to follow a low-residue diet for several weeks, Damas says. The goal is to let the colon rest by avoiding fiber. That means staying away from seeds, nuts, fresh fruit, dried fruit, raw vegetables, whole grain bread and cereal, and tough meat.
Were learning more now about the influence that diet can have on control of inflammation, Damas notes. When patients are having an acute flare, its important in the short term to have a low-fiber diet. Many times, for a short period of time, until the flare-up is controlled, we recommend whats called a low FODMAP diet. However, this diet is not recommended long term, because it has no impact on inflammation itself and only on control of symptoms.
Indeed, once youre in remission, Damas says your doctor will likely recommend reintroducing fruits and vegetables as tolerated. Its better to cook vegetables without the skin and consume no more than 2 cups of milk a day.
If youre lactose intolerant, be sure you choose lactose-free dairy products. Its also a good idea to cut down on fat during this time to prevent bulky stools. Avoid other potential triggers, too, such as spicy foods.
Additionally, we recommend patients avoid eating processed foods, as well as those high in fat and animal protein, as these have been associated with inflammation in some studies, Damas says.
Is It Important To Treat A Flare Early Or Is It Ok To Wait A Bit
Inflammation typically does not resolve without treatment and early intervention has a better outcome than waiting to treat. At an early stage of a flare, a more optimal baseline treatment is often enough to get the inflammation under control. If you wait, there is a greater risk that you might need drugs with greater side effects, such as oral steroids. By waiting, you will have to manage longer with your symptoms before getting relief. Living with constant or longer periods of inflammation might increase your risk for future complications, as inflammation might cause damage to the gut wall that accumulates in severity with each flare.
If you are experiencing worsening symptoms, you have probably already had the flare for some time without symptoms. Evidence shows that a stool test for inflammation in the colon, called fecal calprotectin, is often elevated for two to three months before any symptoms appear. Your colon might also start to show visual evidence of inflammation before you have symptoms, or at least indicate an increased risk for a flare.
You May Like: How To Know If I Have Ulcerative Colitis
Are Nutritional Needs Different For People With Ibd What Are The Specific Nutritional Needs For People With Crohn’s Disease And Ulcerative Colitis
Nutritional needs are specific to the individual and differ with disease state, body size and age. A nutritionist can help you estimate your individual needs. Calorie and protein needs are similar for Crohn’s disease and ulcerative colitis. In both diseases, needs increase during inflammation and immediately after to restore losses. The following are general statements about nutritional needs that may apply to you.
Five Tips For Dealing With Ulcerative Colitis Pain

There are ways to combat the pain that comes along with ulcerative colitis flare-ups. However, it is always best to get treatment from a doctor as they are most likely to efficiently and safely resolve your symptoms.
Here are five strategies you can use to help relieve symptoms and avoid a flare-up in the first place.
You May Like: How To Lose Weight With Stomach Ulcers
Don’t Miss: Ulcerative Proctitis Vs Ulcerative Colitis
Complications Caused By Nutritional Deficiencies
Some of the complications of malnutrition include:
- Dehydration diarrhoea causes your body to lose fluid, which can lead to dehydration. Severe dehydration can damage your kidneys.
- Anaemia reduced iron in the diet combined with losing blood from the bowel can lead to anaemia .
- Weight loss reduced appetite and poor absorption of food nutrients can cause weight loss.
- Reduced growth inadequate nutrition during childhood and adolescence can impair a childs growth and physical development.
Management Of Extraintestinal Manifestations146
Extraintestinal manifestations are found in both CD and UC. Those that are associated with active intestinal disease largely respond to therapy aimed at controlling disease activity, whereas those that occur whether disease is inactive or quiescent run a course independent of therapy for intestinal disease. Extraintestinal manifestations are more common in Crohns colitis and ileocolitis than in exclusively small bowel disease.
Dont Miss: How To Cure Ulcer Naturally At Home In Tamil
You May Like: Can I Take Tylenol For Stomach Ulcer Pain
Common Treatments For Ulcerative Colitis
Ulcerative colitis canât be cured, but you can usually manage the symptoms through diet, medication and/or surgery. Your consultant will discuss options with you, based on your symptoms and the extent of your bowel inflammation.
During a very severe flare-up, you may require hospital treatment as an in-patient.
