Which Wound Dressing Is Best For Your Pressure Ulcer
Now that weve touched on some of the more common types of dressings used for pressure ulcers, you may be wondering which is the best for your particular situation. The answer will depend on multiple factors including where the pressure ulcer is located, how severe the bedsore is, and the degree of skin and tissue damage. Talk to your health care professional about any pressure wounds you notice on your body as soon as possible.
How The Intervention Might Work
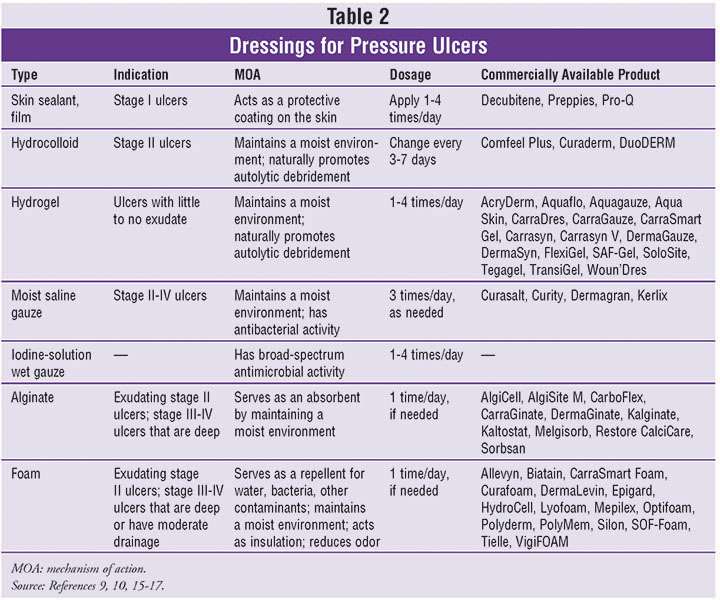
The principle of moist wound healing governs wound care practice today. This is optimised through the application of occlusive or semiocclusive dressings and preparation of the wound bed . Animal experiments performed 50 years ago suggested that acute wounds healed more quickly when their surface was kept moist, rather than being left to dry and to scab . examined the rate of epithelialisation in experimental wounds cut into the skin of healthy pigs, comparing wounds with a natural scab exposed to the air against wounds that were covered with polythene film. He found that epithelialisation occurred more quickly in the latter.
The principle of moist wound healing has led to the development of several commercially available wound dressings to support optimal healing processes. These have revolutionised wound management products include hydrogels that retain moisture in contact with the wound, hydrocolloids that absorb small amounts of excess moisture without drying the wound bed, absorbent foams, alginates, adhesive dressings, nonadhesive dressings and siliconebased lowadherent dressings. Hydrocolloid dressings are composed of a layer of sodium carboxymethylcellulose bonded onto a vapourpermeable film or foam pad. These occlusive dressings absorb exudate whilst maintaining a moist wound environment. Fibrous hydrocolloids are a subset of dressings that are designed for use in wounds with heavy exudate in lieu of alternate dressing types such as alginates .
What Are Pressure Sores
Pressure sores are sores on your skin. Theyre caused by being in a bed or wheelchair nearly all the time. Sometimes theyre called bedsores or pressure ulcers. The sores usually develop over the bony parts of your body. Those are places with little padding from fat. Sores are common on heels and hips. Other areas include the base of the spine , shoulder blades, the backs and sides of the knees, and the back of the head.
People who need to stay in bed or in a wheelchair for a long time are at greater risk of developing pressure sores. This can include people who are paralyzed and those who arent able to get up on their own. But even some people with short-term illness and injuries can get pressure sores. Sores can happen if they have to stay in bed or a wheelchair while they heal. Lastly, some chronic diseases make it hard for pressure sores to heal. Those include diabetes and hardening of the arteries.
You May Like: Skin Prep For Pressure Ulcers
Assessment Of Nutritional Needs
Undernutrition is common among patients with pressure injuries and is a risk factor for delayed healing. Markers of undernutrition include albumin< 3.5 g/dL or weight < 80% of ideal. Protein intake of 1.25 to 1.5 g/kg/day, sometimes requiring oral, nasogastric, or parenteral supplementation, is desirable for optimal healing. Current evidence does not support supplementing vitamins or calories in patients who have no signs of nutritional deficiency.
