Diagnostic Criteria For Haemophagocytic Lymphohistiocytosis
Fever 38.5 °C
Cytopenia with at least two of the following:
Absolute neutrophil count < 1.0 × 10/l
Either:
Hypertriglyceridaemia or
Haemophagocytosis in bone marrow, spleen, liver or lymph nodes
Low or absent NK-cell activity
Ferritin > 500 g/l
Soluble CD25 2 400 U/ml
On suspicion of secondary HLH, bone marrow aspiration was performed. Triglycerides and serum fibrinogen were also analysed, and were within the reference ranges. Reexamination of the patients CT abdomen revealed mild splenomegaly . The bone marrow aspirate showed occasional stromal macrophages with phagocytosed erythrocytes . Quantitative PCR revealed cytomegaloviraemia with 4 600 copies of CMV per millilitre. CMV serology detected IgM and IgG antibodies, with antibody titers showing high IgM and low IgG, consistent with current CMV infection. Other virus tests were negative.
Figure 1 Figure 2
The patient had ulcerative colitis and was undergoing immunosuppressive treatment with azathioprine. He contracted an intercurrent cytomegalovirus infection and developed probable secondary HLH.
Upon discharge after 19 days in hospital, the patient was stable and in good shape clinically. Blood values were almost normalised.
When To See A Doctor
Bleeding from the rectum or blood in or on the stool is never normal. It should always be brought up to a doctor. However, its not always an urgent situation.
If the cause of the bleeding is from a chronic condition , it should be discussed with your gastroenterologist.
In the case of new bleeding, see a doctor as soon as possible. Rectal bleeding that wont stop is a reason to go to the emergency department. Additionally, if you feel faint from blood loss, get to the emergency department right away or call an ambulance.
Abdominal pain can come and go with ongoing conditions, like Crohns disease or ulcerative colitis. Its important to discuss pain at doctors visits. However, if abdominal pain comes on suddenly and is severe, you should go to the emergency room or see a doctor right away.
In infants, caregivers will want to take the baby to see a pediatrician as soon as possible after seeing blood in the stool or around the rectum. Allergic colitis may be a common reason for bleeding, but its important to have a doctor check it out to make sure theres not a more serious reason.
Change In Bowel Movement Frequency
There is no magic number of bowel movements we should all be having each day. Some people go three-to-four times a day, and that is normal for them. Others only move their bowels once a day and that is their normal. However, if you or a loved one experiences a significant change in bowel movement frequency, whether more or less often, its important to discuss this change with your healthcare provider.
Don’t Miss: Ulcerative Colitis And Blood In Urine
Common Mistakes That Can Make Ulcerative Colitis Worse
Too much stress and not enough fluids are just a couple of things that can worsen your UC. Find out what else makes the list.
When youre in the midst of an ulcerative colitis flare, its easy to blame last night’s spicy dinner or this mornings extra-large cup of coffee. But even though there are plenty of well-known dietary and lifestyle triggers, flares can sometimes be unpredictable.
While theres no foolproof way to prevent a flare-up, there are certain steps you can take to minimize your symptoms and reach remission faster.
Here are 10 common mistakes you might be making correct them, and you may start feeling better, faster.
Why Does Ibd Cause Weight Loss
IBD causes weight loss for a few reasons:
- You have diarrhea. During an active symptom flare, you can have six or more loose bowel movements per day. Frequent diarrhea strips your body of nutrients and can lead to weight loss. Some people with IBD eat less to avoid visiting the bathroom so often.
- You feel too sick to eat. Its hard to eat well with symptoms like nausea and belly pain. When you have no appetite, you may eat fewer of the calories and nutrients that you need to maintain your weight.
- You have inflammation. During flares, theres more inflammation in your colon, leading to severe symptoms such as diarrhea and decreased appetite, which may lead to weight loss.
- You experience chronic inflammation. An increased demand for protein is often the result of chronic inflammation. When this happens, your body may start to break down muscle and other fat-free areas of mass. The decrease in muscle mass can cause you to lose weight.
- Your doctor has put you on a liquid diet. Inflammation can leave areas of scar tissue called strictures in your intestines. You may need to stick to a liquid diet until the inflammation goes down and your intestine heals.
You May Like: Can Ulcerative Colitis Cause Cancer
Complementary And Alternative Treatments For Ulcerative Colitis
Some complementary treatments may help some people in their efforts to deal with ulcerative colitis. These treatments, sometimes referred to as alternative therapies, are used in conjunction with traditional medical treatments. Complementary treatments are not meant to substitute for traditional medical care. Be sure to notify your doctor if you are consuming nutritional supplements or homeopathic remedies as they may interact with the prescribed medical therapy.