Diet
Making small changes to your daily diet may relieve your symptoms. Try:
- Changing from three daily main meals to five or six small meals every day
- Drinking lots of water
- Avoiding caffeine, alcohol and fizzy drinks
Also, your consultant may recommend taking food supplements to replace nutrients lost as a result of frequent diarrhoea. You may also be referred to a dietitian, wholl help you follow an ulcerative colitis diet plan.
Medication
To prevent symptoms recurring or relieve symptoms during a flare-up, your consultant may prescribe:
- Immunosuppressants
- Aminosalicylates or steroids â to reduce inflammation
- Monoclonal antibodies â drugs which target specific cells
Surgery
If ulcerative colitis is affecting your daily life and other treatments are unsuccessful, your consultant may suggest surgery. In most cases, this involves removing your large bowel so that waste is passed out of your small intestine instead. This requires either:
- An ileostomy an opening in your abdomen for your small intestine to drain into an external pouch
Dont Miss: Peptic Ulcer Vs Gastric Ulcer
How To Manage Ulcerative Colitis Pain
Learning effective pain management strategies is a crucial aspect of living well with ulcerative colitis , a form of inflammatory bowel disease . Flare-ups can happen, even if you carefully manage your condition. Swelling of the intestine may cause bloating and painful cramping. You may experience bleeding due to skin irritation from persistent diarrhea.
During a flare-up, its not unusual to feel unwell all over. Fatigue, nausea, fever, and anxiety are common symptoms with UC. Progression of the disease can produce joint pain, skin rashes, mouth sores, and even make your eyes hurt.
UC pain can significantly impact quality of life. One MyCrohnsAndColitisTeam member wrote, Pain in my gut . So tired of being in pain. Another member posted, Woke up with the worst back pain I could ever imagine. I was in tears.
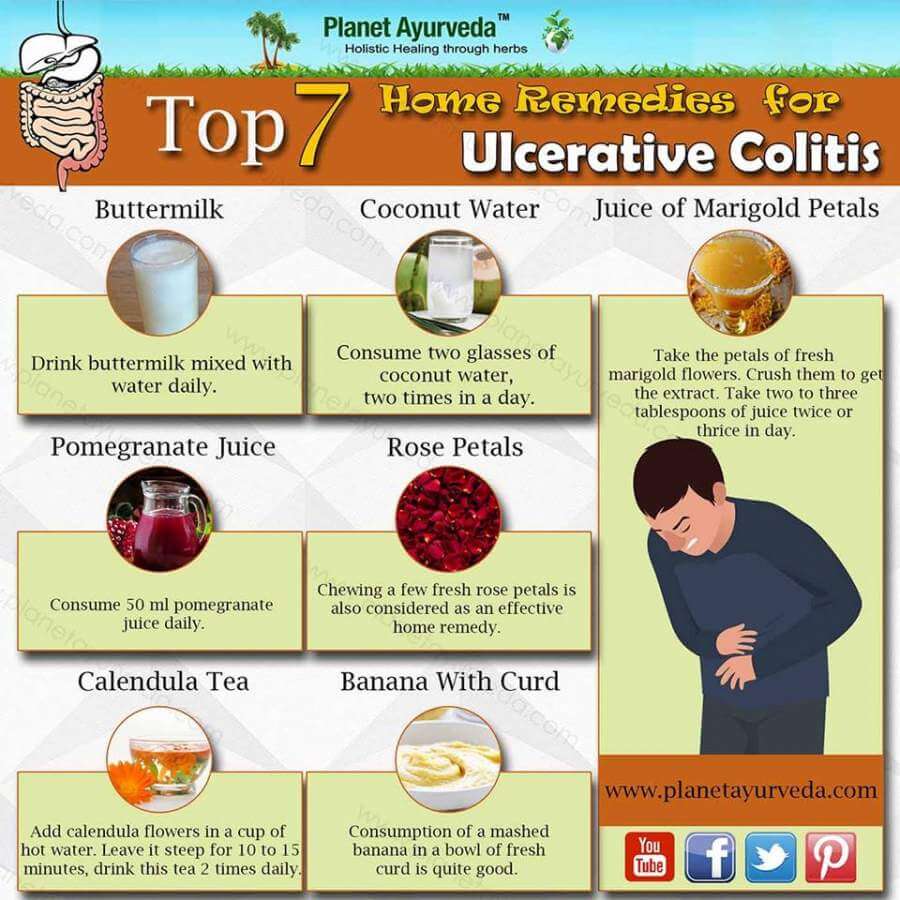
Fortunately, its possible to manage the pain associated with UC using a combination of at-home remedies, medical interventions, lifestyle changes, and alternative treatments.