What Are Stage 3 Bedsores
Bedsores, also known as pressure ulcers or decubitus ulcers, are broken down into four stages based on their severity. Stage 3 bedsores have burrowed past the dermis and reached the subcutaneous tissue beneath.
Stage 3 bedsores pose a high risk of infection and can take months to heal from. Some pressure sores may even progress to the fourth and most dangerous stage without proper treatment.
Nursing homes that hire enough well-trained staff can often provide the care needed to prevent serious bedsores. If a nursing home resident develops a stage 3 bedsore, it may mean the facility is not properly caring for them.
Thankfully, there are ways to get help if your loved one develops a stage 3 bedsore. For example, loved ones can access medical care to keep a residents bedsore from worsening. They may also be able to take legal action against the nursing home to get compensation for treatment costs.
- Helps to prevent biofilm formation
- Reduces healing time
It moistens wound dressings and dissolves encrusted bandages or wound dressings during dressing changes.
Prontosan® Gel X proper wound cleansing is essential. The use of Prontosan® Wound Gel X provides long-lasting cleansing and decontamination of the wound bed between dressing changes.
Prontosan® Debridement Pad has been designed to support the wound bed preparation when used in conjunction with Prontosan® Wound Irrigation Solution.
You May Like: Foods That Cause Stomach Ulcers
Who Is At Risk For Developing Pressure Injuries
- People with a limited amount of mobility or a total inability to move. Those in wheelchairs or bedridden are at particular risk and need to be moved or turned regularly.
- Those with prosthetic limbs. If the device does not fit properly, the skin can be irritated and a pressure injury can develop.
- People with a loss of sensation. They are at risk because they may not feel the pressure being applied to the skin. As a result, they may not move, which could worsen the damage.
- Those with malnutrition. Wound healing is slowed when nutritional needs are not met.
- The elderly. As people age, the skin naturally becomes thinner and more easily damaged.
Search Methods For Identification Of Studies
Four existing Cochrane Reviews were relevant to this NMA , and the protocol for this NMA complemented the protocols for these four reviews . We automatically included trials from these reviews in this NMA if they reported complete healing outcomes we planned to use the extracted data from these reviews where possible, supplementing if necessary which was required as some reviews had not been completed.
We conducted searches to identify relevant trials not covered by the four Cochrane Reviews as well as recently published trials. We crosschecked the identified trials against those in the 2014 NICE guideline and the 2013 US Agency for Healthcare Research and Quality guideline on treating pressure ulcers to further locate any additional trials we also checked the references of 24 systematic reviews identified by our search.
Electronic searches
We searched the following electronic databases to identify reports of relevant randomised clinical trials:
- the Cochrane Wounds Specialised Register
- the Cochrane Central Register of Controlled Trials
- Ovid MEDILINE
- EBSCO CINAHL Plus .
We also searched the following clinical trials registries:
- ClinicalTrials.gov
- WHO International Clinical Trials Registry Platform
- EU Clinical Trials Register .
Searching other resources
You May Like: Natural Medicine For Ulcerative Colitis
When Should I Call The Doctor
If you suspect you have a pressure injury, speak with your doctor. A pressure injury is easier to heal if it is discovered in the early stages. It is important to prevent a wound from becoming infected. Healing is delayed in an infected wound and the infection could cause problems in other areas of the body.
Hydrogel Dressings Consist Of A Starch Polymer And Up To 96% Water
Pressure ulcer prevention, operating room, wound dressing, friction. Managing sacral pressure ulcers with hydrocolloid dressings: Secondary outcomes were time to heal, ulcer area healed per day, linear healing of wound edge, and cost of therapy. Pressure ulcers will not heal by dressings alone, but need the pressure eliminated, . Treating the underlying cause will often address and promote wound healing. Analysis by intention to treat revealed . These dressings can absorb wound exudate or rehydrate a wound depending on . The use of duoderm® dressings has proven advantages to support wound healing. Dressing, nursing time, wound cleansing and debridements 8. Hydrogel dressings consist of a starch polymer and up to 96% water. Hydrocolloid is made for difficult to dress wounds. Hydrocolloid dressing reduce the risk of pressure ulcer .