Complementary treatments may include:
- Massage therapy
- Nutritional dietary supplements, herbal remedies, tea beverages, and similar products
- Probiotics, which in one study had a positive effect on symptoms and quality of life as reported by patients with UC
- Yoga
When To See A Healthcare Provider
If you’re experiencing ongoing or severe digestive symptoms, you should see your primary care physician. Due to the difficulties involved in the diagnosis, you may be referred to a gastroenterologist.
- Significant abdominal pain could mean many things and should be checked out by a healthcare provider as soon as possible. Don’t assume this is due to IBD if it’s accompanied by vomiting, nausea, and fever. These are potential symptoms of a bowel obstruction, which requires immediate medical care.
- Any blood in the stool should always be checked out by a medical professional right away. The blood loss of UC and IC can be significant. If it continues or is accompanied by diarrhea, pain, or vomiting, see a practitioner immediately.
- If the mucus in stool is accompanied by abdominal pain, vomiting, or diarrhea, see a healthcare provider right away to get it checked out.
- Suddenly losing weight unexpectedly is a reason to talk to a practitioner, especially if there is also ongoing diarrhea, vomiting, or a lack of appetite.
- If diarrhea doesn’t resolve on its own and is also accompanied by abdominal pain, blood in the stool, weight loss, fever, or other symptoms, see a healthcare provider as soon as possible.
If abdominal pain is severe or rectal bleeding is substantial, you may have a serious condition that needs emergency medical treatment.
Also Check: What To Eat If You Have Gastric Ulcer
Causes Of Ulcerative Colitis
The cause of ulcerative colitis is unknown. Researchers believed that stress was a possible cause, but they no longer believe that this is a viable explanantion. However, stress can aggravate symptoms. There are now two possibilities for the cause of ulcerative colitis.
- Immune system: some scientists believe that a virus or bacterium may trigger ulcerative colitis. The digestive tract becomes inflamed when the immune system tries to fight off the invading pathogen. It is also possible that inflammation may stem from an autoimmune reaction.
- Hereditary: youre more likely to develop ulcerative colitis if you have a parent or sibling with this disease. However, most people who have ulcerative colitis do not have a family history of ulcerative colitis.
Chronic Constipation Or Constipation Alternating With Diarrhea
It is normal to occasionally feel constipatedhaving difficulty moving bowels or infrequent bowel movements. There are a variety of reasons why someone may experience occasional constipation. But if you or a loved one is frequently experiencing constipation, or constipation alternating with diarrhea, it is important to see a healthcare provider or gastroenterologist. Your healthcare provider will be able to run tests to determine the cause of the constipation and recommend for the best course of treatment for you or your loved one.
Also Check: Natural Ways To Heal Stomach Ulcers
Food As Trigger Of Flare
Participants frequently discussed the possibility that certain foods could trigger flares, but had great difficulty in identifying common themes across participants.
I never could figure out what triggers it. When Ive got a flareup going, I mean, its always, I eat, and then half an hour later Im in the bathroom.
I know until I kept a food journal, I had no concept of what would or wouldnt trigger it. I just its hard to isolate.
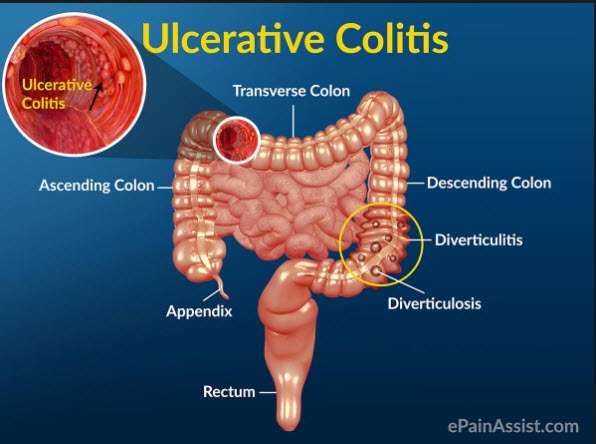
Classifications Of Ulcerative Colitis And Their Symptoms
- Ulcerative proctitis: Inflammation is confined to the area closest to the anus . For some people rectal bleeding may be the only sign of the disease. Others may have rectal pain and a feeling of urgency . This form tends to be the mildest.
- Proctosigmoiditis: Involves the rectum and the lower end of the colon, known as the sigmoid colon. Bloody diarrhea, abdominal cramps and pain.
- Left-sided colitis: Inflammation extends from the rectum up through the sigmoid and descending colon, which are located in the upper left part of the abdomen. Bloody diarrhea, abdominal cramping and pain on the left side and unintentional weight loss.