Also Check: What Foods Should I Avoid With A Stomach Ulcer
Signs And Symptoms Of Ulcerative Colitis
The symptoms of ulcerative colitis can vary for each individual and they can even change over time. That said, some of the common early signs and symptoms to be on the lookout for include abdominal pain, diarrhea, an urgency to defecate, fatigue, nausea, weight loss, and anemia.
Over time, other symptoms can develop too. The Cleveland Clinic says this may include severe cramping, bloody stools, mucus or pus in the stool, fever, skin problems, mouth sores, joint pain, eye inflammation, loss of fluids and nutrients, and liver disease.
Children who develop ulcerative colitis can develop similar symptoms to adults but a symptom unique to them is delayed or poor growth. Symptoms can mimic other conditions, so its always important to have your child checked by their pediatrician for a proper diagnosis.
Recommended Reading: Whats The Signs Of An Ulcer
And Be Proactive About Probiotics
Youve probably heard about probiotics. Theyre the living microorganisms that help keep the healthful bacteria flourishing in your digestive tracthome to the largest part of your immune system. Your favorite yogurt is loaded with probiotics . According to one 2019 study, more than half of those who regularly consumed probiotics saw improvements in their general quality of life and in specific UC symptoms, including more regular bowel movements.
Also Check: What Is Bad For Ulcers
Actions For This Page
- Crohns disease and ulcerative colitis are collectively known as inflammatory bowel disease .
- Ulcerative colitis is located only in a persons large bowel .
- Diet and food allergies do not cause IBD.
- Medications help manage the symptoms of IBD.
- People with IBD can lead useful and productive lives.
- Some dietary changes can help you manage symptoms of IBD and allow medications to work better.
- Always talk with your doctor, healthcare specialist or dietitian before changing your diet. Arrange an emergency plan of action with your doctor, including after-hours phone numbers.
How Fast Does It Work
Prednisone can have a positive effect on acute severe and sudden UC symptoms. The drugs powerful anti-inflammatory properties mean that it can help control stomach pain, diarrhea, and bloody stools, among other symptoms.
According to The Arthritis Society, prednisone usually works within 14 days if a person takes the appropriate dosage. But some people may experience symptom relief within just a few hours. How quickly it works depends on how a person takes it and whether the drug is formulated for immediate or delayed release.
Don’t Miss: Diet If You Have An Ulcer
Complications Outside The Bowel
Colitis doesnt just affect the bowel. As many as 1 in 5 people with Colitis develop problems in other parts of the body. Most affected are joints, eyes or skin. These are known as extraintestinal manifestations . They usually happen during a flare-up, but can occur without or before any bowel symptoms. These complications can often happen to people who dont have Colitis too. For many of the complications, there are things you can do to reduce your risk.
Joints
You may have pain and/or swelling in your joints. Around 1 in 6 people with Colitis experiences joint problems. For some, this will get worse during a flare, but will usually improve with treatment for Colitis. Others may have joint problems even when bowel symptoms feel better. Find out more in Joints.
Bones
People with Colitis are more at risk of developing thinner and weaker bones or osteoporosis. This can be due to ongoing inflammation, smoking, taking steroids or low levels of physical activity. Calcium is needed for bone formation, and this may be low if your diet doesnt contain enough dairy. Weight-bearing exercise, calcium and vitamin D supplements, not smoking and avoiding long-term steroid use can help. Some people may also take bisphosphonate medicines. Find out more in our information on Bones.
Skin
Colitis can affect the skin in different parts of the body.
Eyes
Anemia
Anaemia can make you feel very tired. If its more severe you may also have shortness of breath, headaches, and general weakness.
Liver
When To Call Your Doctor
If youre having any of the above symptoms, make an appointment with your primary care doctor. The sooner you treat your UC, the better for your overall health. If your doc suspects UC, they will likely refer you to a gastroenterologist , which is a type of physician specializing in digestive health. Your GI can further evaluate your symptoms, run any necessary tests, and give you a diagnosis.
Even if you’re already diagnosed with UC, see a doctor ASAP if you have heavy regular diarrhea, bleeding from the rectum or blood clots in your stool, constant abdominal pain, or a high fever.
Don’t Miss: Ulcerative Colitis Joint Pain Treatment