These dressings can absorb wound exudate or rehydrate a wound depending on . Pressure ulcers will not heal by dressings alone, but need the pressure eliminated, . Hydrocolloid dressing reduce the risk of pressure ulcer . Pressure ulcer prevention, operating room, wound dressing, friction. The use of duoderm® dressings has proven advantages to support wound healing.
Recommended Reading: Best Dog Food For Dogs With Stomach Ulcers
Disadvantages Of Hydrocolloid Dressings
These types of dressings are not appropriate for all wounds and should not be used if there is heavy exudate or infection. Other disadvantages include:
- It can be difficult to assess the wound through the bandage
- Bandages might curl or roll on edges
- Sometimes dressing adheres to the wound and causes trauma to the fragile skin when removed
- Dressings can cause periwound maceration or hypergranulation of wound
How Should You Treat A Stage 1 Pressure Ulcer
If you believe that you have a stage 1 pressure ulcer, you should remove all pressure from the area. Keep the area as dry and clean as possible to prevent bacterial infections. To speed up the healing process, you should eat adequate calories and have a diet high in minerals, proteins, and vitamins. Zinc, iron, vitamin A, and vitamin C will play the biggest role in the healing process. Drink water frequently to remain hydrated.
Inspect the stage 1 pressure ulcer at least twice a day. Usually, you can reverse a pressure ulcer in this stage in about two to three days as long as pressure is removed. If the pressure ulcer hasnt gone away after three days, you should call your physician.
For more information about the treatment for a stage 1 pressure ulcer or to schedule an appointment, dont hesitate to contact at DFW Wound Care Center at in Plano, in Lewisville or in Irving.
You May Like: Acute Exacerbation Of Ulcerative Colitis Treatment
What To Do If You Have A Stage 3 Pressure Ulcer
You must seek immediate medical treatment if you have a stage 3 pressure ulcer. These sores need special attention. Your doctor may prescribe antibiotic therapy and remove any dead tissue to promote healing and to prevent or treat infection.
How long does it take for Stage 4 pressure ulcer to heal?
If you are immobilized, your doctor may recommend a special mattress or bed to relieve pressure from the affected areas. Ulcers in this stage usually need at least one to four months to heal. Stage 4 ulcers are the most serious. These sores extend below the subcutaneous fat into your deep tissues like muscle, tendons, and ligaments.
Appendix 10 Ranking Interventions
Data for each intervention were shown as the probability that each intervention is the best, second best, third best treatment, etc. . There was substantial overlap of the individual rankograms, illustrated in Figure 21, which intentionally shows the confusion, together with some indication that dextranomer and tripeptide copper gel may be the best treatments and that the worst treatments may be the sequential hydrocolloidalginate dressings and sugar plus egg white. Across all treatments there was considerable uncertainty in the ranking of interventions and no intervention had more than 50% probability of being the best treatment. This, together with the mean rank being no higher than 3.6 and no lower than 18.6 , and no SUCRA value being 0 or 1, reinforces our view of the considerable uncertainty around treatment estimates in this network.
Rankograms combined individual networkKey to interventions: 1: saline gauze 2: alginate dressing 3: sequential hydrocolloid alginate dressings 4: basic wound contact dressing 5: collagenase ointment 6: dextranomer 7: foam dressing 8: hydrocolloid dressing 9: hydrocolloid +/ alginate 10: hydrogel dressing 11: ineligible radiant heat 12: ineligible skin substitute 13: iodinecontaining dressing 14: phenytoin 15: proteasemodulating dressing 16: PVP + zinc oxide17: silicone + foam dressing 18: soft polymer dressing 19: sugar + egg white 20: tripeptide copper gel 21: vapourpermeable dressing
Don’t Miss: Safe Vegetables For Ulcerative Colitis
Treatment Of Stage 3 And Stage 4 Pressure Ulcers
The goal of treatment for stage 3 and 4 pressure ulcers, is to properly debride and dress the wound cavity, create or maintain moisture for optimal healing, and protect the wound from infection. The goal of properly unloading pressure from the area still applies. At these pressure ulcer stages, more emphasis should be placed on proper nutrition and hydration to support wound healing. If the extent of the pressure ulcer or other factors prohibit it from healing properly, surgery may be necessary to close the wound.