- Pancolitis: Affects more than the left colon and often the entire colon. Bloody diarrhea that may be severe, abdominal cramps and pain, fatigue and significant weight loss
- Fulminant colitis: A rare, life-threatening form of colitis affects the entire colon and causes severe pain, profuse diarrhea and, sometimes, dehydration and shock. People with this condition are a risk of serious complications, including colon rupture and toxic megacolon, a condition that causes the colon to rapidly expand.
Recommended Reading: How To Heal Ulcers In Large Intestine
Strategies For Handling Nausea After Eating
Even though I have a J-pouch, my nausea is often extremely debilitating, making it hard for me to function at work or when Im out with friends. Ive consulted with a dietitian who specializes in ulcerative colitis, and shes helped me really understand what foods to avoid and why.
Ive also figured out a few other coping strategies:
What Color Is Blood From Ulcerative Colitis

The blood color can range from bright red to maroon, with or without blood clots. This symptom often accompanies lower abdominal pain and the urgent need to defecate. Blood from the rectum and large intestine is usually bright red. If blood is a darker color, it may be coming from higher up the gastrointestinal tract.
Read Also: Best Ulcerative Colitis Diet Book
Symptoms Of Ulcerative Colitis
The main symptoms of ulcerative colitis are:
- recurring diarrhoea, which may contain blood, mucus or pus
- needing to empty your bowels frequently
You may also experience fatigue , loss of appetite and weight loss.
The severity of the symptoms varies, depending on how much of the rectum and colon is inflamed and how severe the inflammation is. For some people, the condition has a significant impact on their everyday lives.
When Symptoms Get Severe
In some cases, UC can in some cases cause life-threatening complications including severe bleeding, perforated colon, and severe dehydration. If any of these conditions are present, its a medical emergency and the person should get immediate medical attention. UC can also cause an increased risk of colon cancer and blood clots in the veins and arteries.
Also Check: Causes Of Ulcers In Horses
How Can I Prevent Weight Loss With Uc
Doctors dont recommend any one diet for people with UC. The idea is to eat foods that give you enough calories plus a balance of protein, healthy fats, vitamins, and minerals. Work with a dietitian to find a meal plan you can tolerate and that you enjoy.
Certain foods can make UC symptoms worse. During flares, you may need to avoid certain hard-to-digest foods and drinks like:
- fresh fruits with skin and seeds
- raw vegetables
- dairy, such as milk and cheese
- nuts
- sugary foods, such as candy and soda
- alcohol
However, you dont need to automatically cut all these items out of your diet.
Instead, you can figure out which foods bother you with the help of a food diary. Write down everything you eat and drink, and take note of when your symptoms flare up. Share this diary with your doctor and dietitian. Together, you can come up with a plan that ensures youre eating balanced meals.
After a flare, you can slowly add foods back into your diet. Youll want to try and increase your calorie and protein intake to make up for what you lost.
Here are a few other tips to help you put on weight:
Finally, talk to your doctor about UC treatments. Medications can help to manage inflammation and ease the symptoms that prevent you from eating and gaining weight.
It Helps To Have A Network Of People With Ulcerative Colitis
Hopefully, youll find yourself with a tight-knit group of friends and family members who are ready to support you through even your very worst days. But no matter how well-intentioned those loved ones are, the only people wholl really get what its like to live with ulcerative colitis are other people who have it.
Even my best friend and my boyfriend will never understand what I’ve gone through like my friends that have ulcerative colitis do, Skomski says. Until you live it, you don’t know what it feels like to go through all those years of people not believing you, having the worst pain in your life that you have no understanding of. For a really long time, when I was in my denial phase, I thought, I don’t need to have those people in my life, it’s just gonna make me feel like the sick girl all the time. But to have people that have gone through the same thing changed my life. I don’t think I would be so positive and would embrace it as much as I do if it weren’t for having those people in my life that have the same disease as me.
It can also be such a relief to save valuable energy by skipping a few steps in the explaining process. I’m so used to having to go through the whole song and dance of This is what I went through, Skomski says. When I connect with people that have ulcerative colitis, I don’t have to do that. It’s like a weird bond that I didn’t know that I wanted or needed, but I definitely do.
Recommended Reading: Offloading The Diabetic Foot For Ulcer Prevention And Healing
Abdominal Pain And Bloating
Stomach bloating, distention, cramps or pain in the abdominal or bowel region can be symptoms of colon or rectal cancer. These are common issues that can also be caused by a number of conditions, including diet-related gastrointestinal distress, Crohns disease or ulcerative colitis. See your doctor if you experience frequent abdominal pain and bloating that does not have an obvious cause.
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
- Alcohol.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Salt.
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
Also Check: Ulcerative Colitis Surgery Pros And Cons
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.