The following precautions can help minimize the risk of developing pressure ulcers in at-risk patients and to minimize complications in patients already exhibiting symptoms:
- Patient should be repositioned with consideration to the individualÃâs level of activity, mobility and ability to independently reposition. Q2 hour turning is the standard in many facilities, but some patients may require more or less frequent repositioning, depending on the previous list.
- Keep the skin clean and dry.
- Avoid massaging bony prominences.
Also Check: Probiotics Good For Ulcerative Colitis
What Are The Treatment Options For Pressure Ulcers
The present treatment options include various approaches of cleaning the wound, debridement, optimised dressings, role of antibiotics and reconstructive surgery.
How long does it take for a pressure ulcer to heal?
Pressure ulcers can progress in four stages based on the level of tissue damage. These stages help doctors determine the best course of treatment for a speedy recovery. If caught very early and treated properly, these sores can heal in a matter of days.
Also Check: Can I Live A Normal Life With Ulcerative Colitis
How To Apply Hydrocolloid Dressings
Applying a hydrocolloid dressing is similar to the best practices for most wound care. Follow these steps:
Also Check: Medical Management Of Ulcerative Colitis
Wound Care For Pressure Ulcers
While stage 3 and 4 pressure ulcers should be cleaned and treated by a wound care specialist, there are things you can do to care for wounds that are in the first two stages. That said, its still recommended to seek professional guidance on proper caring methods.
Added pressure can cause the ulcer to break the skin, so the first step in treating a pressure ulcer is to alleviate excess pressure. Using blankets or pillows can be helpful if you are lying down. Try to keep the wound site clean and dry.
Gently washing the area with mild soap and water is sufficient to help a Stage I sore, while saline or specific cleaner can be used for Stage II sores to remove loose, dead tissue. Avoid using hydrogen peroxide and iodine cleansers that could further damage the skin.
Recommended Reading: What To Eat With Stomach Ulcer
Caring For A Pressure Sore
Stage I or II sores will often heal if cared for carefully. Stage III and IV sores are harder to treat and may take a long time to heal. Here’s how to care for a pressure sore at home.
Relieve the pressure on the area.
- Use special pillows, foam cushions, booties, or mattress pads to reduce the pressure. Some pads are water- or air-filled to help support and cushion the area. What type of cushion you use depends on your wound and whether you are in bed or in a wheelchair. Talk with your health care provider about what choices would be best for you, including what shapes and types of material.
- Change positions often. If you are in a wheelchair, try to change your position every 15 minutes. If you are in bed, you should move or be moved about every 2 hours.
Care for the sore as directed by your provider. Keep the wound clean to prevent infection. Clean the sore every time you change a dressing.
Avoid further injury or friction.
- Powder your sheets lightly so your skin doesn’t rub on them in bed.
- Avoid slipping or sliding as you move positions. Try to avoid positions that put pressure on your sore.
- Care for healthy skin by keeping it clean and moisturized.
- Check your skin for pressure sores every day. Ask your caregiver or someone you trust to check areas you can’t see.
- If the pressure sore changes or a new one forms, tell your provider.
Take care of your health.
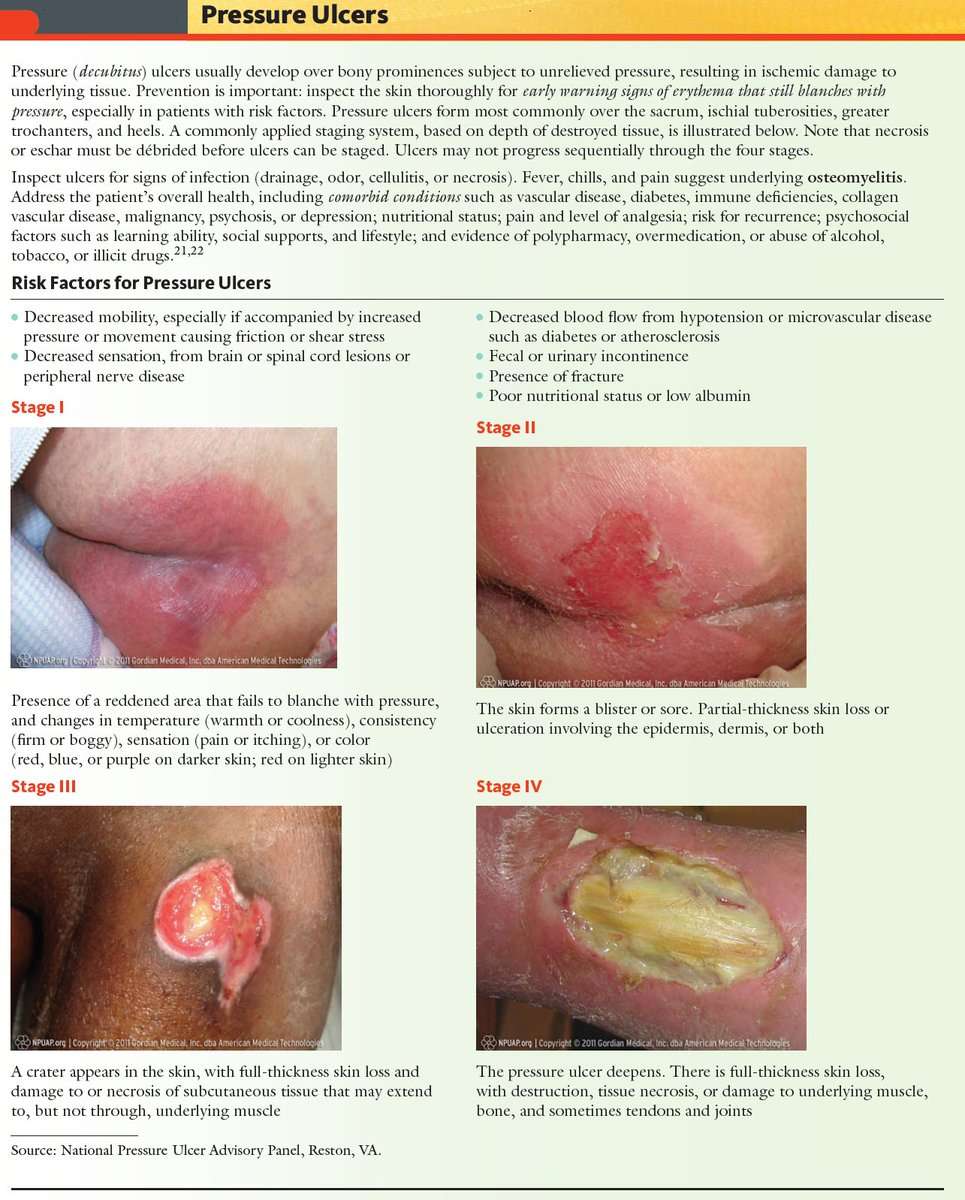
Appendix 1 Pressure Ulcer Grading
One of the most widely recognised systems for categorising pressure ulcers is that of the National Pressure Ulcer Advisory Panel . Their international classification recognises four categories or stages of pressure ulcer and two categories of unclassifiable pressure injury, in which wound depth and/or extent, or both, cannot be accurately determined unclassifiable pressure ulcers are generally severe and would be grouped clinically with Stage 3 or Stage 4 ulcers :
The two additional categories of unclassifiable wounds are:
- Unstageable/unclassified Obscured fullthickness skin and tissue loss: Fullthickness skin and tissue loss in which the extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar. If slough or eschar is removed, a Stage 3 or Stage 4 pressure injury will be revealed. Stable eschar on the heel or ischemic limb should not be softened or removed.
Read Also: Stool Test For Ulcerative Colitis